Therapy of CHF, Outline Slides
advertisement
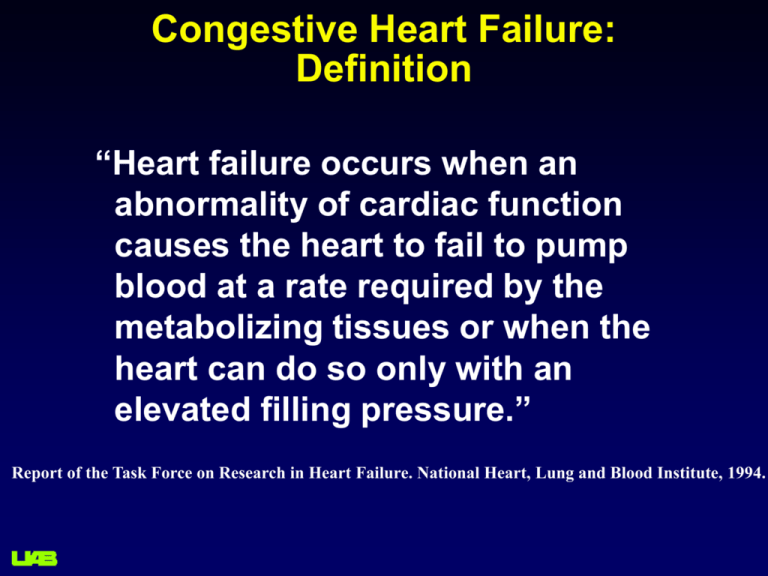
Congestive Heart Failure: Definition “Heart failure occurs when an abnormality of cardiac function causes the heart to fail to pump blood at a rate required by the metabolizing tissues or when the heart can do so only with an elevated filling pressure.” Report of the Task Force on Research in Heart Failure. National Heart, Lung and Blood Institute, 1994. Acute Exacerbations Contribute to the Progression of the Disease Clinical Status With each event, hemodynamic alterations/myocardial injury contribute to progressive ventricular dysfunction Acute event Heart failure progression may be accelerated by the aggressive therapies initiated during hospitalization Time Jain P et al. Am Heart J. 2003;145:S3-S17. Congestive Heart Failure Congestion (as measured by increased intracardiac end diastolic pressures) Symptoms and Survival Physiological Premise of IHM Guided Care (1) Heart Failure Event Symptoms Pressure Changes -21 -14 -7 Proactive 0 Days Reactive Physiological Premise of IHM Guided Care (2) Medical Intervention Averted Heart Failure Event Pressure Changes -21 -14 Proactive -7 0 Days Chronicle® Implantable Hemodynamic Monitor (Medtronic, Inc.) Implantable Hemodynamic Monitor (IHM), RV lead 4+ year battery life (SVO-Lithium) Internal memory 512k RAM, 96k ROM Programable “resolution” from 2 sec - 52 min (mean, range) and trend data storage from 3.5 hr – 3 months Parameters Measured/Calculated/Stored Include: PA systolic (RV systolic) pressure PA diastolic (ePAD from RV pressure at +dP/dtmax) RV diastolic pressure (RA) Maximum positive and negative RV dP/dt (calculated) Heart Rate, Temperature, Patient Activity Pressure and Electrogram Waveforms Programmable and Patient Initiated Trigger for high-res. data store Additional System Components: External Pressure Reference (EPR) – size of “pager” Telemetry data download-upload (office/phone) Chronicle web site data review via internet browser Chronicle® Implantable Hemodynamic Monitor (Medtronic, Inc.) 25g, 14cc Chronicle IHM - Lead Positioning Pressure Sensor Capsule Chronicle Pressure Measurements EGM 1 = RVDP at QRS detection 2 2 = RVSP at peak of waveform 3 3 = ePAD at maximal dP/dt 1 RVP dP/dt Accuracy of Intracardiac Pressure Monitoring 20 40 60 80 100 120 Swan-Ganz RV Systolic Pressure (mmHg) 80 40 60 r = 0.84 0 20 40 60 Chronicle PAD Pressure (mmHg) r = 0.87 20 60 40 20 0 ePAD 0 Chronicle RV Diastolic Pressure (mmHg) r = 0.95 80 100 120 Diastolic 0 Chronicle RV Systolic Pressure (mmHg) Systolic 0 20 40 60 Swan-Ganz RV Diastolic Pressure (mmHg) 0 20 40 60 80 Swan-Ganz PAD Pressure (mmHg) N = 32 patients, 217 measurements at rest (supine, siting), Valsalva, exercise) Magalski, A, et al. Continuous Ambulatory Right Heart Pressure Measurements with an Implantable Hemodynamic Monitor: a Multi-center, 12 Month Follow-up Study of Patients with Chronic Heart Failure, J Card Failure. 2002;8(2):63-70. 120 r = 0.94 20 40 60 80 100 120 6 Months 0 20 40 60 80 100 120 Swan-Ganz RV Systolic Pressure (mmHg) 100 120 80 60 40 20 0 20 40 60 80 100 120 Swan-Ganz RV Systolic Pressure (mmHg) Chronicle RV Systolic Pressure (mmHg) Swan-Ganz RV Systolic Pressure (mmHg) 0 Chronicle RV Systolic Pressure (mmHg) 100 12 Months 100 120 80 r = 0.94 80 60 60 40 40 20 r = 0.95 20 60 40 20 0 0 3 Months 0 r = 0.96 80 100 120 Implant 0 Chronicle RV Systolic Pressure (mmHg) Chronicle RV Systolic Pressure (mmHg) Chronicle Phase I Validation 0 20 40 60 80 100 120 Swan-Ganz RV Systolic Pressure (mmHg) Magalsky A. et al., J Card Failure 2002;vol.8 n.2:63-70 Chronicle System & Information Flow Chronicle IHM Remote Monitor