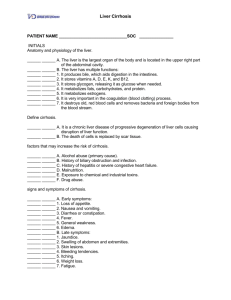
File - Elizabeth Leen
advertisement

Cirrhosis of the Liver with Resulting Hepatic Encephalopathy By: Michelle Hoffman Patient • Teresa Wilcox • Physician: P. Horowitz, MD • Education: doctoral graduate student • Age: 26-years-old • Height: 5’9” (1.7 m) • Current Weight: 125 lbs (56.8 kg) • Usual Body Weight: 145 lbs • BMI:18.5 kg/m^2 – Underweight • Dx: Probable cirrhosis secondary to chronic hepatitis 2 Patient History • Hepatitis C Dx 3 years ago • Complaints of fatigue, anorexia, N/V, weakness • Lost 10 lbs since last visit 6 months ago • Bruising and yellowish skin • Family hx cirrhosis (grandfather) 3 Physical Exam • Tired in appearance • Enlarged esophageal veins • Warm and dry skin with bruising on lower arms and legs • Normal muscular tone and ROM • No edema or ascites 4 Nutrition History • Has not an an appetite for last few weeks – Has not eaten in the last 2 days – Nutrition therapy of small, frequent meals with plenty of liquids 3 years ago • Breakfast: calcium-fortified orange juice • Lunch: soup and crackers with diet coke • Dinner: Chinese or Italian carry-out • Fluids: small sips of water, diet coke, or juice – Does not consume alcohol • Current diet order: Soft, 4-g Na, high-kcal 5 Abnormal Chemistry • Albumin – Normal: 3.5-5 g/dL – Ms. Wilcox: 2.1 g/dL • Total protein – Normal: 6-8 g/dL – Ms. Wilcox: 5.4 g/dL • Bilirubin – Normal: ≤ 0.3 mg/dL – Ms. Wilcox 3.7 mg/dL 6 Abnormal Hematology • RBC – Normal: 4.3-5.4 – Ms. Wilcox: 4.1x10^6/mm^3 • HGB – Normal: 12-15 g/dL – Ms. Wilcox: 10.9 g/dL • HCT (hematocrit) – Normal: 37-47% – Ms. Wilcox: 35.9% 7 Abnormal Hematology • MCV (mean cell volume) – Normal: 80-96 μm^3 – Ms. Wilcox: 102 μm^3 • Ferritin(protein that stores iron) – Normal: 20-120 mg/mL – Ms. Wilcox: 18 mg/mL • PT (prothrombin time) – Normal: 11-16 sec – Ms. Wilcox: 18.5 sec 8 Diagnosis • Cirrhosis – – – – – 12th leading cause of death in the U.S. Ending stage of liver disease Secondary to chronic hepatitis C Replacement of healthy liver tissue with scar tissue Blocks the flow of blood through the liver, causing kidney failure, enlarged liver, thickening of various tissues, portal hypertension, ascites, etc. 9 Diagnosis 10 11 Etiology • Common causes of cirrhosis: – – – – – – – Alcohol-related liver disease Chronic hepatitis C Chronic hepatitis B Autoimmune hepatitis Nonalcoholic fatty liver disease (NAFLD) Bile duct disorders Hereditary disorders 12 Symptoms • Weakness • Fatigue • Loss of appetite • N/V • Weight loss • Abdominal pain and bloating • Itching 13 Complications & Warning Signs • Edema &Ascites • Bruising and bleeding • Portal hypertension • Esophageal varices • Jaundice • Hepatic encephalopathy • Insulin resistance and type II diabetes 14 Ascites 15 Diagnosing Cirrhosis • Look at the clinical signs & symptoms • Biopsy, CT Scan, and MRI may reveal an enlarged liver, reduced blood flow, and /or ascites – Biopsy’s are less common because it it expensive, and usually only confirms a diagnosis 16 Diagnosing Cirrhosis • Blood tests to measure: – – – – Measures function of the liver Albumin Bilirubin PT (Prothrombin Time) • Liver enzymes: – Measures injury to the liver – ALT – AST 17 Severity • MELD – Model for end-stage liver disease – 6 - 40 score range—6 is a likelihood that patient will survive 90 days – Score comes from: •Bilirubin count—measures bile pigment in the blood •Creatine levels—tests kidney function •INR (international normalizes ratio)—tests blood clotting tendency 18 Treating Cirrhosis • Primary medical treatments for cirrhosis: – – – – Preventing further damage Treatment of the complications Liver transplant Nutrition therapy 19 Treating Cirrhosis • Preventing further damage: – The first thing doctors will recommend is abstaining from alcohol and any drugs that will damage the