Types of Urinary Catheters - department general surgery & surgical
advertisement
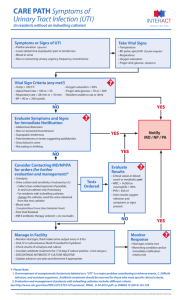
URINARY ELIMINATION. DRAINAGE AND TUBES. URINARY CATHERTERIZATION Sometimes a person is unable to urinate using a toilet, bedpan, urinal, or bedside commode, due to disability or illness. In these situations, a urinary catheter is used. A catheter is a tube that is inserted into the body for the purpose of administering or removing fluids. A urinary catheter is inserted into the bladder through the urethra (or through an incision made in the abdominal wall) to allow the urine in the bladder to drain out. A urinary catheter is used in many different situations: 1. A urinary catheter may be inserted to drain the bladder before or during a surgical procedure, during recovery from a serious illness or injury, or to collect urine for testing. 2. A urinary catheter may be used for a person who is incontinent of urine, if the person has wounds or pressure ulcers that would be made worse by contact with urine. 3. A urinary catheter is necessary when a person is unable to urinate because of an obstruction in the urethra. Usually, inserting a urinary catheter is beyond the scope of practice for a nursing assistant, although in some facilities, nursing assistants are provided with additional training that allows them to catheterize residents or patients. Inserting a catheter is a procedure that requires sterile technique because it involves putting a foreign object (that is, the catheter) into a person’s body. If sterile technique is not used, the catheter can introduce infection-causing bacteria into the bladder. Regardless of whether or not you are trained to actually insert urinary catheters, caring for people who have urinary catheters in place will almost certainly be a part of your daily duties. https://youtu.be/gcVzgOVdpU0 Types of Urinary Catheters You will see many different types of urinary catheters in use. 1. Straight Catheters A straight catheter, also known as a Robinson, Rob-Nel, or Red Rubber catheter, is used when the catheter is to be inserted and removed immediately. The catheter is introduced into the bladder, the urine is allowed to drain out, and the catheter is removed. This type of catheterization may be used to obtain a sterile urine specimen from a woman, before or after surgery, after a vaginal delivery, or when a person needs to empty his bladder but cannot as a result of pain or swelling that is temporary. New guidelines issued by the CDC state that urinary catheters should not be used to obtain urine samples from a person who is able to void voluntarily because of the increased risk of infection. 2. Indwelling Catheters An indwelling catheter, also known as a retention or Foley catheter, is left inside the bladder to provide continuous urine drainage. An indwelling catheter has a soft balloon that is inflated inside the bladder to keep the catheter from sliding out of the urethra. Urine collects in a drainage bag, which is attached to the indwelling catheter by a length of tubing. An indwelling catheter may have two lumens or three lumens. A double-lumen indwelling catheter has two lumens. One lumen, which connects to the catheter tubing, is for urine drainage. The other is used to inflate the balloon that holds the catheter in place. A triplelumen indwelling catheter has three lumens. The extra lumen is used to flush the bladder with irrigation fluid. Regular flushing of the bladder with irrigation fluid helps to keep blood clots from forming inside the bladder. This is important in certain situations, such as when a man has just had prostate surgery. 3. Suprapubic Catheters A suprapubic catheter is a type of indwelling catheter. The suprapubic catheter is inserted into the bladder through a surgical incision made in the abdominal wall, right above the pubic bone. This type of catheter is most often used for people with blocked urethra, and for men. Men typically are notable to use an indwelling urinary catheter that is inserted through the urethra for long periods of time due to the anatomy of the male urethra. While a woman’s urethra is straight and only about 2 inches long, a man’s urethra is curved in an “S” shape and is about 6 inches long. In men, the pressure of the indwelling catheter can cause erosion of the mucous membrane that lines the urethra in the curved areas. CARING FOR A PERSON WITH AN INDWELLING URINARY CATHETER Indwelling urinary catheters are connected by a length of tubing to a urine drainage bag. Urine drains continuously from the bladder, through the catheter, down the tubing, and into the drainage bag. There are several different types of urine drainage bags that you will see in the health care setting. Some urine drainage bags have a long length of tubing that allows them to be carried or secured to a bed frame or the back of a wheelchair. Other urine drainage bags, called “leg bags,” are connected to the catheter by a short length of tubing and secured to the person’s thigh with straps. Leg bags are useful because they can be concealed underneath a person’s clothing and they allow the person to move