Rutchik
advertisement

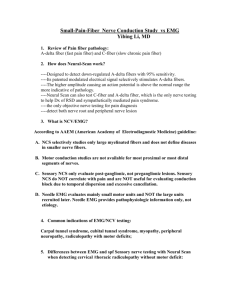
Electrodiagnosis in the management and treatment of cervical and lumbar spine disorders Jonathan S. Rutchik, MD, MPH NEUROLOGY, ENVIRONMENTAL AND OCCUPATIONAL MEDICINE ASSOCIATES 20 Sunnyside Avenue, Suite A-321 Mill Valley, CA 94941, USA TEL: 415-381-3133 FAX: 415-381-3131 jsrutch@neoma.com www.neoma.com OUTLINE • Radiculopathy; epidemiology and EMG • What is an EMG/ NCV? – What is an F wave; an H reflex? • What is the relevant anatomy? • What are the indications in patients with suspected cervical or lumbar radiculopathy? • What are the relevant treatment guidelines? – ACOEM, ODG, AANEM, AAN, ETC • Thoracic outlet syndrome • Interpretation of Data JS Rutchik, MD, MPH www.neoma.com CERVICAL RADICULOPATHY AND EMG • Age adjusted annual incidence 83.2/ 100,000 – 202.94 (50 and 54), <= CTS, <50% of stroke. • Recurrence in 31.7%. 26% undergo surgery • False positive rate (MRI) 20 - 50% with age. • Electrodiagnostic testing of paraspinal and limb muscles is 50 years old. • EMG complements MRI with its ability to localize a lesion and assess functionality of the nerve. • False negative studies: 50-71% sensitive, 6585% specific. JS Rutchik, MD, MPH www.neoma.com EMG/NCV: TWO PARTS “mild shocks and thin needles” • Nerve conduction velocity: Electrical tests of the motor and sensory nerve cables – Conduction velocity (MYELIN) – Distal latency (MYELIN) – Amplitude at recording electrode (AXON) • Electromyography: Needle placed in muscle – – – – Spontanous activity (NERVE INJURY) Recruitment (POWER) Location and Chronicity of injury Neuromuscular junction (N/A) JS Rutchik, MD, MPH www.neoma.com NERVE CONDUCTION STUDIES • Motor studies • Sensory studies • Late responses (F waves) that assess the proximal motor root • H reflexes that assess the sensory afferent and motor effect reflex loop of S1 (*C7/C8) JS Rutchik, MD, MPH www.neoma.com MOTOR STUDIES • Motor nerve test: – Supermaximal stimulation. – Distal latency, Amplitude and Nerve Conduction Velocity • Upper Extremity: – Median, Ulnar, Radial • Lower Extremity: – Peroneal, Tibial JS Rutchik, MD, MPH www.neoma.com F waves • Motor F wave studies proximal roots: – Antidromic motor to the anterior horn of the spinal cord; orthodromically to the muscle. • Pure motor test. • A prolonged asymmetric F waves suggest a proximal root lesion. • Clinical application best for plexopathy. – Quite prolonged in demyelination, AIDP, mild prolongation in axonal injury. • Less sensitive than EMG for radiculopathy since only short segment of nerve is demyelinated in radiculopathy. JS Rutchik, MD, MPH www.neoma.com SENSORY STUDIES • Sensory nerve testing: – Submaximal stimulation – Distal latency, amplitudes and nerve conduction velocity • Upper Extremity: – Median, Ulnar, Radial • Lower Extremity: – Superficial peroneal, sural JS Rutchik, MD, MPH www.neoma.com Sensory studies • Sensory slowing supports a localization distal to the Dorsal Root Ganglion • Sensory slowing in itself suggests either two processes or NOT a pure radiculopathy. • Pearl: recording at thumb assesses upper trunk and C6, D1 is C7 and middle trunk. JS Rutchik, MD, MPH www.neoma.com H REFLEX • • • • • Reflex loop: Orthodromic sensory and motor Utilized to assess for radiculopathy of S1, *C6/7 S1; Popliteal fossa, record in MG C6/7; Median nerve at wrist, record at FCR Unilateral delay, absent suggests tibial, sciatic, sacral plexus, cord, S1 motor or sensory roots. – Once abnormal, may not normalize; limited for patient with prior – Often absent in polyneuropathy or > 60. JS Rutchik, MD, MPH www.neoma.com NEEDLE EMG • Screening cervical and lumbo- sacral myotomes – PARASPINAL, INDIVIDUAL MUSCLES • Anatomy • Needle insertion near motor point – INSERTIONAL ACTIVITY AT REST – RECRUITMENT TO FULL CONTRACTION – SINGLE MOTOR UNIT ASSESSMENT JS Rutchik, MD, MPH www.neoma.com Why is EMG helpful? • Differentiates Nerve roots, dermatomes, both: – C5 v C6 or Median v. Ulnar, or C8 v median • Chronicity of problem: – Acute (activity at rest) versus – Chronic (abnormal wave forms in isolated muscle fiber testing) • F wave assesses proximal root only • Axonopathy confirmed with needle • Severity/ improvement; distal to proximal JS Rutchik, MD, MPH www.neoma.com INDICATIONS FOR EMG/ NCV • Pain • Paresthesia radiating to a nerve root distribution • Associated sensory distrubance +/• Parspinal muscle spasm • Motor dysfunction +/• Exam findings in specific sensory dermatome or motor myotome JS Rutchik, MD, MPH www.neoma.com AANEM* and EMG American Academy of Neuromuscular and Electrodiagnostic MEdicine • C radiculopathy is listed as a possible differential diagnosis and “may be useful” in patient with neck, shoulder or arm pain, numbness, altered