Popular Links
advertisement

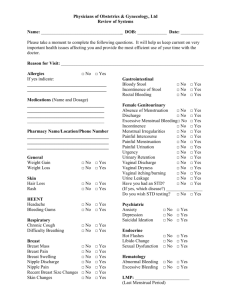
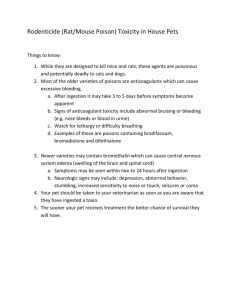
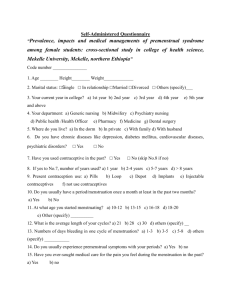
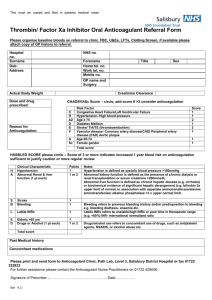
Disorders of Menstruation Pathophysiology, Evaluation and Management Jennifer Mersereau, MD Division of Reproductive Endocrinology & Infertility Department of Obstetrics & Gynecology University of North Carolina March, 2009 Objectives What defines abnormal menstruation? Burden of disease Differential diagnosis of abnormal menstruation patterns Classification of abnormal menstruation Evaluation Treatment Physiology of Menstruation •Exact hormone levels not crucial •Exact cycle day not crucial •General sequence crucial Ovulatory Cycles Orderly proliferation Synchronous, stable endometrial development Lysosomal digestion, vasoconstriction & ischemia desquamation, coagulation, hemostasis Progesterone Estrogen 2 4 6 8 10 12 14 16 18 20 22 24 26 28 Menses NORMAL MENSTRUAL BLEEDING IS SELF-LIMITED Menstrual Cycle What is normal? Menses Duration Volume Interval 4-6 days Approx 30 ml 24-35 days Menometrorrhagia <2 >7 days > 80 ml Menorrhagia Polymenorrhea Oligomenorrhea < 24 > 35 days Metrorrhagia Menstrual Cycle Characteristics Age Variations Highest variation in early adolescent and perimenopausal years Adolescent: long intervals for 5-7 years after menarche Reproductive years: • Majority of cycles 25-28 days • Cycle length can change around age 40-42 until menopause Health, 1986; Belsey, 1997; Volman, 1977; Treolar, 1967; O’Connor, 2001; Taffe, 2002. Abnormal Menstruation: Burden of Disease Most common reason for GYN visits 600,000 hysterectomies each year • ¼ US women will have a hysterectomy by age 60 • 2nd most frequent surgery among reproductive-aged women • Annual cost of $5 billion Most common conditions for hysterectomy: • Fibroids, endometriosis, prolapse • If < 30 years old, menstrual disturbances and dysplasia Surveillance for Reproductive Health, Hysterectomy Surveillance—United States, 1994-1999. Evaluation of Abnormal Menstruation Consider differential diagnosis Target history to narrow differential Exam Labs Imaging Evaluation of Abnormal Menstruation Differential Diagnosis Pregnancy complication! • • • • Threatened or incomplete abortion Ectopic pregnancy Gestational trophoblastic disease Retained products of conception Benign anatomical lesion • Cervical or endometrial polyp • Leiomyoma • Adenomyosis Malignancy • Cervical or uterine cancer (esp HIV + women) Evaluation of Abnormal Menstruation Differential Diagnosis Trauma/foreign body • Children Inflammatory conditions • Endometritis Systemic illness • • • • Thyroid dysfunction Hyperprolactinemia Renal failure Hepatic dysfunction Bleeding disorder • Thrombocytopenia • Platelet function abnormalities • von Willebrand’s disease Medications • Steroidal • Psychiatric Or….. Dysfunctional Uterine Bleeding DUB is a diagnosis of exclusion! DUB is: • Abnormal bleeding pattern, AND • NO ATTRIBUTABLE UNDERLYING ILLNESS OR PATHOLOGY Causes: • Anovulation (90%) Polycystic ovarian syndrome Teenagers or peri-menopausal women • Rarely short follicular or luteal phase Evaluation of Abnormal Menstruation Step 1: History Detailed menstrual history • Inter-menstrual intervals Consistent, normal (q 24-35 days) Variable • Character, volume • Duration Normal (3-7 days) Prolonged • Initial onset of symptoms Evaluation of Abnormal Menstruation Step 1: History Other associated symptoms • • • • • Dysmenorrhea Post-coital bleeding Galactorrhea Hirsutism Fatigue, weight gain, constipation (thyroid) Temporal associations w/ other events • Weight changes • Medication changes Medical history & medications