around freely. When a regular urine drainage bag with a long length of tubing is being used, the tubing is secured loosely to the person’s body near the insertion site using a catheter strap or adhesive tape. Securing the tubing to the person’s body prevents the catheter from being accidentally pulled out during repositioning. In women, the tubing is attached to the thigh. In men, the tubing is attached to the thigh or lower abdomen. A little bit of slack is left in the tubing to prevent the catheter from pulling against the bladder outlet and the urethral opening. The remaining length of tubing is then gently coiled and secured to the bed linens using a plastic clip. Coiling the tubing prevents the tubing from becoming bent or kinked, which would stop the free flow of urine into the drainage bag. Coiling the tubing and securing it to the bed linens also keeps the weight of the tubing from pulling against the person’s body. The drainage bag is then secured to the bed frame or the back of the person’s wheelchair, at a level lower than the person’s bladder. If the drainage bag and tubing are higher than the person’s bladder, then gravity could cause old, contaminated urine to run back down the tubing and into the person’s bladder, causing an infection. All urine drainage bags have a connection adapter (where the catheter tubing attaches) and an emptying spout that is opened to allow urine to drain from the bag. Because the inside of the catheter and tubing are sterile, it is safer for the person if the bag is not disconnected from the tubing once the catheter is in place. Disconnecting the bag from the tubing can allow harmful bacteria to enter the catheter. Occasionally, the tubing has to be disconnected from the bag (for example, to change the bag if it is leaking, to replace a regular drainage bag with a leg bag, or to perform certain procedures). If you must disconnect the tubing from the bag, be sure to prevent the end of the tubing from touching anything, and wipe the exposed tubing with an antibacterial wipe before reconnecting the drainage bag. Providing Catheter Care Although you may not be permitted to catheterize your patients or residents, you will most likely be responsible for providing catheter care. Catheter care involves thorough cleaning of the perineal area (especially around the urethra) and the catheter tubing that extends outside of the body, to prevent infection. Providing good catheter care is important because the catheter provides a pathway for bacteria to travel up from the perineum into the bladder, where they can cause infection. In addition, having a catheter in place eliminates the “flushing” action of normal urination, which helps to remove bacteria from the urinary tract naturally. Because bacteria can be introduced into the body both when a urinary catheter is inserted and after it is in place, urinary tract infections in catheterized people are among the most common health care– associated infections (HAIs). (Remember that HAIs are acquired in the health care setting.) In an effort to reduce the risk of HAIs in people who are catheterized, many facilities require catheter care to be provided routinely (for example, once or twice daily), and again whenever the perineal area becomes soiled (such as when a person is incontinent of faeces). Soap and water should be used when providing catheter care. https://youtu.be/g6rnQR7Cf1w?list=PLBB3C7355164DE53C URINARY INCONTINENCE Urinary incontinence is the inability to hold one’s urine, or the involuntary loss of urine from the bladder. Urinary incontinence may be temporary or permanent. Temporary urinary incontinence can occur as a result of a bladder infection, or after an indwelling catheter that has been in place for a long time is removed. Permanent urinary incontinence can be caused by many things, including: 1. Decreased muscle tone in the bladder or the muscles that support the bladder, such as occurs after childbirth or from obesity Injuries or illnesses that affect the spinal cord, the brain, or the nerves that control bladder function 2. Dementia Urinary incontinence can be emotionally devastating for both the incontinent person and the person’s caregivers. For the person who is incontinent, having wet clothes or smelling like urine can be very embarrassing. In addition, being incontinent of urine places a person at risk for developing skin problems (such as rashes and pressure ulcers) and for falling (as the person rushes to the bathroom to avoid having an accident). For the caregiver, caring for a person who is incontinent of urine can be frustrating and emotionally draining. It is not uncommon to change a person’s clothes or bedding, only to have the person wet herself all over again. Because caring for an incontinent person can be so emotionally trying and time consuming, incontinence is the factor that most often leads family members to have a relative admitted to a long-term care facility. Types of Urinary Incontinence There are many types of urinary incontinence. ■ Stress incontinence is probably the most common type of urinary incontinence. In stress incontinence, urine leaks