Secure Network Clinician Access Chronicle IHM System Web Site 94th percentile Median 6th percentile Bourge, RC et al. J Am Coll Cardiol 2008;51:1073-9 The Implantable Hemodynamic Monitor: Potential Clinical Applications Improve our understanding of the hemodynamic alterations that occur with heart failure and the hemodynamic response to therapy Allow more precise titration and tailoring of heart failure and pulmonary vascular disease (PH) therapy Provide “early warning” of hemodynamic deterioration Aid in the diagnosis of symptomatic events in the outpatient setting (home or clinic) Provide method by which to develop, refine, and optimize the use of chronic hemodynamic data for longterm patient management Possibly affect the intermediate and long term morbidity and mortality in patients with heart failure UAB E011 68y/o male DM, IHD, EF 45%, severe diastolic dysfunction, renal insufficiency, morbidly obese; peripheral neuropathy, LE venous insufficiency, intermittently non-compliant with salt and fluid restriction. CHF/IHD Rx: torsemide 200 bid metolazone 5mg bid spironolactone 50 bid atenolol 25 qDay C/o progressive weight gain (19lbs) over prior weeks, orthopnea, PND, despite massive oral diuretic use. Review of Chronicle IHM pressures revealed only modestly increased RV pressures and no significant change in serum bNP. Admitted from clinic with severe edema for IV therapy. Heart Rate Heart Rate UAB E011 After admission, treated with IV diuretics, IV nesiritide, and strict salt and fluid restriction with a 16kg diuresis. With this, he had a significant improvement in his symptoms and a modest reduction in his daytime filling pressures. Serum BNP: 99 119 75 112 100 126 54 UAB E011 Chronicle Nightly Minimum Pressures Retrospective review of nightly minimums from Chronicle: Note: On April 17th, metolazone dose was increased to 5mg bid due to 12 lb weight gain. After admission, treated with IV diuretics, IV nesiritide, and strict salt and fluid restriction with a 16kg diuresis. With this, he had a significant improvement in his symptoms and a modest reduction in his daytime filling pressures. 54 126 75 112 Serum BNP 106 Clinical Explanation ? The Implantable Hemodynamic Monitor: Potential Clinical Applications Improve our understanding of the hemodynamic alterations that occur with heart failure and the hemodynamic response to therapy Allow more precise titration and tailoring of heart failure and pulmonary vascular disease (PH) therapy Provide “early warning” of hemodynamic deterioration Aid in the diagnosis of symptomatic events in the outpatient setting (home or clinic) Provide method by which to develop, refine, and optimize the use of chronic hemodynamic data for longterm patient management Possibly affect the intermediate and long term morbidity and mortality in patients with heart failure 81yo female – BMI 39.1, BP 108/68, HR 80; Hx of HF (2007), HTN (1995), PAH and Rt renal artery aneurysm (2006), and diastolic dysfunction CHF (Jan 2007), hypercholesterolemia, stress incontinence, Atrial Fibrillation; h/o renal dysfunction when treated with loop diuretics; Referred to UAB for therapy of pulmonary hypertension, class III+ on presentation. Study device implanted 8/28/07 Baseline meds (daily) – Carvedilol (50mg), Coumadin (2.5mg), Atorvastatin (20mg), Triamterene (50mg), Hydrochlorothiazide (50mg) No changes to medical regimen - patient treated only with changes to diet Implanted Monitor Derived Hemodynamics in Pulmonary Arterial Hypertension N=8, a sub-study of a pilot implanted hemodynamic monitor (Chronicle® Device) study in PAH RV pressure waveforms recorded utilizing the implantable monitor and SG catheter