External Rspiration, Gas Transport, & Internal Respiration
advertisement
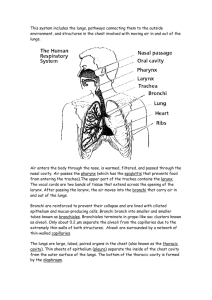
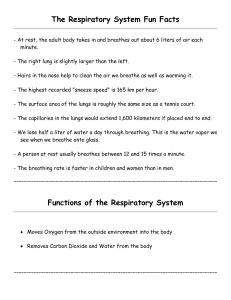
Respiratory Physiology (448-460) Main function of the respiratory system is to supply body with oxygen and remove of carbon dioxide There are 4 parts of respiration: o Pulmonary ventilation (breathing)- air moving into and out of the lungs so air in the alveolar sacs is refreshed o External respiration- gas exchange between blood in the pulmonary capillaries and the alveoli (blood and the external environment) o Respiratory gas transport- transport of oxygen and carbon dioxide to and from the lungs and body via the bloodstream o Internal respiration- gas exchange between the blood and cells in the body due to the occurrence of cellular respiration (process of breaking down glucose into ATP which requires oxygen) Mechanics of Breathing Mechanical process that depends on changes of volume in the thoracic (chest) cavity o Change in volume leads to a change in pressure which affects the flow of gases to equalize pressure o If large volume, the gas molecule inside the container are spread apart… low pressure o If volume is decreased, gas molecules are closer together and have more collisions with the walls of the container thus inc. pressure Inspiration (air flowing into the lungs) Diaphragms and external intercostals (muscles attached to ribs) contract inc size of thoracic cavity o Diaphragm is dome-shaped, when it contracts it moves inferiorly and flattens out inc. the height (superior-inferior direction) of the thoracic cavity Massages the abdominal organs o External thoracic muscles contract which lifts the rib superiorly and pushes the sternum anteriorly which inc the thoracic cavity in the anteroposterior and lateral directions The lungs remain close to the walls of the chest cavity b/c the visceral and parietal pleura secrete a fluid with a surface tension (fluid “sticks” together like water droplets) causes the lungs to expand with the thoracic cavity (inc. intrapulmonary volume) b/c the volume is larger pressure dec. to below atmospheric pressure and air rushes into the lungs to equalize the pressure inside and outside the lungs Expiration (air flows out of the lungs) Passive process that depends on the elasticity of the lungs more than muscle contraction As muscles relax the diaphragm rises superiorly, the intercostals drop inferiorly, and the sternum depresses posteriorly as the muscles return to their resting locations o Causes thoracic volume and intrapulmonary volume to decrease inc pressure in the lungs o When pressure in the lungs becomes higher than the atmospheric pressure gases leave the lungs to equalize the pressures If respiratory passages are narrowed by spasms of the bronchioles (asthma attack) of clogged with mucus of fluid (pneumonia or bronchitis) expiration cannot happen passively the internal intercostals and abdominal muscles must contract to decrease thoracic cavity volume and squeeze the abdominal organs superiorly against the diaphragm Pressure in the pleural space is always negative prevents lung from collapsing *Atelectasis- a lung collapse (lung recoil), the lungs cannot expand and cannot perform ventilation; result of injury to chest wall (alveoli become compressed and can’t expand) *Pneumothorax- visceral pleura is punctured allowing air to enter the pleural space decreasing the bond between the visceral and parietal pleura causing the lung to “detach” from the thoracic wall Nonrespiratory Air Movements (see table 13.1) Situations other than breathing that move air into or out of lungs and may change normal respiratory rhythm (can be reflexive or voluntary) o Cough, sneeze, crying, laughing, hiccups, yawn Respiratory Volumes and Capacities (do not need to memorize specific # values!) many factors affect respiratory capacity: age, gender, size, condition normal quiet breathing moves ~500 ml of air (1 pint) into and out of lungs/breath = tidal volume more air can be forcibly inhaled than during normal breathing ~2100 — 3200 ml= inspiratory reserve volume more air can be forcibly exhaled