team preceptor model: transitions to
advertisement

TEAM PRECEPTOR MODEL:
TRANSITIONS TO
PROFESSIONAL DEVELOPMENT
Susan F. DePasquale, CGRN, MSN, CNS
St. James Healthcare
Sisters of Charity of Leavenworth Health System (SCLHS)
Butte, Montana
Objectives
Define Team Preceptor Model (TPM)
Recognize importance of TPM or “collaborative development” to
nursing role development
Identify new TPM processes and tools within SJH and SCLHS
Education Collaborative
Background:
emerging nursing roles
New evolving regulatory and professional standards of practice:
New grad training levels vary – associate / tech training and
transition programs, i.e. RN to BSN and BSN to MSN
Health reform & incentives for APRN role development - varying
pathways and levels, i.e. DNP
Clinical nursing role development (IP, OP, Triage & all levels of
nursing administration) - certification highly encouraged and
continuing competency mandatory most jurisdictions in U.S. and
internationally. Nurses at all levels are required to demonstrate a
learning plan, professional reflection and peer feedback.
Nursing state / national regulatory levels – increasing focus is on
transition to practice / continuing competency (novice to expert)
Background:
health reform & nursing
An expanding potpourri of new nursing pathways with
specific standards and best practice guidelines to support
role development in a milieu of widespread health care reform.
4
Background: choosing a
nursing pathway
Pathways & Standards of Practice:
Acute Care Clinical Specialties, Subspecialties (i.e. HIV/AIDS,
Addictive Behaviors, EOL Care…), Advanced Practice (multiple
pathways), Women’s / Children’s Health, Genetics, Research …
EBN (evidence-based nursing) standards are professionally
monitored and regulated at many levels
5
Background:
Team Preceptor Model
Team Preceptor Model (TPM) also termed “Collaborative
Preceptor Model” is well entrenched in the nursing literature and
more recently at a regulatory level
Is considered essential in any organization committed to:
collaborative practice
continuing competency
professional role development
high quality health care standards
6
Team Preceptorship:
why is it important?
TPM is important to nursing professional development because it
helps new nurses transition:
from theory into every day practice
from classroom or prior work group into new practice setting
(socialization)
into applied learning and internalizing a new role within a
professional health affiliate or organization
into learned values of their profession within nurturing and
supportive relationships – circle of support
7
Team Preceptorship: defined
When we talk about TPM we are referring to:
A one-to-one relationship between RN Preceptor(s) / Mentor(s)
and a new RN, new grad or nursing student (in a transition to
practice program)
Involvement of an intense, time-limited clinical experience to
facilitate learning (3 months – 1 year, depending on jurisdiction
and level of nursing experience)
Existing support by a clinical education department,
organizational policy and values / mission
Liaisons between a health organization and institutions of
learning; i.e. incorporates community nursing education for
student placements and initial phases of transition to practice
8
Benefit to patient care &
to a health organization
TPM is discussed in the literature in terms of:
Brief review of the literature
Patient Safety initiatives (EBN, Collaboration / Communication,
Team Culture of Safety … )
Nursing recruitment & retention
Nursing role development
Team satisfaction
Accreditation & funding (is a focus of ongoing surveys)
Others (based on experience)?
9
TPM: where are we at?
First Step: review of the literature
Description of collaborative development of the TPM
Methods of evaluating TPM and success - benchmarking:
Seattle - Virginia Mason Medical Center (VM) & Swedish
Healthcare (benchmarking)
Exempla and SCLHS Education Collaborative (system
hospitals and networking)
Montana – SJH staffing and collaborative model (selfreflection), local and regional networking, i.e. small
metropolitan / rural hospital programs and MNA transition to
practice state program
10
TPM: review of literature
The Future of Nursing: Focus on Education (2011). Institute of Medicine. Retrieved online
10/04/2011 at Future of Nursing.
National Council of State Boards of Nursing (2011). Transition to Practice. Retrieved online
09/28/2011 at NCSBN.
College of Registered Nurses of British Columbia (2011). Retrieved online 08/01/2011 at CRNBC
Practice Support
Preceptors Development and Support (2011). BC Academic Health Council: British Columbia,
Canada. Retrieved online 08/01/2011 at Preceptor Development
Cooper Brathwaite, Angela and Lemonde, Manon (2011). Team Preceptorship Model: A
Solution for Students’ Clinical Experience. Toronto, Canada. ISRN Nursing: Vol. 2011, Article ID
530357.
Royal Children’s Hospital (2011). RCH Nursing Preceptorship Model. Melbourne, Australia.
Transition into Practice – A Proposal for a Pilot Study in Ohio. Retrieved online 09/28/2011 at
Ohio Pilot Transition to Practice.
11
TPM: review of literature
Joint Commission (2011). Health Care at the Crossroads: Strategies for Addressing the Evolving
Nursing Crisis.
