Introduction to Physical Assessment
advertisement

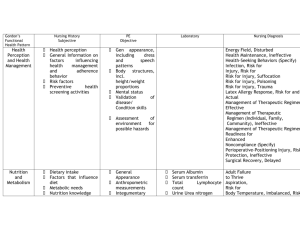
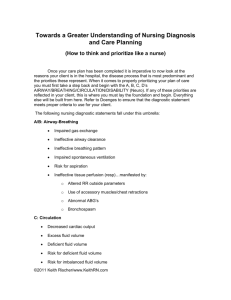
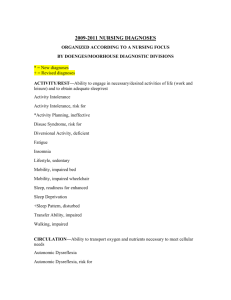
Physical Assessment An Overview J. Carley RN, MSN, MA, CNE Fall, 2009 You’re Late ! Let’s Start Report…. Rm. 3A: Rm. 4A: Rm. 5A: Rm. 6A: Rm. 7A: Velma Aguon 76 y.o. P.I.-Am. Female DX: Hypertensive Crisis Mike Smithe 32 y.o. Afr-Am Male Julian Reilly 44 y.o. Cauc. Male DX: Pericarditis Ashley Wilkes 26 y.o. Cauc. Female DX: Mitral Stenosis Emsley Owens 72 y.o. Afr-Am Male DX: CHF DX: R/O M.I., HTN RN’s Comment: “Oh, *&%$#!!!” “New Admission” Rm. 8A: Rm. 9A: Rm. 10A: Rm. 11A: Rm. 12A: Redd Butler 56 y.o Cauc. DX: Cardiomyopathy, CHF Faith Hopee 78 y.o. N.A. Female DX: A- Fib Frank Arbugast 18 y.o. Afr-Am Male Aubrey Embry 38 y.o. J.A. Female DX: Endocarditis Yolanda Zahara 55 y.o. M.E. A. Female DX: Sickle-Cell Cr. DX: Buerger’s Disease mnemonic “A-D-O-P-I-E” Nursing Process Assessment Diagnosis Outcome Identification Planning Intervention Evaluation List of NANDA Nursing Diagnoses Content and Process of This Course ! The Nursing Process • A Closer Look Assessment Collect Data: √ Review the Clinical Record √ Interview √ Health History √ Physical Examination √ Functional Assessment √ Consultation * Review of the Literature (--Evidence Based Practice) Diagnosis *Interpret Data: √ Identify clusters / cues √ Make Inferences * Validate Inferences * Compare clusters of cues w/ definition, defining characteristics * Identify Related Factors * Document the nursing diagnosis Outcome Identification --Identify expected outcomes --INDIVIDUALIZE to the person --Realistic and MEASURABLE --Include a TIME FRAME Planning --Establish priorities --Develop Outcomes --Set time frames for outcomes --Identify Interventions --Document Plan of Care “The Nursing Care Plan” Implementation --Review planned interventions --Schedule & coordinate patient’s care --Collaborate w/ other team members --Supervise implementation by delegation --Counsel patient & family --Involve the patient in their care --Referrals as need for continuity of care --Document care provided Evaluation --Refer to the outcomes you established --Evaluate individual’s condition: compare actual outcomes to expected outcomes --Summarize results of the evaluation --If expected outcomes not met, identify reasons --Modify Plan of Care as necessary --Document Evaluation of Outcomes, and changes (if any) in Plan of Care Nursing Process Assessment Diagnosis Outcome Identification Planning Intervention mnemonic “A-D-O-P-I-E” Evaluation Subjective Data Objective Data Objective Data: • • • • • Blood Pressure = 142 / 98 mm Hg Weight = 158 lbs (= 71.8 kg) Oral Intake = 2400 mL / 24 hours Urinary Output = 250 mL / 24 hours Imbalance Between Oral Intake & Urinary Output (above) The Interview “Yes.” “Uh Huh.” “I see…” The Interview • During the interview, it is a chance for the patient to tell you how he or she PERCEIVES what is going on—what they THINK (or want you to think) their health state is… U2: Your Blue Room http://www.youtube.com/watch?v=xS4hJabqRc4 Learning Games http://www.quia.com/rr/501084.html http://www.quia.com/rr/503611.html http://www.quia.com/cm/362353.html http://www.quia.com/jg/1698754.html http://www.quia.com/cm/347615.html?AP_rand =1379420649 Part 2: Interviewing & Documentation The Nursing Interview “The Nursing Process…” • Mnemonic: “ADOPIE” = “The Nursing Process” Assessment Diagnosis Evaluation Outcome Identification Implementation Planning Establish Rapport • • • • • • Get organized Do not rely on memory Plan enough time Ensure privacy Get focused Be calm, confident, warm, and helpful Begin the Interview • Give your name and position • Verify the client’s name • Briefly