Breath-by-breath cardiac output was recorded during acute IV epoprostenol infusion at 3, 6 and 9 ng/kg/min. Late systolic pressure augmentation and the cardiac output were estimated using the right ventricular pressure waveforms and correlated with direct measurement of cardiac output (Fick) Karamanoglu, M, et al, Chest 2007, 132:37-43 CO= 30 x(P1st-PES)x(STI-PEI)/RR AP=PSYS-P1st Implanted Monitor Derived Hemodynamics in PAH Psys P1st 40 Qmax ePAD mmHg The basic features of the RV pressure waveform and the identification of these feature points using the first derivative of the RV pressure waveform. Three of these points identify the turning points of the PA flow waveform (in mmHg), PEI, T1st and STI, where PEI = time of dP/dtmax, T1st = time of the early shoulder of the RV pressure waveform, and STI = time of dP/dtmin. The area of the triangle (shaded area) = (P1st-Pes)x ED/2 corresponds to estimated stroke volume (SV). RR = R-R interval PES SV SV ED T1st 0 PEI STI RR dP/dtmax 0 mmHg/s The augmented pressure (AP) caused by the presence of wave reflection is the difference between the late systolic pressure (Psys) and the early systolic shoulder (P1st). dP/dtmin Fig 1, Karamanoglu, M, et al, Chest 2007, 132:37-43 -1000 500 ms Implanted Monitor Derived Hemodynamics in Pulmonary Arterial Hypertension 90 90 mmHg 120 mmHg 120 60 30 0 60 30 0 200 400 600 t (ms) 800 1000 0 0 200 400 600 800 1000 t (ms) The estimated PA flow waveforms inscribed within the RV pressure waveforms before (Left) and after (Right) the infusion of IV epoprostenol. Note that the increase in the estimated stroke volume following the infusion. Fig 3, Karamanoglu, M, et al, Chest 2007, 132:37-43 6 500 4 300 200 2 mmHg L/min/m2 400 100 0 0 Measured (L/min/m2) Implanted Monitor Derived Hemodynamics in Pulmonary Arterial Hypertension Cardiac Index 6 5 4 Y=X, r2=0.95 3 2 1 0 0 1 2 3 4 5 6 Estimated Measured Dose L/min/m2 6 4 2 0 01 03 05 06 07 09 31 34 Difference (L/min/m2) Estimated (L/min/m2) 1.0 +95% CI=0.37 L/min/m2 0.5 Mean=0.0 L/min/m2 0.0 -95% CI=0.37 L/min/m2 -0.5 Bland - Altman Plot -1.0 0 1 2 3 4 5 2 Average (L/min/m ) Fig 6 & 7, Karamanoglu, M, et al, Chest 2007, 132:37-43 6 The Implantable Hemodynamic Monitor: Potential Clinical Applications Improve our understanding of the hemodynamic alterations that occur with heart failure and the hemodynamic response to therapy Allow more precise titration and tailoring of heart failure and pulmonary vascular disease (PH) therapy Provide “early warning” of hemodynamic deterioration Aid in the diagnosis of symptomatic events in the outpatient setting (home or clinic) Provide method by which to develop, refine, and optimize the use of chronic hemodynamic data for longterm patient management Possibly affect the intermediate and long term morbidity and mortality in patients with heart failure Heart Rate UAB E11 Chronically Implanted Hemodynamic Monitor 68y/o male DM, IHD, EF 45%, severe diastolic dysfunction, renal insufficiency, morbidly obese; intermittently noncompliant with salt and fluid restriction. Rx: torsemide 150 bid metolazone spironolactone 50 bid atenolol 25 qDay RV Systolic Pressure (mmHg) 40 RV Diastolic Pressure (mmHg) 20 ePAD (estimated PA diastolic) Pressure (mmHg) Nesiritide + IV diuretics Heart Rate UAB E11 68y/o male DM, IHD, EF 45%, severe diastolic dysfunction, renal insufficiency, morbidly obese; intermittently noncompliant with salt and fluid restriction. Rx: torsemide 150 bid metolazone spironolactone 50 bid atenolol 25 qDay After episode of nausea and diarrhea, consumed beef and chicken bouillon (high in salt). Admitted with hyperkalemia (7.7mm/l) and class IV CHF, 3 lb weight gain. RV