**{m**********|m******xm*******m***m***m***m***m***m***m***m
advertisement
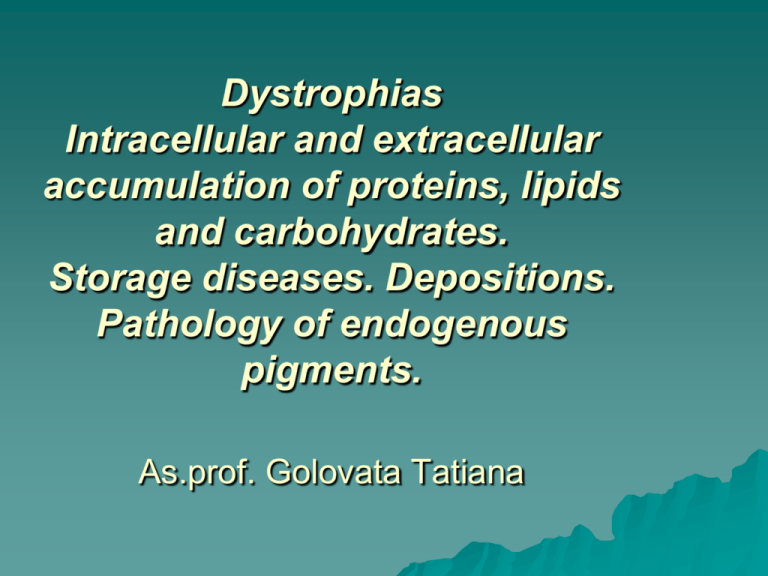
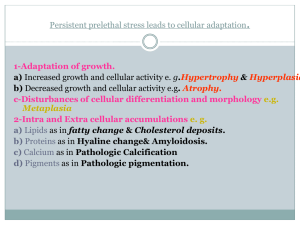
Dystrophias Intracellular and extracellular accumulation of proteins, lipids and carbohydrates. Storage diseases. Depositions. Pathology of endogenous pigments. As.prof. Golovata Tatiana Dystrophy (from the Greek. Dys-disorders and trophonutrition) - a quantitative and qualitative structural changes in the cells and / or intercellular substance of organs and tissues caused by violation of trophic. Morphological essence dystrophy Increase or decrease to-those of any matter contained in the body normally Changing the quality, and physical and chemical properties of substances The appearance of ordinary matter in unusual places The appearance and accumulation of new substances that are not inherent in the normal body Causes of abnormal accumulation of metabolic products 1. Pathology of cells-genetic or acquired defects of specific enzymes involved in the metabolism 2. Dysfunction of transport systems (disorders of blood circulation-hypoxia) 3. Violation endocrine and neural regulation of trophic. Mechanisms of abnormal accumulation of metabolic products Infiltration – ingestion of indigestible materials and accumulation of exogenous materials in cells. Mutations causing alterations in protein folding and transport. Perverse synthesis Decomposition - decay lipoprotein complexes. Classification of pathological accumulation of metabolic products According predominance violation of a particular type of exchange: a) protein, b) fat, c) hydrocarbons d) mineral For localization of the pathological process: a) intracellular (parenchymal) b) extracellular (stromal-vascular); c) mixed Depending on the influence of genetic factors: a) congenital b) acquired. For prevalence of the process: a) general, b) local. Intracellular Accumulations of proteins Accumulatios of proteins appear as rounded, eosinophilic droplets by denaturation and coagulation or vacuoles by hydration Intracellular Accumulations of proteins Pink hyaline droplets in the renal tubular epithelium Reabsorption droplets in proximal renal tubules are seen in renal diseases associated with protein loss in the urine. The process is reversible if the proteinuria diminishes, the protein droplets are metamolized and disappear. Intracellular Accumulations of proteins – hydropic swelling Caused hydration of hyaline droplets by different toxic action Intracellular Accumulations of proteins keratinization disorders Keratinization disorders refers to a large and heterogeneous group of disorders of cornification, the majority of which are genetically determined. Actually, the ichthyoses constitute the predominant portion of keratinisation disorders. The word « ichthyosis » derives from the Greek word « ichthys » which means fish. In most cases, the skin abnormalities appear since birth. Squamous cell carcinoma skin whith keratinization Keratin pearl (P) or eddy in squamous cell carcinoma Extracellular Accumulations of proteins – degenerations of connective tissue Mucoid swelling Fibrinoid swelling Hyalinosis Extracellular Accumulations of proteins – degenerations of connective tissue Mucoid swelling is a stromal dysproteinosis with superficial disorganization of protein in connective tissues with accumulation of basic substance glycoaminoglycan and their redistribution which cause the increasing of vessels permeability Mucoid Occasionally connective tissue appears to secret mucin Characterised by metachromasia Fibrinoid swelling It is a stromal vascular dystrophy defined by destruction of collagen fibers and basic substances with plasmorrhagia and formation of protein and polysaccharide complexes on fibrinoid substance Hyaline It is a stromal vascular dysproteinosis defined by alteration in the extracellular space which becomes homogenous, glossy, pink appearance in sections stained with haematoxylin and eosin Hyaline The term “hyaline” is used in many situations where degeneration is not a feature, e.g. glossy capsule of spleen, dense cartilage like valve Intracellular accumulation of lipids – fatty change This is accumulation of fat in non-fatty tissues, especially the parenchymatous organs, skeletal muscles and the heart, which have a high metabolic rate. Fatty change Development mechanism: Causative factor: cell poisons (bacterial, chemical e.g. alcohol) and clinical disorders (anaemia, cardiac failure, diabetes mellitus) → Reduced cellular enzyme activity → Inability to metabolise fat → Accumulation of fat in cells Fatty change In normal non-fatty tissues the intracellular fat is not visible by light microscopy using conventional fat stains. In fatty