Warshawsky, N.E. and Sullivan-Havens, D. (2010). Global Use of the Practice Environment
Scale of the Nursing Work Index. Nursing Research: 2010.
Spector, Nancy (2009). A Transition to Practice Regulatory Model: Changing the Nursing
Paradigm. Dean’s Notes: Vol. 31, No. 2; Nov/Dec 2009.
Beecroft, P., McClure-Hernandez, A., Reid, D. (2008).
Team Preceptorships: A New Approach for Precepting New Nurses. Journal for Nurses in Staff
Development: July/Aug. 2008: Vol. 24, No. 4; p. 143-148.
Bolten Health Trust (2008). Policy and Frameworks for the Implementation of Preceptorship
for AHPs, HCSs, Nurses, Assistant Practitioners and Support Workers: London, United
Kingdom.
NCSBN’s Transition to Practice Model: A Multi-Site Study Comparing Patient Outcomes (2003).
Retrieved online 10/04/2011 at Transition To Practice International Study
Health Care Provider Preceptor Training Program: Model Curriculum (2003). Chancellors
Office California Community Colleges: Sacramento California
Queensland Health Preceptor Program for Transition Support (2001). Queensland Nursing
Council: Australia
12
TPM: collaborative
development
TPM is a synergistic and dynamic process, involving:
an innovative model based on the premise of collaborative
mentoring - the conceptual framework
nurses working together with several team members where each
mutually coach and facilitates each others personal and
professional growth - to promote a spirit of team
each individual in the TPM being recognized for unique
experiences, skills, and knowledge that he or she brings to
another’s learning experience - individualized and inclusive of
diversity and creativity
13
TPM: collaborative
development
Each member of the health team participates in the following
during the course of a preceptorship:
a direct or supportive role (example: orientation to unit)
coaches the new nurse in dynamic processes that support the
acquisition of new skills, interactions, and activities leading to
professional growth and development (example: documenting a
learning plan and peer feedback, professional practice support)
models a team approach that fosters a reciprocal relationship
between all stakeholders of the health team or collaborative
(example: standardization of learning tools; includes education,
leadership, interdisciplinary and community liaisons)
14
TPM: methods of
evaluating
Actual Study Analysis (2011) – Framework:
Community Health Nurse Preceptor / Student Group
Data collected - using a focus group format to enhance
information recall and robust data
An interview guide was created to help in facilitating two focus
groups – separate interview questions specifically for students
and for preceptors
Focus Groups interviewed at 12 weeks of placement; included 9
students and 14 preceptors
15
TPM: methods of
evaluating
Actual Study Analysis (2011) – Evaluation Points:
Support for preceptors and students
Collaboration among team members
Good communication among team members
Feeling overworked for preceptors (delay in work flow) and for
students (perception of delay in work)
Accessibility of preceptors for students
Expertise of preceptors for students
16
TPM: Methods of
evaluating
Actual Study Analysis (2011) – Findings:
Preceptors and students faced different challenges during
implementation of the TPM
Preceptors felt overworked and students perceived the delay in
workflow
These results have implications for clinical practice
Opportunities existed for participatory planning, i.e. student’s
learning from one or more preceptors (not necessarily a nurse) to
develop competencies
17
TPM: methods of
evaluating
About Feedback:
“You identify in your learning plan that your preceptor is there to
highlight learning experiences for you that correspond with your
learning plan, to help you accomplish your goals. For me, it was a
very effective approach”.
Clinical Study Team Preceptorship Model: A Solution for Students’
Clinical Experience (2011).
18
TPM: methods of
evaluating
Benchmarking Other’s Successes:
VM & Swedish Models – Shared Leadership, Unit Practice
Councils, Team Projects / Project Reports, Professional
Recognition
SCLHS Model – is an Education Collaborative that engages all
sister hospital sites; the sharing of standard work to develop:
Team Engagement – i.e. shared leadership councils
Evaluation Method – i.e. nursing economics, nursing quality
Evidence Based Learning (to promote a continuous learning
environment and culture of safety) – i.e. TEAM STEPPS,
shared teaching tools and resources
Professional Recognition of all team members at varying
levels of experience and learning plans
To help identify stakeholders, nursing and non-nursing – i.e.
Aspiration Risk Lean Project (interdisciplinary team)
19
SJH: what’s our team
model?
A few models were reviewed before visioning our own:
20
SJH: an evolving team model
Red = New Structures
Green = New Language (theory)
TEAM PRECEPTOR MODEL
SCLHS Education Collaborative
The Placement Coordinator – role & new tools, i.e.