explain your purpose How to listen • • • • Be an empathetic listener Use short supplementary phrases Listen for feelings as well as words Let the person know when you see body language that conflicts with what they say • Be patient if the patient has a memory block • Avoid the impulse to interrupt • Allow for pauses How to ask Questions • Ask about the main problem first = chief complaint • Focus your questions to gain specific information about the signs and symptoms • Don’t lead the witness • Restate the other person’s words to clarify • Use open-ended questions • Avoid closed –ended, yes or no questions How to terminate the interview • • • • • • If the session has been long, give a warning As the person to summarize their primary concerns Ask if there are other areas to be discussed Offer yourself as a resource Explain routines and provide information about who does what End on a positive note Charting & Documentation • • • • • • • If it isn’t written, then it wasn’t done Chart at the time it occurs – if possible Follow facility guidelines Is the information clear and logical? Is it true? Is it non - judgmental? Record all abnormals and normals Charting guidelines • • • • • • Be precise Stick to the facts Sign your name after each entry SOAP format – focuses on specific problems AIR, DAR, PIE, DIE formats – focus on nursing interventions and client response Prioritize the client problems Part Two: Complete Health History • • • • • Biographical Data Reasons for Seeking Health Care History of Present Health Concern Past Health History Family Health History Lifestyle and Health Practices Profile • • • • • • • Description of Typical Day Nutrition and Weight Management Activity Level and Exercise Sleep and Rest Medication and Substance Use Self-Concept Self-Care Responsibilities NANDA Nursing Diagnosis List Activity Intolerance Activity Intolerance, Risk for Airway Clearance, Ineffective Anxiety Anxiety, Death Aspiration, Risk for Attachment, Parent/Infant/Child, Risk for Impaired Autonomic Dysreflexia Autonomic Dysreflexia, Risk for Blood Glucose, Risk for Unstable Body Image, Disturbed Body Temperature: Imbalanced, Risk for Bowel Incontinence Breastfeeding, Effective Breastfeeding, Ineffective Breastfeeding, Interrupted Breathing Pattern, Ineffective Cardiac Output, Decreased Caregiver Role Strain Caregiver Role Strain, Risk for Comfort, Readiness for Enhanced Communication: Impaired, Verbal Communication, Readiness for Enhanced Confusion, Acute Confusion, Acute, Risk for Confusion, Chronic Constipation Constipation, Perceived Constipation, Risk for Contamination Contamination, Risk for Coping: Community, Ineffective Coping: Community, Readiness for Enhanced Coping, DefensiveCoping: Family, Compromised Coping: Family, Disabled Coping: Family, Readiness for Enhanced Coping (Individual), Readiness for Enhanced Coping, IneffectiveDecisional Conflict Decision Making, Readiness for Enhanced Denial, Ineffective Dentition, Impaired Development: Delayed, Risk forDiarrhea Disuse Syndrome, Risk for Diversional Activity, Deficient Energy Field, Disturbed Environmental Interpretation Syndrome, Impaired Failure to Thrive, Adult Falls, Risk for Family Processes, Dysfunctional: Alcoholism Family Processes, Interrupted Family Processes, Readiness for Enhanced FatigueFearFluid Balance, Readiness for Enhanced Fluid Volume, Deficient Fluid Volume, Deficient, Risk for Fluid Volume, Excess Fluid Volume, Imbalanced, Risk for Gas Exchange, Impaired Grieving Grieving, Complicated Grieving, Risk for Complicated Growth, Disproportionate, Risk for Growth and Development, Delayed Health Behavior, Risk-Prone Health Maintenance, Ineffective Health-Seeking Behaviors (Specify) Home Maintenance, Impaired Hope, Readiness