Beyond ADHD: Treating Children with Co
advertisement
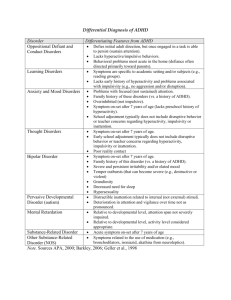
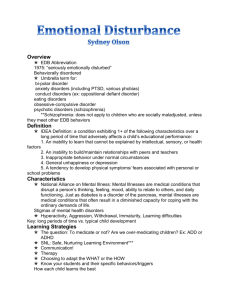
Beyond ADHD: Treating Children with Co-occurring Conditions S. Steve Snow. MD Doug Emch MD Child Psychiatrists- Nashville, TN Professional Affiliations • Private Practice, Child/Adolescent/Adult Psychiatry. Belle Meade Office Park, 4535 Harding RD Nashville TN 37205 (Emch and Snow). • Clinical Professor of Psychiatry, Vanderbilt University (Snow) • Child/Adolescent Psychiatrist, Centerstone Mental Health Centers (Emch) • Child/Adolescent Psychiatrist, Namaste, Inc. (Emch) • Child Adolescent Psychiatrist, Teambuilders Counseling Services, Inc. (Emch) Disclosures • Speaker’s Bureaus: Eli Lilly and Novartis Pharmaceutical Companies (Snow) • Preparation of the presentation received no commercial support • Off-label uses of medications, such as lack of approval for specific diagnosis or certain ages, as frequently used by psychiatrists, will be included. Learning Objectives • Review diagnostic guidelines for Attention Deficit Hyperactivity Disorders (DSM-IV-TR) • Identify common co-occurring conditions with ADHD, and disorders which mimic ADHD • Update pharmacotherapy for ADHD and it’s co-occurring disorders Presentation Outline • • • • • ADHD Mimicry Comorbid Conditions Pharmacotherapy Questions? ADHD Inattention • • • • Hyperactivity • Fidgets • Out of seat • Climbs/runs Impulsivity • Blurts out • Impatient • Interrupts Careless Inattentive Not listening Poor instructions • • • • • Disorganized Avoids Loses things Distracted Forgetful • Loud • On the go • Talkative ADHD Subtypes • Predominantly Inattentive (20-30%) • Predominantly Hyperactive/Impulsive (<15%) • Combined hyperactive-impulsive and inattentive (50-75%) Etiology • Genetic – Heritability about 76% – Complex - Chromosomes 4,5,6,8,11,16,17 • Non-Genetic – Perinatal stress and low birth-weight – Traumatic brain injury – In utero substance exposure – Trauma – Society? Farone, Molecular Genetics of ADHD, Biol Psychiatry 57:1313-1323 (2005) FCC: All Programming To Be Broadcast in ADHDTV by 2007 QuickTime™ and a decompressor are needed to see this picture. …in accordance with the ADHDTV standard, that all shows be no more than six minutes in length, and that they contain jarring and unpredictable camera cuts to shiny props and detailed background sets… QuickTime™ and a decompressor are needed to see this picture. Prevalence • 1-20% of child/adolescent population (5-8%) • Account for 30-50% of child referrals to mental health services • 4-5% of adult population • Males:Females :: 9:1 4:1 2:1 Mimicry • • • • • • • • • • Learning disorders Hypoglycemia/Diabetes Hypo/hyperthyroidism Allergies Hearing/vision problems Toxicity (lead, mercury) Epilepsy Nutrient deficiencies Anemia Sensory integration dysfunction • • • • • • • • • • • Anxiety disorders Bipolar/depression Trauma/PTSD Attachment disorders Sleep disorders Infections Pain Traumatic Brain Injuries Fetal Alcohol Syndrome Substance abuse Family problems Comorbidity • Almost 3/4’s of individuals with ADHD have a psychiatric comorbidity: – – – – – – – – – Conduct Disorder (10-20%) ODD (54-84%) Substance Abuse (40%) Anxiety Disorders (30-40%) Affective Disorders (20-30%) Learning Disorders (@ 33-60%) Tic Disorders (34%) Developmental Disorders (?) Sleep disorders (25-50%) Academic Impairment • Very well documented – Failure to perform academically is the single most common source of referral for children and adolescents • Children with ADHD – Perform poorly on achievement tests and fail grades / courses significantly more often than children without ADHD – Complete 3 fewer years of education than matched controls – More likely not to graduate from high school (35%) • Academic impairment more profound when learning disabilities are present Weiss & Hechtman Hyperactive Children Grown Up 1993 Manuzza & Klein The Economics of Neuroscience, 2001:47-53 