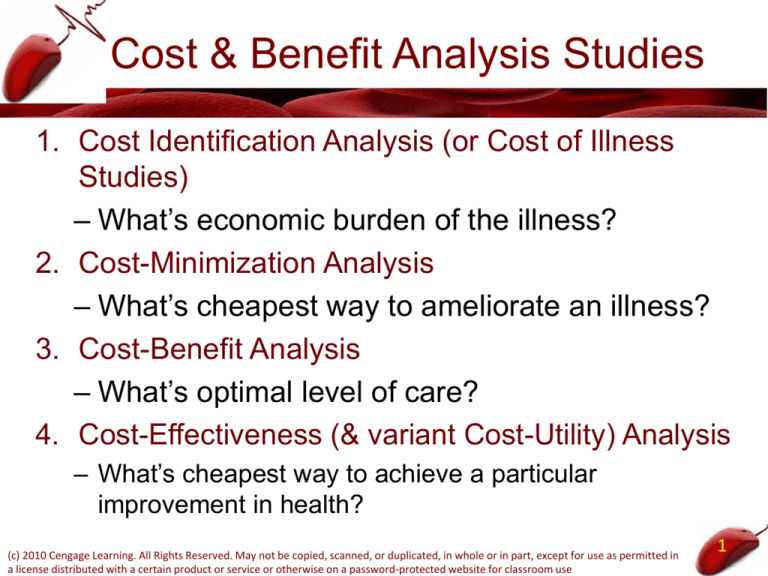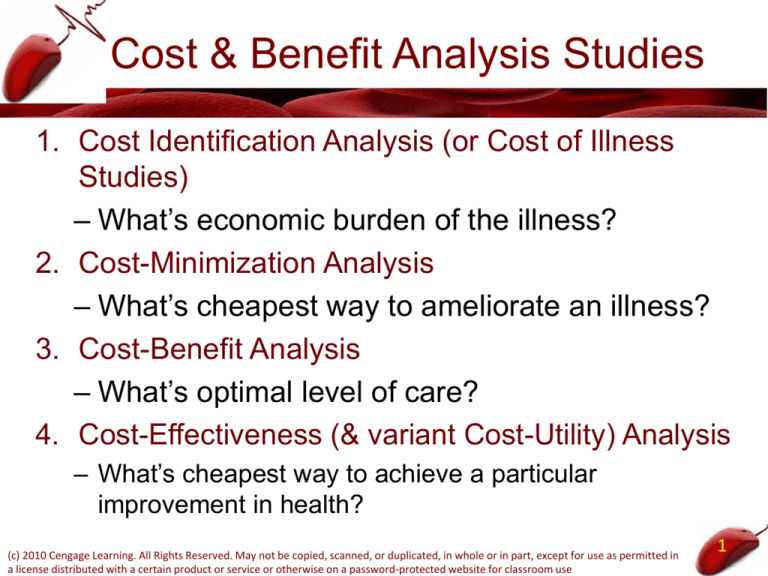
Cost & Benefit Analysis Studies
1. Cost Identification Analysis (or Cost of Illness
Studies)
– What’s economic burden of the illness?
2. Cost-Minimization Analysis
– What’s cheapest way to ameliorate an illness?
3. Cost-Benefit Analysis
– What’s optimal level of care?
4. Cost-Effectiveness (& variant Cost-Utility) Analysis
– What’s cheapest way to achieve a particular
improvement in health?