for Enhanced Hopelessness Human Dignity, Risk for Compromised Hyperthermia Hypothermia Immunization Status, Readiness for Enhanced Infant Behavior, Disorganized nfant Behavior: Disorganized, Risk for Infant Behavior: Organized, Readiness for Enhanced Infant Feeding Pattern, Ineffective Infection, Risk for Injury, Risk for Insomnia Intracranial Adaptive Capacity, Decreased Knowledge, Deficient (Specify) Knowledge (Specify), Readiness for Enhanced Latex Allergy Response Latex Allergy Response, Risk for Liver Function, Impaired, Risk for Loneliness, Risk for Memory, Impaired Mobility: Bed, Impaired Mobility: Physical, Impaired Mobility: Wheelchair, Impaired Moral Distress Nausea Neurovascular Dysfunction: Peripheral, Risk for Noncompliance (Specify) Nutrition, Imbalanced: Less than Body Requirements Nutrition, Imbalanced: More than Body Requirements Nutrition, Imbalanced: More than Body Requirements, Risk for Nutrition, Readiness for Enhanced Oral Mucous Membrane, Impaired Pain, Acute Pain, Chronic Parenting, Impaired Parenting, Readiness for Enhanced Parenting, Risk for Impaired Perioperative Positioning Injury, Risk for Personal Identity, Disturbed Poisoning, Risk for Post-Trauma Syndrome Post-Trauma Syndrome, Risk for Power, Readiness for Enhanced Powerlessness Powerlessness, Risk for Protection, Ineffective Rape-Trauma Syndrome Rape-Trauma Syndrome: Compound Reaction Rape-Trauma Syndrome: Silent Reaction Religiosity, Impaired Religiosity, Readiness for Enhanced Religiosity, Risk for Impaired Relocation Stress Syndrome Relocation Stress Syndrome, Risk for Role Conflict, Parental Role Performance, Ineffective Sedentary Lifestyle Self-Care, Readiness for Enhanced Self-Care Deficit: Bathing/Hygiene Self-Care Deficit: Dressing/Grooming Self-Care Deficit: Feeding Self-Care Deficit: Toileting Self-Concept, Readiness for Enhanced Self-Esteem, Chronic Low Self-Esteem, Situational Low Self-Esteem, Risk for Situational Low Self-Mutilation Self-Mutilation, Risk for Sensory Perception, Disturbed (Specify: Auditory,Gustatory, Kinesthetic, Olfactory Tactile,Visual) Sexual Dysfunction Sexuality Pattern, Ineffective Skin Integrity, Impaired Skin Integrity, Risk for Impaired Sleep Deprivation Sleep, Readiness for Enhanced Social Interaction, Impaired Social Isolation Sorrow, Chronic Spiritual Distress Spiritual Distress, Risk for Spiritual Well-Being, Readiness for Enhanced Spontaneous Ventilation, Impaired Stress, Overload Sudden Infant Death Syndrome, Risk for Suffocation, Risk for Suicide, Risk for Surgical Recovery, Delayed Swallowing, Impaired Therapeutic Regimen Management: Community,Ineffective Therapeutic Regimen Management, Effective Therapeutic Regimen Management: Family,Ineffective Therapeutic Regimen Management, Ineffective Therapeutic Regimen Management, Readiness for Enhanced Thermoregulation, Ineffective Thought Processes, Disturbed Tissue Integrity, Impaired Tissue Perfusion, Ineffective (Specify: Cerebral,Cardiopulmonary, Gastrointestinal, Renal) Tissue Perfusion, Ineffective, Peripheral Transfer Ability, Impaired Trauma, Risk for Unilateral Neglect Urinary Elimination, Impaired Urinary Elimination, Readiness for Enhanced Urinary Incontinence, Functional Urinary Incontinence, Overflow Urinary Incontinence, Reflex Urinary Incontinence, Stress Urinary Incontinence, Total Urinary Incontinence, Urge Urinary Incontinence, Risk for Urge Urinary Retention Ventilatory Weaning Response, Dysfunctional Violence: Other-Directed, Risk for Violence: Self-Directed, Risk for Walking, Impaired Wandering YOUR TOPIC GOES HERE • Your Subtopics Go Here TRANSITIONAL PAGE Backdrops: www.animationfactory.com - These are full sized backdrops, just scale them up! - Can be Copy-Pasted out of Templates for use anywhere!