Social Function • Social problems begin in childhood, persist into adolescence – – – – – – Fewer friends, more limited social skills Lower self esteem on assessment scores 3X’s as likely to have trouble getting along with peers ½ as likely to have good friends 2Xs as likely to get picked on by peers 3Xs as likely to have problems that limit after school activities Suppl. JAACAP Practice Parameters for Use of Stimulant Medications 2002;41:26S-49S I.M.P.A.C.T. Survey;NYU Child Study Center;2001 Sexual Behaviors • Longitudinal follow-up of cohort of 160 children with ADHD shows: – More unprotected sex & >50% tested for HIV • 0 in the control group – Of 43 children born to study participants, 42 were born to those in the ADHD group • Limiting their academic and occupational attainment • 54% of these had lost custody of the children Barkley. Attention 1996;8-11 Criminality • ADHD has high comorbidity with ODD and CD – Coupled with an impulsive, high risk lifestyle • increases risk for legal problems • Patients with ADHD more likely to be: – Arrested (39% vs. 20%) – Convicted (28% vs. 11%) – Jailed (9% vs. 1%) Biederman et. al. Arch Gen Psychiatry 1996;53,437 Manuzza et. al. Arch Gen Psychiatry 1989;46,1073 Oppositional Defiant Disorder ODD • Pattern of negative/hostile/defiant behavior – Loses temper – Argues with adults – Defies adults’ requests/rules – Deliberately annoys others – Blames others – Touchy/annoyed easily – Angry/resentful – Spiteful/vindictive Conduct Disorder • • • • Aggression to people and animals Destruction of Property Deceitfulness, lying, stealing Serious violation of rules TICs • Transient Tic • Chronic Motor or Vocal Tic • Tourette’s (Motor and Vocal) Sleep Requirements per 24 hours • Infant to 6 months: 16-20 hours • 6mo to 2 yrs: roughly 15 hours • 2 to 6 yrs: 10-12 hours • Grade School (7 to 13 yrs): 9 to 11 hours • High School (14 to 18 yrs): roughly 9 to 10 hours (may vary greatly day by day) Dr. Scott Shannon Please Don’t Label My Child Anxiety Disorders • • • • • • Generalized Separation Obsessive-Compulsive Specific & Social Phobia Panic Stress Disorders/PTSD Affective Disorders • • • • Depression Dysthymia Cyclothymia Bipolar Depression • Prevalence – 2% Children – 4-8% Adolescents – Male:female 1:1 1:2 – 20% cumulative incidence by 18 – 5-10% children/adolescents subsyndromal JAACAP Practice Parameter 46:11, Nov 2007 Depression • 2 weeks of (5): – – – – – – – – – Depressed mood or irritability, or Loss of interest/pleasure Wt change (failure to thrive) Sleep changes Psychomotor agitation/retardation Fatigue Feeling worthless/guilty Poor concentration/indecisiveness Recurrent thoughts of death or suicide Dysthymia • Depressed mood or irritability on most days for most of the day for 1 year • Plus – Changes in appetite or weight – Changes in Sleep – Problems with decision making or concentration – Low self-esteem, energy, hope Juvenile Bipolar Disorder • Adult criteria in DSM; none for youngsters • Severe type of mood disorder; manic-depressive illness • Episodes of mania, major depression, or both, often with psychosis • Mania includes hyperactivity, which can mimic ADHD, but also elation, grandiosity, and flight of ideas; may not sleep for days • Irritability and rapid speech seen with both • Depression often very severe, sometimes mixed with mania; can be suicidal, psychotic, even look catatonic • Key is an up and down course, with children and teens often cycling very rapidly, unlike most adults Developmental Problems and Substance Abuse • Many types of underlying developmental disorder, as well as external factors such as illicit substance use, and complicate or mimic ADHD • Autistic Spectrum Disorder overrides and presumably includes ADHD, under current DSM guidelines, although frequently ADHD sx are marked in these pts and the target of Tx • Cocaine, methamphetamine and other stimulant abuse can mimic ADHD sx, but even marijuana and other CNS-depressant