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
1
I. Cost Identification Analysis
• Cost identification studies
– Measure the total cost of a given medical
condition or type of health behavior on the
overall economy
• Total cost - three major components:
1. Direct medical care costs
2. Direct nonmedical costs
3. Indirect costs
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
2
Cost Identification Analysis
• Direct medical care costs
– Incurred by medical care providers
• Hospitals, physicians, and nursing homes
– All necessary medical tests and examinations
– Administering medical care
– Any follow-up treatments
• Direct nonmedical costs
– All monetary costs imposed on any nonmedical care
personnel, including patients
• Transportation to and from the medical care provider
• Home care; specific dietary restrictions
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
3
Cost Identification Analysis
• Indirect costs
– Time costs associated with implementation of
the treatment
– Opportunity cost of the patient’s (or anyone
else’s) time that the program affects
• Lost productivity (& wages) to economy
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
4
Cost Identification Analysis
• Behan & Cox (2011)
– Total Cost of Obesity in US & Canada in 2009
• $300 Billion
– $128 Billion in Medical Costs
– $172 Billion in costs from excess disability and mortality
• Sobocki et al. (2006)
– Cost of depression in Europe
• 118 billion euros (Direct costs = 42 billion euros)
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
5
Cost Identification Analysis
• Dall et al (2010)
– Direct and indirect costs of diabetes in 2007
• $218billion
– $153 billion direct medical costs
– $65 billion indirect expenses such as lost work days and
permanent disability
• The American Heart Association
– Cost of cardiovascular disease and stroke
• $448.5 billion in 2008
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
6
II. Cost-Minimization Analysis
• Identifies which alternative treatment has
the lowest cost
– Is laparoscopic hysterectomy less costly than
standard surgery
– Is kidney transplant less costly than dialysis for
end stage renal disease
– Is repositioning and mobilization less costly
than special dressings and ointments for
treating pressure ulcers in hospital (8% patients
get them still)
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
7
Cost Minimimization Analysis
• Coast et.al. (1998)
– Cost of hospital in the home care in UK was
25% less than full hospital care
• Loubeau, Loubeau & Jantzen (2001
– Breakeven point for kidney transplant vs.
dialysis is 39 months.
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
8
III. Cost-Benefit Analysis
• Objective #1: Assess whether the Total
Benefits of health care activity are greater
than the Total Costs
• Objective #2: Assess whether the Total
Benefit/Total Cost ratio for differing types of
care are equal
• Objective #3: find the level of health care
activity that maximizes net benefits to
society
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
9
Cost-Benefit Analysis
• Similar decision making process as finding
the level of production that maximizes net
profit to a business
• TNSB = TSB – TSC
– TSB - total social benefit in consumption
• Money value of the satisfaction generated from
consuming the god or service
– TSC - total social cost of production
• Money value of all the resources used in producing
the good or service
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
10
Cost-Benefit Analysis
• TNSB from medical services
TNSB(Q) = TSB(Q) - TSC(Q)
– Q – quantity of medical services
• Maximize TNSB(Q)
– Choose Q at which the difference between TSB
and TSC reaches its greatest level
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
11
FIGURE 3–1
Determination of the Efficient Level of Output
The TSC curve represents the TSC of producing medical care and is upward sloping because total
costs increase as more medical care is produced. The curve bows toward the vertical axis because
the marginal cost of producing medical care increases as more medical care is produced.
TSC
Costs and
benefits
of medical
services
TSB
A
B
0
Q0
The TSB curve represents the monetary
value of the total social benefit
generated from consuming medical
care. The curve is positively sloped to
reflect the added monetary benefits
that come about by consuming more
medical care. The curve bows
downward to capture the fact that
society experiences diminishing
marginal benefit with regard to medical
care.
Quantity of medical services (Q)
TNSB is maximized when the vertical distance between the two curves is greatest and that occurs
at Q0 level of medical services.
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
12
Cost-Benefit Analysis
• TSB - increase at a decreasing rate
– Diminishing marginal benefit
• Successive incremental units of medical services
generate continually lower additions to social
satisfaction
– Slope: MSB(Q) = ΔTSB/ΔQ
• MSB - marginal social benefit from consuming a unit
of medical services
• MSB decreases with quantity since the slope of the
TSB curve declines due to diminishing marginal
benefit
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
13
Cost-Benefit Analysis
• TSC - increase at an increasing rate
– Increasing marginal costs of producing medical
services.
– Slope: MSC(Q) = ΔTSC/ΔQ
• MSC - marginal social cost of producing a unit of
medical services
• MSC increases with output as the slope of the TSC
curve gets steeper due to increasing marginal cost
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
14
Cost-Benefit Analysis
• Maximize TNSB
– Slope of TSB = slope of TSC
– MSB(Q) = MSC(Q)
– At output level Q0
• Allocative efficiency - best quantity of medical
services
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
15
Cost-Benefit Analysis
• MSB curve - negatively sloped
– Diminishing marginal benefit
• MSC curve - positively sloped
– Increasing marginal costs, respectively
• Efficient amount of medical services: Q0
– Where MSB = MSC
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
16
FIGURE 3–2
Under- and Overprovision of Medical Services
Costs and
benefits
of medical
services
The MSC curve stands for the marginal social cost of producing medical care and is
upward sloping because of increasing marginal costs.
