Chapter 46: Bowel Elimination
advertisement

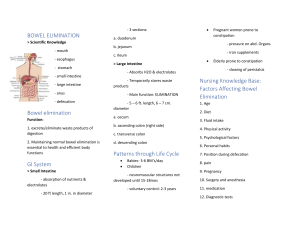
Chapter 46: Bowel Elimination Bonnie M. Wivell, MS, RN, CNS Scientific Knowledge Base Mouth Esophagus Digestion begins with mastication; saliva dilutes and softens food Peristalsis moves food bolus into the stomach Stomach Small intestine Stores food & liquid; mixes Duodenum, jejunum, and food, liquid and digestive ileum juices; moves food into small intestines Large intestine Anus The primary organ of bowel elimination Expels feces and flatus from the rectum Factors Affecting Bowel Elimination • Age – Infants: small stomach capacity; less secretion of digestive enzymes; rapid peristalsis; lack neuromuscular development so cannot control bowels – Older adults: arteriosclerosis which causes decreased mesenteric blood flow, decreasing absorption in small intestine; decrease in peristalsis; loose muscle tone in perineal floor and anal sphincter thus are at risk for incontinence; slowing nerve impulses in the anal region make older adults less aware of need to defecate leading to irregular BMs and risk of constipation Factors Affecting Bowel Elimination • Diet: fiber such as whole grains, fresh fruits and vegies • • • • • help flush the fats and waste products from the body with more efficiency; decreased fiber → increased risk of polyps; be aware of food intolerances Fluid intake: 6-8 glasses of noncaffeinated fluid daily; liquifies intestinal contents easing passage through colon Physical activity: promotes peristalsis Psychological factors: stress increases peristalsis resulting in diarrhea and gaseous distention; ulcerative colitis; IBS; gastric and duodenal ulcers; crohn’s disease Personal habits: fear of defecating away from home Position during defecation: squatting is the normal position Factors Affecting Bowel Elimination • Pain: hemorrhoids, rectal surgery, rectal fistulas • • • • and abd. surgery Pregnancy: increased pressure; slowing peristalsis in third trimester Surgery and Anesthesia: lows or stops peristalsis; paralytic ileus = direct manipulation of the bowel and lasts 24-48 hours Medications: laxatives and cathartics; laxative overuse can decrease muscle tone and can cause diarrhea which can result in dehydration and electrolyte imbalance; see Table 46-2 Diagnostic tests: bowel prep; barium Common Bowel Elimination Problems • Constipation – Causes: improper diet, reduced fluid intake, lack of exercise, and certain meds – A significant health hazard • Impaction – Causes: unrelieved constipation – Debilitated, confused, and unconscious more at risk – Continuous ooze of diarrhea is a suspect sign • Diarrhea – Causes: antibiotics via any route; enteral nutrition; food allergies or intolerance; surgeries or diagnostic testing of the lower GI tract; C. difficile; communicable food-borne pathogens Common Bowel Elimination Problems • Incontinence – Causes: physical conditions that impair anal sphincter function or control • Flatulence – Causes: certain foods; decreased intestinal motility – Can become severe enough to cause abd distention and severe sharp pain • Hemorrhoids = dilated, engorged veins; internal or external – Causes: straining with defecation; pregnancy; heart failure; chronic liver disease Bowel Diversions • Ostomies: Certain disease /conditions prevent normal passage of stool; temporary or permanent artificial opening in the abd wall; location determines consistency of stool – Loop colostomy: Usually done emergently; temporary; usually involves transverse colon; two openings through one stoma – stool and mucus; external supporting device usually removed in 7-10 days – End colostomy: one stoma formed from the proximal end of the bowel and distal portion of the GI tract removed or sewn closed (Hartman’s pouch); common in colorectal cancer and rectum is usually removed; temporary in surgery for diverticulitis – Double-barrel colostomy: bowel is surgically severed and two ends brought out onto the abd; proximal stoma functions and distal stoma is nonfunctioning Loop Colostomy Double-Barrel Colostomy Double-Barrel Colostomy End Colostomy Bowel Diversions Cont’d. – Alternative procedures • Ileoanal pouch: colon removed for tx of ulcerative colits or familial polyps; pouch is formed from distal end of small intestines and attached to anus; pouch acts as rectum so pt. is continent; has temporary ileostomy while healing • Kock continent