from the bladder when the person coughs, sneezes, or exerts herself. Stress incontinence can also occur if a person delays voiding and the bladder becomes too full. Childbirth, obesity, and loss of muscle tone as a result of aging are all factors that can contribute to stress incontinence. Stress incontinence can also occur in men after prostate surgery. Stress incontinence can often be corrected with exercises or surgery. ■ Urge incontinence is the involuntary release of urine right after feeling a strong urge to void. This type of incontinence is common in people with urinary tract infections because irritation of the bladder causes the bladder muscle to spasm, expelling the contents of the bladder with little warning. Other conditions that decrease the ability of the bladder to hold urine, such as an enlarged prostate gland or increased intake of caffeinated beverages or alcohol, can also cause urge incontinence. ■ Functional incontinence occurs in the absence of physical or nervous system problems affecting the urinary tract. The person just cannot make it to the bathroom in enough time, or wait until a bedpan or urinal is provided. It is thought that being in a strange environment (as a hospital or long-term care facility would be to someone who has just been admitted) contributes to functional incontinence. Confusion, disorientation, and loss of mobility are also contributing factors. ■ Overflow incontinence occurs when the bladder is too full of urine. Overflow incontinence is associated with urinary retention, which is the inability of the bladder to empty either completely during urination, or at all. Urinary retention can result from blockage of the bladder outlet (such as occurs with an enlarged prostate gland or from swelling of the urethra during labour or childbirth), or from pain following a surgical procedure. Some injuries that involve the spinal cord can also keep the bladder from emptying fully, leading to urinary retention because the bladder does not empty completely when the person voids, it refills with urine quickly, and the urine simply overflows. A person with overflow incontinence may “dribble” urine in between visits to the bathroom. If a person cannot empty his bladder completely, it may be necessary to insert a catheter (either temporarily or permanently) to allow urine to drain from the bladder and prevent urinary retention and overflow incontinence from occurring. ■ Reflex incontinence occurs when there is damage to the nerves that enable the person to control urination. The bladder fi lls, but the person does not feel the urge to urinate. When the bladder is completely full, it empties reflexively (that is, automatically). Some people with certain disorders of the nervous system, such as paralysis from a spinal cord injury, will catheterize themselves with a straight catheter on a regular basis to prevent reflex urinary incontinence. MANAGING URINARY INCONTINENCE Many products are available to help manage urinary incontinence, including incontinence pads, incontinence briefs, and condom catheters. In addition, techniques such as bladder training may be used to help a person overcome certain types of incontinence. For some people, temporary or permanent catheterization may be necessary to manage the incontinence. 1. Incontinence Pads and Briefs Products made for urinary incontinence are available to help prevent soiling of clothes and furniture. Incontinence pads and briefs are specially made to absorb urine and hold it away from the person’s skin. Keeping the skin dry helps to reduce the skin problems that can occur from prolonged contact with urine. Incontinence pads are placed inside the person’s underpants to prevent wetting of the clothes and to draw the moisture away from the person’s body. Incontinence briefs are worn instead of underpants. Incontinence pads and briefs are very useful for active people. For a person who is confined to bed, special bed protectors are used to help to keep the bed linens and mattress dry and to wick urine away from the person’s skin. Many facilities have policies that specify that incontinence briefs are to be used only when the person is out of bed, and that bed protectors are to be used when the person is sleeping. Incontinence briefs tend to fit closely, which makes it difficult for air to reach the skin. Switching between briefs and bed protectors helps to prevent skin breakdown by allowing the skin to be exposed to the air at night. As a nursing assistant, you must make sure that these incontinence products are changed frequently and that urine is cleaned from the skin whenever the change occurs. 