than during normal breathing ~1700 ml = expiratory reserve volume after forcible exhalation about 1200 ml of air remains in lungs and cannot be voluntarily exhaled = residual volume o important because allows gas exchange to occur between breathes (bc blood is continuously flowing) o help keep alveoli inflated total amount of exchangeable air = vital capacity o sum or TV+IRV+ERV (does not include residual) total lung capacity ~6000 ml some inhaled air never reaches the alveoli b/c it stays in a windpipe (trachea, bronchi, bronchioles), called dead space volume o ~150 ml stays in respiratory tract during normal breathing and 350 ml is used for gas exchange ***exhaled air contains carbon dioxide and other gases that were inhaled like oxygen*** Volumes are measured with a spirometer o Useful in determining the loss of respiratory function or to track the course of a respiratory disease Pneumonia (fluid in lungs) inspiration blocked causing lower IRV and VC Emphysema (lungs lose elasticity) ERV is lower and residual volume is higher because the lungs cannot expel air Respiratory Sounds Can hear bronchial sounds as air rushes into or out of the trachea and bronchi Can hear vesicular breathing sounds as alveoli fill with air *impaired lung tissue, mucus, or pus accumulation can create abnormal sounds such as crackles (like bubbling liquid) or wheezing (whistling) External Rspiration, Gas Transport, & Internal Respiration All gas exchanges occur due to the laws of diffusion External respiration Dark red blood in pulmonary circuit (from pulmonary arteries) collects oxygen by binding to hemoglobin which makes oxygenated blood bright red at the same rate that CO 2 is diffused into the alveoli to be exhaled o Occurs because O2 concentration in blood is lower than in the alveoli since O2 is used by body cells o CO2 concentration is higher in blood than in the alveoli because cells create CO 2 during cell respiration and it diffuses into the plasma of blood Gas Transport in Blood Oxygen carried in blood in 2 ways: o Attaches to hemoglobin in red blood cells makes oxyhemoglobin (how most O2 is carried) o Dissolved in blood plasma, the liquid part of blood (very little is carried this way) Carbon dioxide is transported in blood as bicarbonate ions (HCO3—) necessary to maintain body;s normal pH ~ 7.4 o RBCs turn CO2 into HCO3— then it diffuses into the plasma *** MOST CO2 IS CARRIED IN BLOOD PLASMA NOT IN RBCs!*** o A little CO2 is carried in RBC by binding to hemoglobin but the binding site for CO 2 is different than oxygen’s binding site therefore CO2 presence in RBC does not impact O2 transport Before CO2 diffuses out of blood, it must be changed from HCO3— into CO2 … HCO3— enters RBC RBC adds H+ makes H2CO3 (carbonic acid) breaks down into H2O and CO2 Process must occur in RBC because the presence of carbonic anhydrase speeds up the reaction (is a catalase) *hypoxia- a condition in which the body is not receiving enough oxygen; causes skin to have a bluish tint (if can’t see in skin can see in nailbeds); can result from anemia (having too little RBCs, pulmonary disease, or impaired blood circulation) *Carbon monoxide poisoning- is a specific type of hypoxia, occurs when CO (an odorless, colorless gas) is inhaled and competes with oxygen for the same binding sites on hemoglobin. Because, CO bonds to hemoglobin more readily than oxygen, the body does not get enough oxygen. Carbon monoxide is produced when objects are burned and become only partially oxidized (released in exhaust fumes of cars, during fires, from burning coal, etc.). People with CO poisoning don’t show typical hypoxia signs. Their skin tone looks blush (b/c CO binding to Hb produced the same red color that is seen when oxygen binds to Hb), they get headaches, and appear confused. Internal respiration Process in which oxygen is unloaded from blood and carbon dioxide is added to blood Reverse processes as what occurs in the lungs happen here because of molecule concentrations Control of Respiration Done in 1 ways: 1. Neural control 2. Non-neural factors that affect respiration Neural Regulation: Setting the Basic Rhythm