Systolic Pressure (mmHg) 40 RV Diastolic Pressure (mmHg) 20 ePAD (estimated PA diastolic) Pressure (mmHg) Nesiritide + IV diuretics The Implantable Hemodynamic Monitor: Potential Clinical Applications Improve our understanding of the hemodynamic alterations that occur with heart failure and the hemodynamic response to therapy Allow more precise titration and tailoring of heart failure and pulmonary vascular disease (PH) therapy Provide “early warning” of hemodynamic deterioration Aid in the diagnosis of symptomatic events in the outpatient setting (home or clinic) Provide method by which to develop, refine, and optimize the use of chronic hemodynamic data for longterm patient management Possibly affect the intermediate and long term morbidity and mortality in patients with heart failure Chronicle™ Implantable Hemodynamic Monitor: Patient Example UAB Pt E1: Systolic and Diastolic 80 70 Implant 60 RVsys mmHg 50 40 30 20 RVdiast 10 0 -10 13-Oct 14-Oct 15-Oct 16-Oct 17-Oct 18-Oct days 19-Oct 20-Oct Clinic Visit 21-Oct 22-Oct Chronicle™ Implantable Hemodynamic Monitor: Patient Example UAB Pt E1: Temperature 40.0 39.5 39.0 degrees C Implant 38.5 38.0 37.5 37.0 36.5 36.0 13-Oct 14-Oct 15-Oct 16-Oct 17-Oct 18-Oct 19-Oct 20-Oct days Clinic Visit 21-Oct 22-Oct The Implantable Hemodynamic Monitor: Potential Clinical Applications Improve our understanding of the hemodynamic alterations that occur with heart failure and the hemodynamic response to therapy Allow more precise titration and tailoring of heart failure and pulmonary vascular disease (PH) therapy Provide “early warning” of hemodynamic deterioration Aid in the diagnosis of symptomatic events in the outpatient setting (home or clinic) Provide method by which to develop, refine, and optimize the use of chronic hemodynamic data for longterm patient management Possibly affect the intermediate and long term morbidity and mortality in patients with heart failure COMPASS-HF Study Design / Enrollment Baseline Evaluation Withdrew prior to implant = 24 n = 301 Implant Attempted Unsuccessful implant = 3 n = 277 Total Clinician Access Group = 134 CHRONICLE Randomization - 274 (stratified by LVEF or 50%) Blocked Clinician Access Group =140 CONTROL 1 Month Follow-up 1 Month Follow-up 3 Month Follow-up 3 Month Follow-up 6 Month Follow-up 6 Month Follow-up At 6 months Chronicle guided care enabled in all patients Study timeline: First implant March 18, 2003; Database closed June 3, 2005 Bourge, RC, et al. J Am Coll Cardiol 2008;51:1073-9 Study Clinical Care Guidelines Pressure State • • (RV systolic, RV diastolic, Estimated PAD) Treatment strategy Hypervolemic • Medication titration • Modify dietary restrictions • ? Hospitalize, ? IV therapy Optivolemic • Ongoing management & assessment Hypovolemic • Medication titration • Modify dietary restrictions • ? hospitalize, ? fluid administration Ranges were determined for each patient at baseline and assessed over time Guidelines were followed in 96% of patient state assessments COMPASS Patient Baseline Characteristics Chronicle n=134 Control n=140 p-value 58 14 58 13 0.75 Gender (% female) 34 36 0.80 Ethnicity (% Caucasian) 47 53 0.71 Etiology (% Ischemic) 47 44 0.72 NYHA (% Class III) 84 87 0.49 2.2 1.9 2.4 1.7 0.29 Concomitant Devices (%) 43 37 0.39 Diuretic Use (%) 93 99 0.02 ACE-I or ARB Use (%) 83 80 0.64 Beta Blockade Use (%) 81 79 0.88 Age, years (mean ± sd) Prior HF Events (mean ± sd)* *Six months prior to implantation RESULTS: All Safety Objectives Exceeded Number of patients at risk Number of complications (patients) Complication-free survival at 6 months (95% CI) System 277* 24 (23) 91.5% (88.7%-94.3%) Sensor 274 0 (0) 