GOAL OF HISTORY: • Does she ovulate? If not, DUB LIKELY! • What labs do you need to confirm you initial diagnosis? Evaluation of Abnormal Menstruation Ovulation - does she or doesn’t she? • • • • • Menstrual history Basal body temperature (BBT) monitoring (biphasic) Ovulation predictor kits Timed serum progesterone (> 3 ng/ml) Ultrasound Implications: if ovulatory… • Search for an anatomical/pathological cause Evaluation of Abnormal Menstruation Step 2: Exam Weight Thyroid exam Signs of other illnesses Signs of hyperandrogenism • Hirsutism • Acne Endocervical Polyps Squamous Cell Carcinoma of Cervix Pelvic exam • Cervical and vaginal lesions • Size, shape of uterus Evaluation of Abnormal Menstruation Step 3: Laboratory Tests All patients: screen for • Pregnancy (history or urine hcg) • Thyroid disorder (TSH) • Anemia, thrombocytopenia (CBC) Select patients: • • • • Hyperprolactinemia (PRL) Bleeding disorders (coagulation panel, vWF) Chemistry (AST, ALT, Creatinine) Endometrial biopsy???? Evaluation of Abnormal Menstruation Endometrial Biopsy Risk of endometrial carcinoma: • Age 30-34: • Age 35-39: • Age 40-49: 2.3/10,000 6.1/10,000 36.2/10,000 Duration of time exposed to unopposed estrogen is more important than age Possible results: proliferative, secretory, hyperplasia, atypia, carcinoma, acute or chronic endometritis Ash, J Reprod Med, 1996.; ACOG Practice Bulletin 14, 2000. Endometrial Biopsy Chronic endometritis Adenocarcinoma Endometrial Hyperplasia Evaluation of Abnormal Menstruation Step 4: Imaging Who needs imaging? Regular cycles volume duration Regular cycles intermenstrual bleeding Abnormal bleeding, evidence of ovulation RULE OUT ANATOMIC LESION Failed medical management Evaluation of Abnormal Menstruation Step 4: Imaging Ultrasound can help diagnosis: • • • • Fibroids Polyps Adenomyosis Endometrial stripe < 5 mm, denuded, atrophic 5-12 mm, normal > 12 mm, thick, biopsy! Hydrosonogram: increases sensitivity to detect endometrial lesions, 70% 90% Hysteroscopy Becker, 2002. Uterine Imaging Ultrasound Normal endometrium Late proliferative or luteal phase Thin endometrium Early proliferative phase or atrophy Uterine Imaging Routine Ultrasound Saline Sonogram Submucous myoma Endometrial polyp Uterine Imaging Hysteroscopy Hyperplasia Polyps Atrophy Myoma Adenocarcinoma Treatment of Abnormal Menstruation What is the diagnosis? DUB Restore growth, development and shedding of a stable endometrium Prevent development of hyperplasia or neoplasia Bleeding from Specific Cause Cycle Physiology Progesterone Estrogen Estrogen 2 4 6 8 10 12 14 16 18 20 22 24 26 28 Menses DUB/Anovulation Ovulatory Cycle Treatment: DUB Option 1: Cyclic Progestins Rx Progestin Rx Progestin Endogenous estrogen 1 5 9 13 17 21 25 1 5 9 13 17 21 25 Calendar Day Progestins: 1. Medroxyprogesterone (MPA) 10mg qd 2. Norethindrone acetate 5 mg qd Treatment: DUB Option 2: Oral Contraceptives Rx Cyclic OCP Rx Cyclic OCP Progestin Progestin Estrogen Estrogen Endogenous estrogen 1 5 9 13 17 21 25 1 5 Pill Cycle Day 9 13 17 21 25 Treatment of Anovulation with Acute, Heavy Bleeding Hemodynamically stable?? • IVF, CBC, transfusion • D&C Strongly consider biopsy Ultrasound Treatment – High dose OCP taper Treatment of Anovulation Maintenance Therapy • Goal: Restore regular menstrual bleeding patterns • Prevent endometrial cancer!! • Failed management = further workup Treatment: Anovulatory Bleeding Preventing Endometrial Hyperplasia & Neoplasia Histology Cytologic Atypia Architectural Pattern Risk of neoplasia Simple hyperplasia -- Regular 1% Complex hyperplasia -- Irregular, crowded 3% Simple + atypia + Regular 8% Complex + atypia + Irregular, crowded 29% Kurman