Team Preceptor
Model:
Novice ToPractice
Expert
motivational interviewing, change models, etc… [HR
and Staffing share this role]
EP Role with Intermediate to Advanced RN:
o Initial Timeframe: role begins ≥ 1 year
o Goals: Advanced/complex skills validation,
Professional Plan & Development
o Collaborative Network: NP, LT, ED
o Tools: Professional Planner, Skills Lab &
Validation, Preceptor Collaborative, Nursing
Research, Peer-To-Peer Feedback
Lessons Learned:
EP roles often start sooner and
can cross over, i.e. charge duty,
quality, or others and this can be
a bridge or a detriment
depending on staffing and
preceptorship needs
CLINICAL
EDUCATOR
(ED)
EXPERT
PRECEPTOR
(EP)
LT Role with Novice to Expert RN:
o Initial Timeframe: role begins ≤ 3 months
o Goal: Socialization to organization / dept.,
HR (compliance), Staff Satisfaction,
Professional Plan Development
o Collaborative Network: N, NP, EP, ED (& HR)
o Tools: RN Job Description, Orientation Packet,
Skills Checklist, Peer-to-Peer Feedback Forms,
CEU Record & Professional Planner
ED Primary Role for the Novice to Expert RN:
o Initial Timeframe: role begins ≤ 3 months
o Goals: Socialization to organization / department,
Skills Validation (basic competencies), Preceptor
Role & Agreement, Professional Plan Development,
Peer-To-Peer Feedback
Lessons Learned:
o Collaborative Network: N, NP, EP, LT
is interdisciplinary
o Tools: Professional Planner, Skills Checklist,
Skills Lab & Validation, Online Learning,
Dept. Guidelines / Pathways, Nursing Protocol
NOVICE
(N)
NOVICE
PRECEPTOR
(NP)
LEADERSHIP
TEAM
(LT)
Lessons Learned: SJH leadership
wears “many hats”; SCLHS
standardization and transparency
of information is purported to
help support LT participation
Exempla – Culture of Safety, LEAN, EPIC, New Leadership (Councils)21
National Board of Nursing – White Paper (Joint Commission) “Future of Nursing”
Lessons Learned:
Tools used is part of an evolving
process within SCLHS and new
changes affecting standardization,
i.e. electronic portfolio
NP Role with Novice RN:
o Initial Timeframe: role begins ≤ 3 months
o Goals: Socialization to organization / dept., Skills
Validation (novice - intermediate skills),
Professional Plan Development
o Collaborative Network: N, EP, LT, ED
o Tools: Professional Planner, Skills Checklist,
Skills Lab, Online Learning, Nursing Protocol,
Peer-to-Peer Feedback Forms
Lessons Learned: TPM includes assumptions re:
NP role that we approach more cautiously; i.e.
NP educational curriculum and preparation?
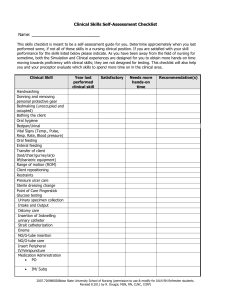
SJH: professional planner
& feedback tools
SJH Model –
Includes all levels of nursing experience
starts with the nurse performing a self assessment and forming a
professional plan
utilizes peer feedback to support reflection, identify and meet
practice goals, a performance evaluation (starts with milestone
meetings during orientation) and as part of a growing CV
SCLHS Model – pending (in early formative stages, goal to standardize
across the system)
Benchmarking – Shared Leadership and Professional Recognition
Program (PRP), i.e. magnet hospitals utilize a career ladder format that
includes a standard learning planner / continuing competency journal
22
SCLHS: evaluation tools
Exempla Collaborative – shared the Practice Environment Scale of
the Nursing Work Index (4 score); national measure for associate
engagement adopted from the “striving to be heard” study
TOPIC
QUESTION NO.
Nurse Participation in Hospital Affairs
5, 6, 11, 15, 17, 21, 23, 27, 28
Nursing Foundations for Quality of Care
4, 14, 18, 19, 22, 25, 26, 29, 30, 31
Nurse Manager Ability, Leadership, and Support of Nurses
3, 7, 10, 13, 20
Staffing and Resource Adequacy
1, 8, 9, 12
Collegial Nurse-Physician Relations
2, 16, 24
SCLHS – survey monkeys, i.e. Press Ganey, Culture of Safety
Surveys, etc …
Can you think of any others? How do we evaluate our education
for nursing and all associates?
23
Measuring engagement:
practice environment scale
Examples of questions (Scale 1 – 4)
Career development / clinical ladder opportunity
Active staff development or continuing education program for
nurses
Praise and recognition of job well done
Enough time and opp0rtunity to discuss patient care problems
with other nurses
Collaboration (joint practice) between physicians and nurses.
{1 = strongly agree, 2 = agree, 3 = disagree, 4 = strongly disagree}
24
Recognition moment
SJH Nursing Preceptors
SJH Nursing Leadership and Education Collaborative
SCLHS Education Collaborative
Silver Bow and Montana (a rich regional body of nursing
collaboration and knowledge sharing)
Nationally and Internationally
25
Finally ~
Thanks for listening!
26