2. Condom Catheters A condom catheter can be used to manage incontinence in men. A condom catheter is not a true catheter because it is not placed inside the body. It consists of a soft plastic or rubber sheath, tubing, and a collection bag for the urine. The sheath is placed over the penis and the collection bag is attached to the leg. The urine flows through the tubing into the collection bag, allowing the man to urinate at will. The condom must fit the penis. It should be fastened securely enough to prevent leaking, but not so snugly that it restricts circulation. Many condom catheters have adhesive material on the inside of the condom that allows for a good seal. Others must be secured with elastic tape. The tape strip is applied in a spiral fashion to allow for changes in the size of the penis. Applying the tape in an overlapping, circular fashion would compromise blood flow if the man had an erection, possibly causing permanent damage to the penis. Use of a condom catheter requires good skin care. The penis must be cleaned, and the condom apparatus changed, daily. 3. Bladder Training Bladder training is commonly used to help people relearn how to control their urinary elimination. For example, a person may be encouraged to use the bedpan, urinal, or commode at scheduled times. Scheduling helps promote regular emptying of the bladder. The primary goal is for the person to be able to control involuntary urination. If this is not possible, then the person may still at least be able to get to the bathroom in time to avoid accidents, because she will know when voiding is due to occur. The person’s care plan will note any special bladder training techniques that are being used and the nurse will instruct you on any specific duties you will be assigned as part of that training. https://youtu.be/98xMS9UquXY MEASURING URINE OUTPUT Urine output is a key indicator of fluid balance. In a person who is maintaining a good fluid balance, urine output is neither too high nor too low. Oliguria is the state of voiding a very small amount of urine over a given period of time (for example, voiding only 100 to 400 mL of urine over 24 hours). Oligmeans “few” and -uria means “urine.” A person who is dehydrated might become oliguric (that is, has a urine output that is well below normal). Polyuria (poly- means “many”) is excessive urine output. Polyuria, also known as diuresis, can be a sign of a health problem. For example, polyuria can be a symptom of poorly controlled diabetes. Or, polyuria may be the desired effect of a medication. For example, a person who is retaining excessive amounts of fluid (for example, as the result of a heart disorder) may be put on a medication called a diuretic to help rid the body of the extra fluid. The polyuria that results is a sign that the medication is having the desired effect. Evaluating a person’s urine output is also a good way to determine how well a person’s kidneys are working. Anuria (an- means “none”) is defined as the state of voiding less than 100 mL of urine over the course of24 hours. Anuria usually indicates that a person is in kidney failure. Not all of the people you care for will need to have their urine output measured and recorded, but people who have illnesses or take medications that may alter their body’s ability to maintain a healthy fluid balance will need to have their urine output measured regularly. Some people who are critically ill will have their urine output measured and recorded every hour, but most people in the health care setting have routine orders for their urine output to be measured and recorded each shift. If a person uses a regular toilet, you will need to remind the person to void into a specimen collection device (“commode hat”) and to call you after he or she has finished voiding so that you can measure and record the amount of urine. Specimen collection devices, urinals, and the drainage bags used with urinary catheters often have markings that make measuring urine output easy. If they do not, then the urine output can be measured by pouring it into a graduate. A graduate is also used to measure urine output if a person voids into a bedpan or bedside commode bucket. Remember to place the graduate on a flat surface when measuring urine so that your measurements are accurate. If the urine output of one of your residents or patients is being monitored, you will need to keep a record of the amount of urine passed at each voiding. Some intake and output (I&O) flow sheets will have spaces to record the amount of each individual voiding, while others may only have a space to record the end-of-shift amount. To obtain the end-of-shift amount, simply add the individual amounts together and record the total in the appropriate space. https://youtu.be/PypKGeRDe5A OBTAINING A URINE SPECIMEN Urinalysis, or examination of the urine under a microscope and by chemical means, is a commonly used diagnostic tool in the health care setting. Substances found in urine during urinalysis can help doctors diagnose kidney disease, certain metabolic diseases, and infections. The collection and analysis of urine over the course of 24 hours allows for evaluation of kidney function. To perform urinalysis, a urine specimen must be obtained. Depending on the situation, the method of collecting a urine specimen may vary. For routine urinalysis, no special collection procedures are necessary. The person is asked to urinate directly into the specimen cup, if possible. If this is difficult for the person, he or she can urinate into a specimen collection device , or into a bedpan or urinal. The person must not have a bowel movement