liver further – Consume a balanced diet and a multivitamin may be recommended (D and K especially) – Avoid nonsteriodalantinflammatory drugs (NSAIDS) •Ibuprofen 20 Treating Cirrhosis • Treating complications: – Ascites •Antidiuretics – Bleeding from varices •Beta-blockers •Propanolol – Hepatic Encephalopathy •Laxatives (lactulose) 21 Treating Cirrhosis • Liver Transplant: – Cirrhosis in irreversible, and many patients will eventually need a liver transplant as the only option left – 80% of patient live for 5 years after surgery 22 Nutrition Therapy Recommendation Kcals 35-40 kcal/kg Protein 1.6 g/kg/day Fat 30% of calories/day CHO 50-60% of calories/day Sodium No more than 2-g/day Fluid 1.2-1.5 L/day Calcium 1,000-1,500 mg Vitamins May need multivitamin supplement; see doctor 23 Energy & Protein • Ms. Wilcox’s energy needs: • Weight: 56.8 kg • 35 x 56.8= 1,988 calories • 40 x 56.8= 2,272 calories – 2,000-2,200 calories/day. • Ms. Wilcox’s protein needs: • 1.6 x 56.8=90.8 – ~ 91 g protein/day 24 Nutrition Problems – Inadequate energy intake: NI-1.4 – Inadequate oral intake: NI-2.1 – Malnutrition: NI-5.2 – Inadequate protein-energy intake: NI-5.3 – Underweight: NC-3.1 25 PES Statements – Inadequate energy intake related to decreased appetite, fatigue, and nausea by recent cirrhosis of the liver dx as evidenced and diet recall – Underweight related to decreased appetite in past three weeks as evidenced by diet recall, recent 10 lb weight loss, and BMI of 18.5 kg/m^2 26 Nutrition Intervention & Support • Small frequent feedings • Encourage oral liquid supplements • High kcal and protein diet • Restrict sodium intake to ≤ 2-g • Abstain from alcohol consumption • Provide foods that are easy to chew and swallow • Optimize gastric emptying – Avoid excessive fiber – Control blood glucose – Liquids over solids if necessary 27 Prognosis • Depends on stage of the disease • Once the liver has scarred over, it cannot be reversed, meaning it cannot return to its normal function • Survival is generally 10 years after dx (90%) • Complications of ascites, portal hypertension, jaundice, hepatorenal syndrome, hepatic encepalopathy, etc. • Liver transplant will most likely be needed as a result of cirrhosis 28 Prognosis: Stages of Cirrhosis • Stage 1 – Patients without gastro-esophageal varices or ascites have mortality of ~1% per year • Stage 2 – Patients with gastro-esophageal varices but no ascites have mortality of ~4% per year • Stage 3 – Patients without gastro-esophageal varices but have ascites have mortality rate of ~20% per year • Stage 4 – Patients with GI bleeding from portal hypertension with/without ascites have mortality of ~57% per year 29 References • Nelms, M., Sucher, K. P., Lacey, K., & Roth, S. L. (2011). Nutrition Therapy and Pathophysiology. Belmont, California: Wadsworth, Cengage Learning. • "Prognosis." Best Practice. BMJ Group, 14 June 2012. Web. 11 Nov. 2012. <http://bestpractice.bmj.com/best-practice/monograph/278/followup/prognosis.html>. • Longstreth, George F. "Cirrhosis: MedlinePlus Medical Encyclopedia." Medline Plus. U.S. National Library of Medicine, 16 Oct. 2011. Web. 11 Nov. 2012. <http://www.nlm.nih.gov/medlineplus/ency/article/000255.htm>. • Lee, Dennis. "Cirrhosis (Liver) Symptoms, Causes, Treatment - How Is Cirrhosis Treated? on MedicineNet." MedicineNet. N.p., 2012. Web. 11 Nov. 2012.<http://www.medicinenet.com/cirrhosis/page5.htm>. • "Cirrhosis." Cirrhosis. University of Maryland Medical Center, 2011. Web. 11 Nov. 2012. <http://www.umm.edu/patiented/articles/what_causes_cirrhosis_000075_2.htm> . • "National Digestive Diseases Information Clearinghouse (NDDIC)." Cirrhosis. N.p., Dec. 2008. Web. 11 Nov. 2012. <http://digestive.niddk.nih.gov/ddiseases/pubs/cirrhosis/>. • "Learning About Your Health." Cirrhosis of the Liver. CPMC Sutter Health, 2012. 30