sensation (e.g., pins and needles), weakness, cramps, fasciculations, muscle atrophy or hypertrophy (focal or diffuse) • L radic is listed as a possible differential diagnosis and “may be useful” in patient with back, hip or leg pain, numbness, altered sensation (i.e., pins and needles), weakness, cramps, fasciculations, muscle atrophy or hypertrophy. JS Rutchik, MD, MPH www.neoma.com AANEM, C spine and EMG Muscle Nerve 22: supp 8, S209-211, 1999 • Guideline: • Needle: >= one muscle innervated by each spinal root, cervical 5, 6, 7, 8, and thoracic 1 in asymptomatic limb. • Cervical paraspinals at 1 or more levels should be examined – Not in prior posterior approach of laminectomy. • >= one motor and one sensory NCV study to determine if concomitant polyneuropathy or nerve entrapment exists. • Median and ulnar nerves M and S studies; if symptoms suggest CTS or ulnar neuropathy. • NCV abnormal, or suggestion of polyneuropathy, NCV of other ipsilateral and contralateral nerves to define the cause of any abnormalities. JS Rutchik, MD, MPH www.neoma.com AANEM, C spine and EMG Muscle Nerve 22: supp 8, S209-211, 1999 • Option: • If needle abnormal, one or more contralateral muscles to exclude bilateral radiculopathy • Differentiate between radiculopathy and polyneuropathy, motor neuron disease, spinal cord lesion, or other neuromuscular disorders. • Median and ulnar F wave studies for suspected C8 or T1 radiculopathy; compare with contralateral side. • Perform H reflects of the FCR to assist in identifying pathology of the cervical 6 and 7 nerve root. JS Rutchik, MD, MPH www.neoma.com EMG and Radiculopathy • Indicated often to rule out other conditions • Upper extremity nerve entrapments, brachial plexopathy, thoracic outlet syndrome, hereditary or acquired neuropathies • Lower extremity entrapments, cauda equina syndrome, conus medullaris, spinal cord conditions, polyneuropathy • These disorders are important considerations in the electrodiagnostic evaluation of patients with a suspected radiculopathy. JS Rutchik, MD, MPH www.neoma.com ACOEM, EMG and Neck Pain • When the neurologic examination is less clear, however, further physiologic evidence of nerve dysfunction can be obtained before ordering an imaging study. Electromyography (EMG), and nerve conduction velocities (NCV), including H-reflex tests, may help identify subtle focal neurologic dysfunction in patients with neck or arm symptoms, or both, lasting more than three or four weeks. • Absence of progression motor weakness in 4-6 weeks. (Table 8-3) • Clarify nerve root dysfunction preoperative or preepidural Not if history, physical exam and imaging consistent (D) (Table 8-8) JS Rutchik, MD, MPH www.neoma.com ACOEM, EMG and Lower Back Pain • EMG may assist in identifying/ defining low back pathology such as disc protrusion, cauda equina, spinal stenosis and post laminectomy syndrome (Table 12-7).False-positive rate is 30% for imaging studies > 30 w/o sx, risk of dx confusion is great. • Needle EMG and H reflexes to clarify nerve root dysfunction (C) (Table 12-8) – Not rec for clinically obvious radiculopathy (D) JS Rutchik, MD, MPH www.neoma.com Official Disability Guidelines, EMG and Cervical spine • “Not necessary for 4-6 weeks. Not necessary for the diagnosis of intervertebral disk disease with radiculopathy” • Usefulness in differentiating neuritis, neuropathy, or muscle abnormalities from radicular neuropathy and for cases where the etiology of the pain is not clear. • Cites AANEM guidelines. • Issue of requirement of positive EMG for diskectomy or laminectomy. Washington State • Recommended (needle, not surface) as an option in selected cases. • Odd mention of no indication for F waves or NCV (only in CTS?) but indication for H reflexes. JS Rutchik, MD, MPH www.neoma.com Official Disability Guidelines, EMG and Lumbar spine • May be useful to obtain unequivocal evidence of radiculopathy, after 1-month conservative therapy, “but not necessary if radiculopathy is already clinically obvious” • EMG’s may be required by the AMA Guides for an impairment rating of radiculopathy. – (Note: Needle EMG and H-reflex tests are recommended, but Surface EMG and F-wave tests are not very specific and therefore are not recommended JS Rutchik, MD, MPH www.neoma.com Thoracic Outlet Syndrome/ Brachial Lumbosacral plexopathy • • • • • Controversy: true neurogenic rare Sensory and motor loss in C8-T1 distribution Fibrous band over T1. Weakness in thenar and hypothenar, atrophy. Protocol includes antebrachial studies (SNAP) to assess lower and upper truck. – Ulnar and medial antebrachial SNAP abn, median SNAP normal. Median MUAP reduced > ulnar MUAP. • Collision studies? • Thorough needle examination JS Rutchik, MD, MPH www.neoma.com