change, the accumulated fat is visualised using frozen sections, stained by Sudan III and indicated by bright orange vacuoles In routine paraffin sections the fat has been dissolved and is indicated by clear vacuoles Fatty change For example Fatty liver – organ is enlargement and yellow – “goose liver” A heart on the inside of which stripes of yellowish or white, tiger skin is simulated – “tiger heart”. Effect of fatty myocardium is cardiac failure Obesity Obesity is defined as a body mass index equal to or greater than 30. The main cause of obesity is increased intake of food. Manifestations: increased of adipose tissue in the fat depots Obesity Obesity must be distinguished from intra-cellular fatty change describe above. Gross degrees of obesity lead to increased adipose tissue in abnormal sites, e.g. between myocardial fibres. Metabolic disturbances of cholesterol Accumulation of cholesterol manifested histologically by intra-cellular vacuoles, are seen in several pathologic processes, e.g. atherosclerosis, xanthomas. STORAGE DISEASES - INBORN ERRORS OF METABOLISM Inborn errors of metabolism are single-gene defects resulting in the absence or deficiency of an enzyme or the synthesis of a defective protein. Inborn errors of metabolism have four possible consequences: accumulation of an intermediate metabolite (e.g. homogentisic acid in alkaptonuria) deficiency of the ultimate product of metabolism (e.g. melanin in albinos) synthesis of an abnormal and less effective end product (e.g. haemoglobin S in sickle cell anaemia) failure of transport of the abnormal synthesised product (e.g. α1-antitrypsin deficiency). Disorders of carbohydrate metabolism The commonest disorder of carbohydrate metabolism with an inherited component in its aetiology is diabetes mellitus. Histological manifestations: reduce glycogen content in traditional depot, e.g. in the liver accumulation in abnormal places, e.g. in the renal tubular epithelium TISSUE DEPOSITIONS - Amyloid In this condition, a 'waxy' substance composed essentially of an abnormal protein is deposited in the extracellular tissues, particularly around the supporting fibres of blood vessels and basement membranes. Amyloid is resistant to degradation and removal by the usual process so that the deposition progresses relentlessly. Detection of Amyloid Amyloidosis of the kidney. sections stained Congo Red Amyloidosis of the adrenal. sections stained Congo Red CLASSIFICATION of Amiloidosis Pathological effects Calcification - Abnormal deposits of calcium salts occur in two circumstances: dystrophic and metastatic. Dystrophic calcification occurs in tissue already affected by disease. Common examples are: atheromatous plaques calcification of mitral valve ring old tuberculous lesions fat necrosis old thrombi necrotic tissue dead parasites Calcification Metastatic calcification is much less common than dystrophic calcification and occurs as a result of hypercalcaemia. Frequent causes are: hyperparathyroidism Pathology of endogenous pigments. Melanin pigmentation Local melanin pigmentation This is seen in tumor derived from the melanocytes of the skin and choroid cost of the eye Pathology of endogenous pigments. Melanin pigmentation Generalised melanin pigmentation (melanosis) is a characteristic of this condition which involves the destruction of the adrenals, adrenal thus remuving the inhibitory adrenal control. Pigmentation is seen on exposed skin surfaces, and those subject to local irritation including squamous mucous surfaces such as the mouth. Pathology of endogenous pigments. Iron-containing pigment - haemosiderin It is iron derived from red cells breakdown is held in the spleen, liver and marrow. When the amount of iron within the cells becomes excessive and overloads the ferritin system, it is deposited in a brown granular form – haemosiderin. This occurs in two situations: 1. Local breakdown of red cells in tissues e.g. in internal haemorrhage. 2. Visceral siderosis – this is seen in the liver, spleen in cases of haemolytic anaemia, and in blood transfusion. Iron is found in the liver parenchyma. Easily demonstrated by the Prussian Blue reaction. Pathology of endogenous pigments. Lipofuscin This is yellowish brown pigment having a high lipid content, often found in the atrophied cells of old age – “wear and tear” pigment. It is particularly common in the heart muscle around nucleus. Pathology of endogenous pigments. Iron-free pigment - Bilirubin 1. 2. 3. When the bilirubin content of the serum rises above 34 μmol/l, jaundice appears. This can be brought about by an abnormality in one of main ways: Post - hepatic (obstructive) jaundice Pre- hepatic jaundice Hepato-cellular jaundice Thank you for your attention