at the same time the urine is being collected, or place toilet paper in the collection device, because these actions will change the urinalysis results. The urine is then poured from the collection device, bedpan, or urinal into the specimen cup. In some situations, it may be necessary to obtain a midstream (“clean catch”) urine specimen using a sterile specimen container. This method of collecting urine prevents contamination of the urine by the bacteria that normally live in and around the urethra. A midstream (“clean catch”) urine specimen is usually ordered when the doctor suspects a urinary tract infection. This way, if any bacteria are found in the urine sample, the doctor knows that they are the ones most likely responsible for the infection. When a midstream (“clean catch”) urine specimen is requested, the person is asked to clean the area around the urethral opening with a special cleansing wipe. The urine flow is started, then stopped, then started again. The urine sample is collected from the restarted flow. Your facility or agency may train you to do a type of routine urine testing that involves dipping chemically treated paper strips into a urine sample. Chemicals on the paper react with certain substances that may be found in the urine, causing the chemical blocks on the paper to change colour if these substances are present in the urine. The paper is then compared with a colour chart that comes with the strips, and the results are recorded in the person’s chart and reported to the nurse. https://youtu.be/dWE2jGv8-8E URINAL AND PROMOTING NORMAL ELIMINATION Urinals A man uses a urinal to urinate when he cannot get out of bed. The urinal is designed to fit between the man’s legs. To urinate, the man puts his penis in the opening of the urinal. If the man is very weak or disabled, you may need to place his penis inside the opening of the urinal for him. Promoting Normal Elimination Being in a health care facility can change a person’s normal elimination patterns, which can cause health problems. The most effective method of treating urinary and bowel problems is to prevent them from happening in the first place. As a nursing assistant, you can help promote normal urinary and bowel function for your patients or residents. The following tips are simple, but effective. ■ Encourage plenty of fluids, unless a person has a medical condition that requires fluid restriction. Drinking plenty of fluids helps the kidneys to work properly, and regular urination flushes harmful bacteria from the bladder, helping to prevent urinary tract infections. In addition, drinking enough fluids helps to keep the faeces soft, making bowel movements easier. ■ Answer call lights promptly and take people to the bathroom or provide them with a bedpan or urinal as soon as they ask you to. Many residents and patients do not want to “bother” the nursing staff and will wait until the last minute to call for assistance with the bedpan or for help getting to the bathroom. If the person must wait too long for help to arrive, he or she may have an accident. ■ Encourage your patients or residents to call when they first feel the urge to void. This can help to prevent accidents. In addition, “holding” urine or faeces is not only uncomfortable, it can lead to problems such as constipation. ■ Offer people the chance to eliminate frequently, especially if they are bedbound or require assistance. Some people may find it easier to accept an offer of assistance than to ask for help. ■ Provide for privacy and comfort. A person is able to urinate or have a bowel movement much more easily if she is warm enough, in a comfortable position, and ensured of as much privacy as possible. Most women urinate and have bowel movements in a sitting or squatting position. Help a woman to sit upright by elevating the head of the bed (if she is using a bedpan), or have her lean forward a bit while seated on the toilet or bedside commode. Most men stand up to urinate and sit down to have a bowel movement. Some men have no difficulty using a urinal while lying down, but others will need to sit up or even to stand. In this case, you may need to help the man to sit or stand up. If a person is having difficulty urinating, there are some things you can do to help. For example, try turning on the faucet and allowing water to run into the sink. The sound of running water, which accompanied many of our early toilet training lessons, can help a person relax enough to start the urine stream. The sound of the running water also helps to cover up the sounds of urination, which may put some people more at ease. Putting the person’s fingers in a basin of warm water can also help stimulate urination. If a person is having difficulty moving his bowels, make sure that the person does not feel rushed. Many people like to read while having a bowel movement. Some people find that drinking warm fluids Men who cannot get out of bed to urinate can use a urinal. Coffee, tea, or warm water with lemon helps stimulate the bowels to empty. Finally, regular exercise and foods that contain insoluble fibre help to promote regular bowel movements.