A
MSC
G
E
C
H
F
B
MSB
QL
Q0
TNSB is maximized at Q0 level of medical
care where the two curves intersect. At
that point, the MSB of consuming medical
care equals the MSC of production.
The MSB curve stands for the marginal
social benefit generated from
consuming medical care and is
downward sloping because of the
notion of diminishing marginal benefit.
QR Quantity of medical services (Q)
If QL amount of medical care is produced, then the MSB exceeds the MSC and society would be better
off if more medical services were produced. If QR amount of medical care is produced, then the MSB is
less than the MSC and too much medical care is produced.
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
17
Cost-Benefit Analysis
• TNSB
– Area below MSB curve but above MSC curve
• Sum of net marginal social benefits
– Area ABC = maximum TNSB that society
receives if resources are allocated efficiently
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
18
Cost-Benefit Analysis
• For QL < Q0 : MSB > MSC
– Too few medical services are being produced
– Deadweight loss: ECF
• Lost amount of net social benefits
• Cost associated with an underallocation of resources
to medical services
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
19
Cost-Benefit Analysis
• For QR > Q0 : MSC > MSB
– Too many medical services are being produced
– Deadweight loss GCH
• Net cost to society from producing too many units of
medical services and therefore too few units of all
other goods and services.
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
20
Cost-Benefit Analysis
• NMSB(Q) = MSB(Q) - MSC(Q)
– NMSB - net marginal social benefit the society
derives from consuming a unit of the good
• If NMSB > 0
– Total net social benefit increases if an additional
unit of the good is consumed
• If NMSB < 0
– Society is made worse off if an additional unit of
the good is produced and consumed
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
21
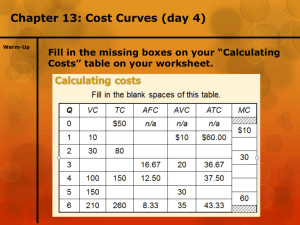
Cost Benefit Number Example
No. of
Flu Shots
0
1000
2000
3000
4000
5000
Total Marginal Decline in Total Marginal Net
Costs Costs Illnesses Benefits Benefits Benefits
40K
--0
0
0
60K
20
1500
150K
150
90K
80K
20
3000
300K
150
220K
100K
20
3600
360K
60
260K
120K
20
3900
390K
30
270K
140K
20
4000
400K
10
260K
Note: assume each illness prevented generates $100 in extra benefits
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
22
Steps for Cost/Benefit Analysis
• Must identify two relations
– Health Production Function, i.e., how does
medical care influence health
• Benefits from improvement in health must be
“monetized” to dollar benefits
• More years worked, less suffering, less future health
care spending
– Medical Care Production Function, i.e., what
are the costs of differing levels of care
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
23
Practical Issues of Using Cost-Benefit
Analysis
• What are the opportunity costs of medical
care?
• Benefits in future must be discounted to
today’s $
• Quality differences in health inputs/outputs
are difficult to measure & compensate for
• How to place a dollar value on better health,
e.g., value of saved life, less pain &
suffering
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
24
Human capital approach
• Many medical interventions
– Extend or improve the quality of life
• Human capital approach
– Value of a life = the market value of the output
produced by an individual during his or her
expected lifetime
– Estimate the discounted value of future
earnings resulting from an improvement in or
an extension of life
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
25
FIGURE 3–3
Present value of lifetime earnings, males & females, 2000
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
26
Human capital approach
• Present value of lifetime earnings
– Initially increases with age
• Value of lifetime earnings that accrue mainly in the
middle adult years are discounted over a shorter
period of time
– Peak - between the ages of 20 and 24
– Then decreases with age
• Productivity and number of years devoted to work
decrease
– Sensitive to the discount rate
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
27
Human capital approach
• Shortcomings
– Unable to control for labor market imperfections
• Gender, racial, other forms of discrimination
– Doesn’t take into account
• Value of any pain and suffering averted because of a
medical treatment
• Value an individual receives from the pleasure of life
itself
– A chronically unemployed person
• Has a zero or near-zero value of life
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
28
Willingness-to-pay approach
• Willingness-to-pay approach
– How much money people are willing to pay for
reductions in the probability of dying, injury
• Labor market wage differences – how much extra do
dangerous jobs have to pay to induce workers to risk
their lives?