100% (98.9%-100%) * 3 patients had unsuccessful implant Bourge, RC, et al. J Am Coll Cardiol 2008;51:1073-9 Comparison of Observed Call Rates During Randomized Period Call Type Group Mean Call Rate (Calls/Patient) CHRONICLE 20.7 Clinician-Initiated 0.88 CONTROL 21.2 CHRONICLE 3.0 Patient-Initiated 0.51 CONTROL 2.8 CHRONICLE 23.7 Overall Call Rate 0.94 CONTROL CHRONICLE (n=134) CONTROL (n=140) p-value 24.0 Bourge, RC, et al. J Am Coll Cardiol 2008;51:1073-9 Efficacy Objective Control (n = 140) # of Pts with Events 44 60 Total HF Related Events 84 113 Hospitalizations 72 99 Emergency Department Visits 10 11 2 3 0. 67 0.85 Urgent Clinic Visits Event Rate / 6months* % Reduction in Event Rate 1. 2. Cumulative Events 120 Chronicle Control 100 Events Chronicle (n =134) (p=0.091; 21% p=0.332) 80 60 40 20 0 1 2 4 Months Poisson model - Scaled Deviance = 1.8 Negative Binomial model - Scaled Deviance = 0.8 Bourge, RC, et al. J Am Coll Cardiol 2008;51:1073-9 6 Major Component of Primary Endpoint: HF-related Hospitalization Time to Event Analysis Freedom from HF-related hospitalization 100% 80% Chronicle Control 60% 40% RR = 0.64 (95%CI = 0.42 - 0.96) p=0.03 20% 0% 0 50 100 150 200 Days Bourge, RC, et al. J Am Coll Cardiol 2008;51:1073-9 Efficacy in NYHA Class III Patients Control (n = 122) # of Pts with Events 35 51 Total HF Related Events 58 99 50 86 Emergency Department Visits 6 11 Urgent Clinic Visits 2 3 0. 54 0.85 Hospitalizations Event Rate / 6months 1 % Reduction in Event Rate 1. 2. Cumulative Events 120 100 Events Chronicle (n =112) Chronicle Control 80 60 40 20 0 2 (p=0.0061; 36% p=0.0582) 4 6 Months Poisson model - Scaled Deviance = 1.7 Negative Binomial model - Scaled Deviance = 0.8 Bourge, RC, et al. J Am Coll Cardiol 2008;51:1073-9 Body Weight and RV Diastolic Pressure Before Hospitalization Body Weight Lbs RV Diastolic Pressure mmHg 300 25 250 20 200 * * Chronicle Control 150 15 * * 100 7 weeks 4 weeks 2 weeks 1 day prior 5 days post 10 7 weeks 4 weeks * = p<0.05 vs 1 day prior hospitalization 2 weeks 1 day prior 5 days post ™ ® Savacor HeartPOD Heart Failure Therapy System Senses: Left Atrial Pressure Temperature IEGM ‘Chip’ in tip RF power / telemetry Personalized-realtime: LASIX® (Furosemide) 40 mg 1 white tablet Drug management CRM programming RA LA LASIX® 40 Recheck in 12h CardioMEMS Wireless Heart Failure Sensor HF Sensor technology based on clinically proved commercially available system for abdominal aneurysms repair monitoring AAA Sensor HF Sensor Externally powered – no battery Remon Tech (Boston Scientific): Acoustic-Non Data Recording Miniature pressure transducer, attached to self expanding anchor device, inserted into pulmonary artery via percutaneous venous approach Implant activated, measurements taken, data transmitted via ultrasound External unit operated by patient, displays Anchoring device and records data Implant may communicate with other implanted devices using acoustic telemetry Micro battery, life > 5 years; may be recharged using acoustic energy The Implantable Hemodynamic Monitor: Potential Clinical Applications Improve our understanding of the hemodynamic alterations that occur with heart failure and the hemodynamic response to therapy Allow more precise titration and tailoring of heart failure and pulmonary vascular disease (PH) therapy Provide “early warning” of hemodynamic deterioration Aid in the diagnosis of symptomatic events in the outpatient setting (home or clinic) Provide method by which to develop, refine, and optimize the use of chronic hemodynamic data for longterm patient management Possibly affect the intermediate and long term morbidity and mortality in patients with heart failure