ileostomy: consists of a reservoir constructed from small bowel and nipple valve which keeps contents of reservoir inside body; permits entry of external catheter to drain pouch • Macedo-Malone Antegrade Continence Enema (MACE); for improving continence in pts with neuropathic or structural abnormalities of the anal sphincter Ileoanal Pouch Anastomosis Kock Continent Ileostomy Care of the Patient With a Bowel Diversion • “Bagging” the ostomy • Assessing stoma and skin • Assessing stool output • New stoma vs. Old stoma • Patient education and counseling Psychological Considerations • • • • • Body image changes Face a variety of anxieties and concerns Must learn how to manage stoma Cope with conflicts of self-esteem and body image Can be concealed with clothing but pt. aware of its presence • Difficulty with intimacy/sexual relations • Foul odors, leakage, spills and inability to control or regulate passage of gas and stool is embarrassing • Ostomy support: – United Ostomy Association – National Foundation for Ileitis and Colitis Nursing Process and Bowel Elimination • Assessment – Nursing history (see Box 46-2) • • • • • • • • • • • • • • • Usual elimination pattern Usual stool characteristics Routines to promote normal elimination Use of artificial aids Presence/status of bowel diversions Changes in appetite Diet history Daily fluid intake History of surgery or illnesses of GI tract Medication history Emotional state History of exercise Pain or discomfort Social history Mobility and dexterity Nursing Process and Bowel Elimination – Physical assessment of the abdomen • Mouth: poor dentition, dentures, mouth sores • Abdomen: inspect, auscultate, palpate, percuss • Rectum: inspect – Inspection of fecal characteristics – Review of relevant test results • Fecal specimens: cannot mix feces with urine or water – Stool for occult blood (FOBT or guiac) see Box 46-3 – Fecal fat requires 3-5 days of collection – Ova & Parasites (O&P) • Labs: bilirubin, ALK, Amylase, CEA • Diagnostic Exams: KUB, endoscopy, colonoscopy, barium enema, barium swallow, US, MRI, CT scan (may require pre-procedure preparation) Nursing Diagnosis • Bowel incontinence • Constipation • Risk for constipation • Perceived constipation • Diarrhea • Toileting self-care deficit • Body image, disturbed Planning • Goals and outcomes – Client sets regular defecation habits – Client is able to list proper fluid and food intake needed to achieve bowel elimination – Client implements a regular exercise program – Client reports daily passage of soft, formed brown stool – Client doesn’t report any discomfort associated with defecation • Setting Priorities • Collaborative Care - WOCN Implementation • Health Promotion: establish routine – Promotion of normal defecation • Sitting position • Position on bedpan – see pg. 1196 • Privacy • Acute Care – – – – Meds Cathartics and laxatives Antidiarrheal agents Enemas Types of Enemas • Cleansing enemas – Tap water – Normal saline – Hypertonic solutions – Soapsuds • Oil Retention • Carminative – Mag, gylcerin and water; relieves gaseous distention • Medicated enemas – Kayexalate Implementation Cont’d. • Enema administration – “Enemas till clear” – See pages 1200-1202 • Digital removal of stool – last resort – Can cause irritation to the mucosa, bleeding and stimulation of vagus nerve • Inserting and maintaining a nasogastric tube NG Tubes • Levine or salem sump tubes are most common for • • • • • stomach decompression or lavage See pages 1204-1209 for insertion procedure Connected to intermittent suction (LIS) Air vent should NEVER be clamped, connected to suction or used for irrigation Not a sterile technique Care of pt. with NG – – – – Comfort Frequent mouth care/gargling Maintain patency of tube Turn client frequently to allow for adequate emptying Continuing and Restorative Care • Care of ostomies • Irriating a colostomy • Pouching ostomies (see pages 1211-1215) • Nutritional considerations with ostomies • Bowel training • Proper fluid and food intake • Regular exercise • Hemorrhoids • Skin integrity Evaluation • The effectiveness of care depends on how successful the client is in achieving goals and outcomes • Optimally the client will be able to have regular, pain-free defecation of soft-formed stools • It is necessary to ask questions so establishing a therapeutic relationship is VERY important • Nursing interventions may be altered if necessary