• Consumer safety purchases – how much do people
spend to avert deaths and avert injury
• Survey data – how much do people say they would
pay to avoid death or injury
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
29
• Willingness to Pay Evidence
– From wage differences, value of life saved = .6
mil to 16.2 mil.
– From consumer purchases, value of life saved
= .07 mil. to 4 mil. (smoke detector spending,
auto safety devices)
– From surveys, value of life saved = 1 mil to 15.6
mil.
• Although wide range, upper bound is
around $16 million or so per life saved
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
30
Value of Saved Life
Willingness to Pay Basis
($1000s)
Desire for prompt coronary care
66
Auto air bag purchases
360
Smoke detector purchases
370
EPA sulfur scrubbers
500
Seat belt use
540
Law enforcement
850
EPA water radium regs
2500
Dangerous factory wages
3200
OSHA safety rules
3500
Premium tire purchases
3600
Airline safety rules
11800
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
31
Some Estimates of the Value of Life in the US
The following estimates have been applied to the value of life when
using cost-effectiveness analysis. The estimates are either for one
year of additional life or for the statistical value of a single life.
•$50,000 per year of quality life (international standard most private
and government-run health insurance plans worldwide use to
determine whether to cover a new medical procedure)[5]
•$129,000 per year of quality life (based on analysis of kidney
dialysis procedures by Stefanos Zenios and colleagues at Stanford
Graduate School of Business)[5]
•$9.1 million (Environmental Protection Agency, 2010)[6]
•$7.9 million (Food and Drug Administration, 2010)[6]
•$9.4 million (Transportation Department, 2015)[7]
•$9.1 million (Prof. W. Kip Viscusi, Vanderbilt University, 2013)[8]
32
Maybe Willingness to Pay Understates Value of Life?
Difference between Statistical Life and Identified Life
• Tirhas Habtegiris was a 27 year old woman on a ventilator dying of
cancer in a Baylor TX hospital in 2005. No hope for recovery & no
money or insurance.
• Family in Africa informed on 12/1/15 that she would be unplugged if
not transferred. No other hospital would accept so on 12/12/15 she
was unplugged despite family wishes to keep her alive until they
could arrive from Africa.
• Texas law allows hospitals to discontinue care should the attending
physician believe it’s inappropriate and futile.
• Took 16 minutes to die. Whether she was conscious is in debate
with hospital claiming large doses of narcotics made her
unconscious.
• Question: was decision to unplug correct from MB vs. MC view?
Maybe not. Statistical lives can be really cheap according to
willingness to pay (e.g., communities won’t build guardrail for $200K
that saves a life a year).
• But people who “identify” with the life will raise a lot of money to save
particular people. So statistical life understates value of life.
Willingness-to-pay approach
• πˣ V = C
• V=C/π
– Value of the human life lower-bound estimate
• Advantage
– Measures the total value of life and not just the
job market value
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
34
Should College Students Be
Vaccinated?
• Meningococcal disease
• Jackson et al. (1995)
– Cost-benefit analysis – policy to vaccinate all
college students
– Benefits - from a decrease in the number of
cases of meningococcal disease
– Cost of implementing a vaccination program for
all college students
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
35
Should College Students Be
Vaccinated?
• Costs
– Cost of the vaccine ($30) multiplied by the
number of doses needed
• 2.3 million freshmen
• 80% receive the vaccine
– Estimated cost of any side effects
• One severe reaction per 100,000 students
vaccinated ($1,830 per case)
– $56.2 million a year
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
36
Should College Students Be
Vaccinated?