substances can result in dreamy, off-task school performance Developmental Disorders • Co-occurring developmental disorders are the rule with ADHD, but may not be medication targets and require specialized learning approaches: • Mental Retardation, of varying degrees of severity, may be changed to Intellectual Disability or similar term in DSM-V. • Learning Disorder include Reading, Math and Written Language disabilities • Developmental Coordination Disorder may produce problems in sports, predispose to minor injuries, but also be a target of teasing or hazing Developmental Disorders (cont) • Communication Disorders include both expressive and receptive language disabilities, as well as Phonological (Articulation) disorders and Stuttering • Elimination Disorders include enuresis or encopresis and may require both medical and behavioral intervention • Tic Disorder are specified as transient, chronic motor or vocal and Tourette’s Syndrome; most individuals with Tourette’s have parallel ADHD sx and often OCD, as well; stimulants may exacerbate tics and RX may be complex • Haloperidol (Haldol) and pimozide (Orap) are problematic older drugs, age 12 and older for pimoxide, but atypical agents as will be discussed for bipolar disorders are used off-label for severe T.S. Treatment QuickTime™ and a decompressor are needed to see this picture. Medications for ADHD • Stimulants – methylphenidates, amphetamines • Alpha-agonists – Clonidine, Tenex, Intuniv, Kapvay • NE/DA Active Antidepressants – Wellbutrin • Strattera • Provigil/Nuvigil • Tricyclic Antidepressants Duration of Action • 2-5 hours • • • • methylphenidate (MPH) (Ritalin) (1-4 hrs) d-MPH (Focalin) (1-4 hrs) d-amphetamine (Dexedrine) (1-6 hrs) Amphetamine-dextroamphetamine (Adderall) (4-6hrs) • 5-8 hours • • • • methylphenidate SR (Ritalin SR) (3-8 hrs) methylphenidate ER (Metadate ER, Methylin ER) (3-8 hrs) d-amphetamine (Dexedrine Spansules) (6-8 hrs) extended release MPH (Ritalin LA & Metadate CD) (6-8 hrs) • 10-12 hours • • • • • methylphenidate (Concerta) (10-12 hrs) dexmethylphenidate (Focalin XR) (10-12hrs) Methylphenidate transdermal (Daytrana) (9-12) amphetamine-dextroamphetamine (Adderall XR) (10-12 hrs) lisdexamfetamine (Vyvanse)- (12-14hrs) Stimulant Side Effects • • • • • • • Delay of sleep onset Reduced appetite Weight loss Tics Stomach ache Headache Jitteriness But not necessarily • Staring • Daydreaming • Irritability • Anxiety • Nail biting Suppl. JAACAP Practice Parameters for Use of Stimulant Medications 2002;41,#2:29S Diet • Issues with sugars and dyes • Citric Acid and Ascorbic Acid – Citrus fruits, juices – Coke, Diet Coke, Dr. Pepper, A&W Root Beer • Not the clear, yellow, or red drinks – Cereals, MVI – Anything in foil wrappers • High fat diets Medications for ADHD • Stimulants – methylphenidates, amphetamines • Alpha-agonists – Clonidine, Tenex, Intuniv, Kapvay • NE/DA Active Antidepressants – Wellbutrin • Strattera • Provigil/Nuvigil • Tricyclic Antidepressants Antidepresants • SSRIs – Fluxoetine (Prozac), Sertraline (Zoloft), Citalopram (Celexa), Escitalopram (Lexapro), Paroxetine (Paxil), Fluvoxamine (Luvox) • SNRIs – Venlafaxine (Effexor), Desvenlafaxine (Pristiq), Duloxetine (Cymbalta) • NE/DA – Buproprion (Wellbutrin) Antidepressants (cont) • Tricyclics – Imipramine (Tofranil), Amitriptyline (Elavil), Clomipramine (Anafranil) • Other – Trazodone, Remeron SSRI Side Effects • Common – sleep changes – restlessness – headaches – akathisia – appetite changes – sexual dysfunction • 3-8% youths – impulsivity – agitation – irritability – silliness – “behavioral activation” Black Box Warning: Suicidality JAACAP Practice Parameter 46:11, Nov 2007 Anxiolytics • SSRIs – Prozac, Zoloft, Celexa • • • • Buspar Neurontin Strattera? Benzodiazepines – Valium, Klonopin, Ativan Pharmacotherapy of Bipolar Disorder • Lithium carbonate, typically from 150 mg to 450mg, one to two tabs or caps, up to BID often in