et al, Cancer, 1985 Treatment: Anovulation Preventing Endometrial Neoplasia ATYPIA Present Yes Fertility desired? Megace 40-80mg x 3-6 months Re-biopsy Absent No Hysterectomy Cyclic progestins or OCPS Rebiopsy if abnormal bleeding occurs Treatment of Abnormal Menstruation What is the diagnosis? DUB Bleeding from Specific Cause Treat underlying cause Decrease volume and duration of menses Treatment Complications of Pregnancy Ectopic pregnancy • Salpingostomy • Salpingectomy • Methotrexate Threatened abortion • Observation Incomplete/inevitable abortion • Curettage Empty Sac Ectopic Treatment Chronic endometritis Indirect cause of bleeding Twice as common in HIV+ patients Doxycycline 100mg bid x 10 days Kerr-Layton et al, Infect Dis Obstet Gynecol, 1998 Treatment Leiomyomas Medical treatment • OCPs: decrease volume/duration of menses • NSAIDS • GnRH agonists Surgical treatment • Myomectomy • Hysterectomy Treatment Small Submucous Myomas, Polyps 1 2 Hysteroscopic Resection 3 Treatment Prolapsing, Large Myomas Abdominal or Laparscopic Myomectomy Vaginal Myomectomy Treatment Multiple Myomas Completed Childbearing Abdominal Hysterectomy Treatment: Ovulatory Patient with Unexplained Menorrhagia Medical Options • NSAIDS: 20-40% decrease • OCPs: 40% decrease • Levonorgestrel IUD: 75-95% decrease Excellent option with chronic illnesses Women highly satisfied • GnRH agonists Surgical Options • Endometrial ablation • Hysterectomy Hall, Br J Obstet Gynecol, 1987; Fraser, Aust NZ J Obstet Gynecol, 1995; Cochrane Database Syst Rev, 2002. Absence of Menstruation Primary Amenorrhea Outflow obstruction, Mullerian abnormalities Androgen insensitivity syndrome – 46 XY Ovarian failure • Turners syndrome, 45 XO • Autoimmune • Cancer treatments Other causes Secondary Amenorrhea Asherman’s syndrome Premature ovarian failure Pituitary lesion • Most common = prolactinoma • Sheehan’s syndrome Hypothalamic hypogonadism Other causes Abnormal Puberty Precocious Puberty <8 years old GnRH-dependent • Idiopathic – most common • CNS abnormality GnRH-independent • Ovarian cyst/tumor • McCune Albright syndrome Treatment: • Surgery when appropriate • GnRH agonist Delayed Puberty See primary amenorrhea Conclusions Abnormal menstruation is extremely common Most common cause of a sudden change in bleeding patterns is a complication of pregnancy! Careful menstrual history Use labs and imaging to support your clinical suspicions Anovulatory bleeding: goal is to restore normal menstrual patterns Bleeding from other causes: correct underlying pathology and decrease volume/duration of menses Questions? Examples of Effects of Exogenous Progestin in Ovulatory Cycles Ovulation Provera C Provera B Provera A Endogenous Progesterone Follicular Phase 14 Luteal Phase 28 Treatment: Anovulatory Bleeding Preventing Endometrial Hyperplasia & Neoplasia Simple Hyperplasia Complex Hyperplasia Complex Atypical Hyperplasia Menstrual Cycle Definitions of Abnormalities Irregular intervals • Oligomenorrhea, > 35 days • Polymenorrhea, < 24 days Excess amount and/or duration • Menorrhagia Irregular interval • Metrorrhagia Irregular interval and amount/duration • Menometrorrhagia Uterine Imaging Ultrasound Submucous myoma Intramural myoma Adenomyosis ADD: (4/7) • Info about PCOS vs. hypo-hypo. • Look up DUB (is it almost always PCOS??) • More about HIV? Treatment: Acute bleeding High dose OCP ‘Taper’ Progestin Rx OCP (monophasic) bid X 7d, qd X 7-14d Estrogen Endogenous Estrogen Menses Treatment: Atrophic Endometrium Sequential Estrogen and Progestin Rx Progestin Rx Estrogen (CEE 1.25-2.5 mg/d or micronized estradiol 2.0 mg/d, q4h prn; CEE 25 mg i.v. q4h prn) Endogenous Estrogen Menses