• Benefits include
– Medical costs diverted
• Treatment costs per case = $8,145
• Costs for cases occurring in the 2nd, 3rd, and 4th
years of college - discounted at 4%
• $3.1 million at 15 times the baseline rate
– Estimated value of lives saved
• Human capital approach - value of lost earnings
• Each life saved =$1 million
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
37
TABLE 3–1
Estimated Benefits and Costs for the Vaccination of College
Students against Meningococcal Disease (in millions of $)
Incidence would Incidence would
double w/o
be 15X w/o
vaccine
vaccine
Cost of the Vaccination Program
Total Benefits
Direct Medical Benefits
Indirect Benefits—Value of Lives Saved
$56.2
9.3
0.5
8.8
$56.2
63.8
3.1
60.7
Net Benefits—(Benefits – Cost)
-46.9
7.6
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
38
Should College Students Be
Vaccinated?
• Estimated costs, baseline times 2
– Outweigh the benefits by more than $46 million
• Net benefits, baseline times 15
– $7.6 million.
• Estimated possible rate: 2.6 times
– Costs outweigh the benefits
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
39
Should school kids (5-18) be vaccinated for flu?
(Jordana. S. et al. 2008)
• Costs per household = $36
– Acquisition, Administration and Adverse events
• Benefits per household = $208
– Direct – outpatient, hospitalization, Rx, OTC $105
– Indirect – productivity loss, time costs due to illness
$103
• Net Benefits per household = $172
• Benefits/Costs per household = $208/36 = 5.8
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
40
Costs and Benefits of New Medical
Technologies
• Advances in medical technology
– Driving force behind rising medical costs
– Profound effect on health and well-being of
millions of people
• Overall mortality & disability rates in the United
States have fallen consistently since World War II.
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
41
Costs and Benefits of New Medical
Technologies
• Impact of medical technology on health
– Total product curve for medical care
• Relationship between health and amount of medical
care consumed
– New medical technology - improves health
• Total product curve - rotates upward
• Each unit of medical care consumed now has a
greater impact on overall health
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
42
Costs and Benefits of New Medical
Technologies
• Cutler and McClellan (2001)
– Benefits outweigh the costs
– Heart attack
• 1984 – 1998: increase life expectancy by 1 year
• Net benefit: $60.000; Payoff 7 to 1
– Low-birthweight infants
• Net benefits = $200,000 per infant; Payoff 6 to 1
– Depression
– Cataracts
– Breast cancer
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
43
Cost-Effectiveness Analysis
• Cost-effectiveness analysis CEA
– Health care benefits are often long-term and
intangible, making them difficult to monetize.
– CEA doesn’t try to monetize benefits
– Typically it shows the marginal cost of
producing a life year saved or the marginal cost
of averting a death for differing treatments
– Basically a Marginal Cost/Marginal Benefit
calculation
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
44
Autologous Blood Donations Are They
Cost Effective?
• Autologous blood donation
– Donor and recipient are the same person
• Allogeneic blood donation
– Donor and recipient are different people
• Autologous blood donation
– Safer
– More costly
• More administrative and collection expenses
• Higher discarding costs
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
45
TABLE 3–3
Estimated Cost Effectiveness of Autologous Blood Donations
Total Hip
Coronary-artery
Replacement Bypass grafting
Abdominal
Hysterectomy
Transurethral
Prostatectomy
$68
$107
$594
$4,783
Life Years Saved per
unit transfused
0.00029
0.00022
0.00044
0.00020
Cost effectiveness
(row one/row two)
$235,000
$494,000
$1,358,000
$23,643,000
Additional cost
per unit of autologous
blood transfused
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
46
Cost Effectiveness Study Findings
• Medicaid mandate (1990) that all states
provide prenatal care to <133% poverty
women
– insured increased from 12% (1979) to 43%
(1992)
– Medicaid cost/client increased $224
– Infant mortality decreased from 11.5 to 8.5%
– Marginal cost per life save = $840K
– Pretty cheap
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
47
• Joyce et al explain 75% decrease in
neonatal mortality (1950 – 1996) as due to
– Increased teen family planning (.6 lives per
1000 participants)
– Increased neonatal ICUs (2.8 lives per 1000
participants)
– Increased prenatal care (4.5 lives per 1000
participants)
– Cost for each 1000 extra participants are 122K,
13.6 mil. and 176K
– MC/MB (cost per life saved) are 203K, 4.8 mil.
and 39K, respectively. Prenatal care cheapest!