controlled-release form • FDA approval ages 12-17; many side effects, including tremor, thirst and somnolence; lab needed to monitor Li levels, electrolytes, renal and thyroid studies • Calms mania and helps prevent mood excursions, but not very effective for depression • Less likely now to be the first agent prescribed Bipolar Treatment: Anticonvulsants • Anticonvulsant “mood stabilizers” • Commonly prescribed, approvals for pediatric epilepsy, but not for mood problems • Valproic Acid (Depakote) has adult bipolar indication; dose range 125mg BID to as much as 750mg BID, or more; may cause drowsiness or ataxia; lab monitoring for serious liver, pancreatic or heme A.E.’s • Lamotrigine (Lamictal) also has adult bipolar indication; dose range 25mg BID to 150mg BID, or more; usually well-tolerated and no blood monitoring, but rare toxic rashes, and very slow acclimation Anticonvulsants (cont) • Oxcarbamazepine (Trileptal) does not have an indication for mood disorders, adult or children, but has had considerable clinical use, and largely replaced carbamazepine (Tegetol); usually tolerated except for sedation and hyponatremia, though not usually a problem; dosed 150mg BID up to 600mg BID or more • Topiramate (Topamax) also used off label in doses of 50-100mg BID, up to 200mg BID or more, but may cause some cognitive difficulties, such as anomia, and predispose to renal stone formation • Gabapentine (Neurontin) used off label in doses of 100mg BID or TID, to as much as 600mg TID or more; some initial fatigue, like other agents, but generally well-tolerated and does not interact much with other drugs Bipolar Treatment: Atypicals • Atypical neuroleptics, such as Risperidone, Aripiprazole, and Olanzepine have mostly replaced older agents, such as Haloperidol and Thioridazine, so-called “typical neuroleptics” • Risperidone (Risperdal) in doses from 0.25mg BID, all the way to 4mg BID, or more, treat mania and stabilize bipolar episodes; approved in children and adolescents ages 10 and up for mania; can cause significant weight gain, sedation, prolactin stimulation and other adverse effects • Aripiprazole (Abilify) approved ages 10-17 and used in doses of 2mg daily up to a maximum of 30mg per day, often in divided doses; generally not as much weight increase, but may cause restlessness and dystonias; does not elevate prolactin Atypical Antipsychotics (cont) • Olanzepine (Zyprexa) is a potent anti-psychotic, with concerns of weight gain and subsequent metabolic problems, but does have an approval for bipolar 1 disorder, ages 13-17; dose ranges from 2.5 to 30mg, or more • Quiatepine (Seroquel) is not approved in children or adolescents, but used for insomnia of bipolar disorders, and for psychosis and mood stability in higher doses, range from 25 to 800mg or more, off label. Sedation and wt gain as S.E.’s • Ziprasidone (Geodon), also non-approved in kids, but sometimes used because of wt. gain from other agents, or sedation from other agents; more concern in children of QT prolongation on EKG; more EPS and akathisia; does not raise prolactin levels Parent Medication Guide • Newly revised guide for Depression in children and adolescents • Comprehensive guide to ADHD Rx; nice discussion of conditions that accompany and/or “show the same type of sx” • Joint project of American Psychiatric Association and American Academy of Child and Adolescent Psychiatry • Available at ParentsMedGuide.org • Slides available at www.emchpsychiatry.com ? Dopamine • Enhances signal • Improves attention – – – – – Focus Vigilance Acquisition On-task behavior On-task cognition Nigrostriatal Pathway Mesolimbic Pathway Substantia nigra Mesocortical Pathway Ventral tegmental area Solanto. Stimulant Drugs and ADHD. Oxford; 2001. Norepinephrine • • • • Dampens noise Decreases shifting Executive operations Increases inhibition –Behavioral –Cognitive –Motoric Frontal Limbic Locus ceruleus Solanto. Stimulant Drugs and ADHD. Oxford; 2001.