presentation ( format)
advertisement

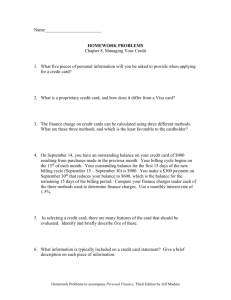
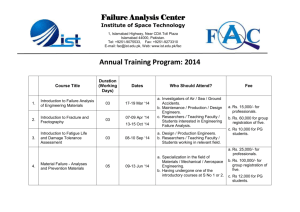
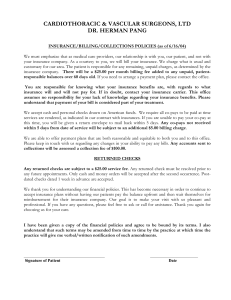
IMPLEMENTING A MEDICAL BILLING MODEL: STUDENT HEALTH CENTER REVENUE POTENTIAL Donna Hash & Merry Lawrence Presentation Overview • Background • Getting Started • Terms & Definitions • Fee Schedule • Planning Process • Operational Changes • Key Considerations • Implementing the Process • Evaluation • Monitoring & Reporting • Lessons Learned • Next Steps Background: Motivating Factors • Our Previous Approach • Financial Considerations • University Administrative Charges • Student Fees • Organizational Aims • Improve Services to Students • Recruit & Retain Quality Clinicians • Data • In 2008, ~90% of students surveyed were insured* *Based on spring 2010 NCHA data (1,632 student respondents) Getting Started: Exploring New Opportunities • Health Services Fee • Ongoing cost increases and budget/resources decreases • Medical Billing Model (old vs. new) • Provide cost-effective services & generate revenue • Consistent with industry billing standards • Establish a Fee Schedule • What to charge? How much? • Conversion factor Gross Revenue $1,000,000 $900,000 $800,000 $700,000 $600,000 $500,000 Gross Revenue $400,000 $300,000 $200,000 $100,000 $0 2007-2008 2008-2009 2009-2010 2010-2011 2011-2012 2012-2013 Getting Started: Learning the Lingo Operational Changes: Preliminary Decisions • In-house Billing vs. Billing Service • EMR/EHR • Establishing a Fee Schedule • Conversion factor • CPT, E&M Codes • RBRVS Malpractice Non Fac Total 15952 Excision, trochanteric pressure ulcer, w/ skin flap closure; 12.31 12.03 12.03 2.63 26.97 26.97 090 15953 15956 with ostectomy Excision, trochanteric pressure ulcer, in preparation for muscle or myocutaneous flap or skin graft closure; 13.57 16.79 13.29 14.05 13.29 14.05 2.67 3.42 29.53 34.26 29.53 34.26 090 090 15958 16000 with ostectomy Initial treatment, first degree burn, when no more than local treatment is required 16.75 .89 14.83 1.01 14.83 .34 3.39 .12 34.97 2.02 34.97 1.35 090 000 16020 Dressings and/or debridement of partialthickness burns, initial or subsequent; small (less than 5% total body surface area) .71 1.56 .77 0.10 2.37 1.58 000 16025 Medium (eg, whole face or whole extremity or 5% to 10% total body surface area) 1.74 2.27 1.26 0.29 4.30 3.29 000 16030 Large (eg, more than 1 extremity., or greater than 10% total body surface area) 2.08 2.86 1.45 0.37 5.31 3.90 000 16035 16036 Escharotomy; initial incision Each additional incision (list separately in addition to code for primary procedure) 3.74 1.50 1.53 0.69 1.53 0.69 0.63 0.27 5.90 2.46 5.90 2.46 000 zzz 17000 Destruction (eg, laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement), premalignant lesions (eg, actinic keratoses), first lesion 0.65 1.65 0.92 0.08 2.38 1.65 010 Code Description Work Value Non Fac PE FAC PE Fac Total Global Gap Fee for Service Example: Code 17110 Description Deconstruction (eg, laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement), of benign lesions other thank skin tags or cutaneous vasular proliferative lesions; up to 14 lesions Work Value Non Fac PE FAC PE Malpractice Non Fac Total Fac Total Global Gap 0.70 2.48 1.27 0.08 3.26 2.05 010 Non FAC Total (code value) = 3.26 Sample Conversion Factor = $50.00 Code Value x Conversion Factor 3.26 x 50 = $163.00 Operational Changes: Key Considerations • Contracting with insurance plans • Top 3 • Clearinghouses • Electronic medical claim submission (ERA) • Staffing • Billing Manager • Payment processing • • • • • • • Check ICD/CPT codes Create billable claim forms Submit claims (electronically) Correct/re-bill claims Post payments Manage accounts receivables Patient responsibility charges to patient accounts Operational Changes: Insurance Aging A/R • Utilize Practice Management Software/EMR • Document patient information (e.g., store ID cards) • Use reporting tools • 3 Primary Reports: • Accounts Receivable Aging Report • Payer Mix Analysis • Summary of Charges • Analyze by transaction code Evaluation: Monitoring & Reporting A/R Report: • Patient charges detailed by plan • Aging “buckets” • Focus on oldest claims • Analysis of aging conducted by the Billing Manager Evaluation: Payer Mix Analysis Evaluation: Summary of Charges Lessons Learned • Provider Cooperation & Coordination • Clinical staff buy-in • Management support • Billing Office Staff • Professional development • Reporting Process • Payment codes, adjustment codes, charting system, missed charges etc. • Monitor reimbursements for errors • Annual Technology Upgrades • Plan for changes & train staff Next Steps • Adapt to ACA • Contract with additional insurers • Adjust fee schedule • Consider the value of an in-house patient advocate • Student advisory board • Financial assistance plan • Prepare for ICD 10 • October 1, 2015 expected implementation • Continue to support the health & well-being of students Contacts & Resources Contacts at WSU: Online Resources: Donna Hash, Administrative Manager Health & Wellness Services 509.335.6759 donna.hash@wsu.edu Resource-Based Relative Value Scale www.ama-assn.org//ama/pub/physician-resources/solutionsmanaging-your-practice/coding-billing-insurance/medicare/theresource-based-relative-value-scale.page Medical Group Management Association Merry Lawrence, Billing Office Manager Health & Wellness Services 509.335.5293 mklawrence@wsu.edu www.mgma.com American Medical Association www.ama-assn.org/ama/pub/physicians/physicians.page Credentialing & Contracting Article www.articlesbase.com/business-articles/improve-yourpractice039s-financial-health-focus-on-the-four-ps-in-a-podpatients-payers-payments-and-productivity-2003088.html