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
48
• Other estimates
– Annual Spiral CT scanning costs 116K per life
year saved for heavy smokers & 2.3 mil. For
ex-smokers (vs. traditional chest x-rays)
– Simvastatin to person diagnosed with heart
disease costs 5-10K per LYS
– Cost effectiveness of annual breast cancer
screening (mammogram)
• Age 50-69, cost per year of life saved = $21,400
• Age 40-49, incremental cost-effectiveness ratio =
$105,000 per life-year saved
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
49
• Hillary Clinton Care (1994)
– Proposed universal coverage including:
– only biannual mammograms for +50 women with a
differing estimated cost-effectiveness ratio of $105K per
life year. Not for 40-49 year olds where costeffectiveness ratio was estimated to be $190K per life
year saved. Spending $190K for one year of life wasn’t
worth it but $105K OK?
– Only once every 4 year PAP smears would be covered
with a MC/MB of $12K per life year saved. Not more
frequently because MC/MB increases rapidly ($220K
for 3 years and $310K for 2 years).
50
Cost-Utility Analysis (CUA)
• Critics of CEA: life-years are not always the
same for differing treatments
– Some care leads to many life-years but poor
quality of life
– Other care leads to few life-years but greatly
enhanced quality of life
– Cost-utility analysis (CUA) estimates the benefit
side in terms of life-years saved adjusted for
quality of well-being
– 1 = perfect health and 0 = death
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
52
• Calculates the marginal cost per quality
adjusted life year (or life saved)
– Calculated rank for all medical services
– MCQALYS = Marginal Cost/Marginal
Benefit/QWB where Benefit is LYS after
treatment and QWB ranges from 0 to 1
– E.G. Jogging from 30-60 prevents 78.1
coronary heart disease events and produces
1138 QALYS (adjusted by QWB = .8) yielding
MCQALYS of $11300
– Treating mild angina = MCQALYS of $40K
– Treating hypertension = MCQALYS of $25-65K
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
53
• Calculates the marginal cost per quality
adjusted life year (or life saved)
– Calculated rank for all medical services
– MCQALYS = Marginal Cost/Marginal
Benefit/QWB where Benefit is LYS after
treatment and QWB ranges from 0 to 1
– E.G. Jogging from 30-60 prevents 78.1
coronary heart disease events and produces
1138 QALYS (adjusted by QWB = .8) yielding
MCQALYS of $11300
– Treating mild angina = MCQALYS of $40K
– Treating hypertension = MCQALYS of $25-65K
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
54
TABLE 3–2
An Example of Cost Effectiveness and Cost-Utility Analysis
Treatment option
Cost
Life-years
gained
Health-utility index
QALY
Current procedure
$20,000
2 years
0.7
1.4
New procedure
$110,000
8 years
0.4
3.2
Unadjusted MC/MB
of:
current procedure
new procedure
$20K/2
$110K/8
=$10K per LYS
=$1375 per LYS
Quality Adjusted
MC/MB of:
current procedure
new procedure
$20K/1.4
$110K/3.2
=$14.3K per QALYS
=$3475 per QALYS
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
55
Cost-Utility Analysis
• Neumann et al. (2000)
– Effectiveness of prescription drugs
• Mean ratio of $11,000 per quality-adjusted life-year
– Immunization - $2,000 per QALY
– Medical procedures - $140,000 per QALY.
– Surgery - $10,000 per QALY
– Screening at $12,000 per QALY
• Stone et al. (2000)
– Effectiveness of clinical preventive services
• Median cost utility ratio = $14,000 per QALY
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
56
Cost-Utility Analysis
• Digital vs. film mammography
– Digital - superior in its ability to detect cancer for
certain subpopulations
• Far more expensive
– Tosteson et al. (2008)
• Replacement of all-film mammography screening with
all-digital = cost $331,000 per QALY gained
• Targeted-digital mammography screening
– Women 50 and younger - $26,500 per QALY
– Women 50 and younger plus women older than 50 with
dense breasts - $84,500 per QALY
(c) 2010 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part, except for use as permitted in
a license distributed with a certain product or service or otherwise on a password-protected website for classroom use
57