Reproductive System
advertisement
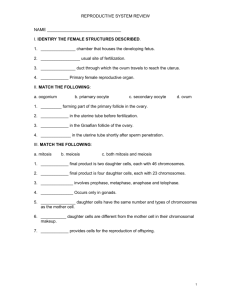
Reproductive System Human Anatomy Chapter 24 • The reproductive system becomes active after puberty. During puberty the reproductive organs mature to create a fertile individual capable of reproducing. The primary sex organs produce the sex cells (egg/sperm) and sex hormones. The accessory sex organs are all the components involved in maintaining the sex cell and assisting in the process of fertilization. • • • I. The male reproductive system: This system is simpler than the female reproductive system. A. Scrotum: a sac located outside of the abdominal cavity, made up of a thin layer of smooth and skeletal muscle and skin. It is divided into left and right by a septum to form different compartments for the testicles. The scrotum keeps the testicles outside the body so they can be 3 degrees cooler than normal core temperature. The muscles of the scrotum contract to bring the testicles closer to the body in cooler conditions. In warm conditions they relax to allow the skin to stretch and maximize cooling. • • B. Testes: Oval shape organs made up of thousands of seminiferous tubules where the sperm is produced. It responds to follicle stimulating hormone that signals sperm production. When the sperm is in its last stages of maturation it moves to the epididymus. 1. Gross anatomy: about 1 x 4 inches, complete surrounded by a fibrous capsule and partially enclosed by a serous membrane that develop when the testes traveled outside the body into the scrotum. The fibrous capsule divides the testicles into wedge-like compartments called lobules that are filled with seminiferous tubules. They are innervated by an abundant about of visceral sensory nerves that make them very sensitive to pain. The high sensitivity serves for protection and in sexual arousal. • 2. Seminiferous tubules and spermatogenesis: The seminiferous tubules consist of a thick stratified epithelium surrounding a lumen. The epithelium has spermatogenic cells that mature into sperm. At puberty the seminiferous tubules begin to produce about 400 million sperm. the spermatogenic cells are protect by a blood-testis barrier that keep the cells from activating the immune system. • Spermatogenesis: these are the stages involved in sperm formation. • Stage 1: formation of spermatocytes: spermatogonia divide by mitosis to produce two daughter cells, one remains in the germ line (to continue regeneration of more spermatogonia) and the other one goes on to become sperm. • Stage 2: Meiosis: this is a reduction division that takes a cell through two rounds of division. At the end four genetically distinctive cells (spermatids) are created which will each mature into a sperm. • Stage 3: Spermiogenesis: spermatids mature into sperm, the cell develops a long flagella, a mid piece with high mitochondria count, and a “head” filled with DNA= the nucleus. At the tip of the head lies a sac filled with digestive enzymes called the acromosome (see page 676). • Other cells in the testicles perform jobs like assisting the cells to mature and exit the scrotum (referred to as nurse cells), produce male androgen (like testosterone), and muscular cells that cause tiny contractions to push the sperm out of the testes. When sperm leaves the seminiferous tubules it travels down the efferent tubules towards the epididymis. • C. Reproductive duct system is males: This section discusses the tubules through which sperm travel to exit the body. • 1. Epididymis: organ that arches over the posterior lateral side of the testis. If you uncoil the epididymis is can be as long as 6meters or 20 feet! During the twenty days the sperm spend here they complete maturation and gain the ability to swim and fertilize. During ejaculation smooth muscle contracts to send mature sperm to the ductus deferns. • 2. Ductus deferens: also known as the vas deference, it runs superior to the testicles, enters the abdominopelvic cavity, runs posterior to the bladder, passes by the seminal vesicle, form the ampulla and ejaculatory duct, and finally leads into the prostatic urethra. • 3. Spermatic cords: a tube of fascia holding blood vessels, nerves, and the ductus deference. See page 672 figure 24.2. • 4. Urethra: As discussed in the previous chapter the urethra and men carries both sperm and urine. During ejaculation the sphincter muscles close off the bladder so urine is not released into the semen. The urethra is divided into the prostatic urethra (section passing through prostrate gland), the membranous urethra (urogenital diaphragm) and the spongy urethra (penile). Urethral glands along the spongy urethra secrete a lubricating solution before ejaculation. • D. Accessory glands: These glands produce substances that increases the chances of sperm survival once it is outside the body. These secretions in addition to sperm form semen. • 1. Seminal vesicles: paired glands located posterior to the bladder. During ejaculation smooth muscle contract to help secrete a fluid that contains fructose (sugar), nutrients, prostagladins to stimulate the urethra to contract, substances that suppress the immune system against sperm in females, enzymes the enhance sperm mobility, and enzymes that thicken the ejaculate. • 2. Prostate gland: the size of a chestnut, also has smooth muscle that contracts to assist in the release of prostatic secretion. This is a milky white fluid that has substances to enhance sperm mobility and thicken ejaculate. It is susceptible to tumors and sexually transmitted diseases (STDs). • 3. Bulbourethral glands: secrete a mucus substances that lubricates and neutralizes the acid from urine in the male urethra. E. Penis: Designed to deliver semen into the female reproductive tract. It originates at the root, expends through the body, and ends at the glans penis. Skin around the glans penis is called prepuce (circumcision has contradicting arguments that seem to weigh equally). The penis contains erectile bodies: corpora spongiosum, corpora cavernosa, and others consisting of smooth muscle and connective tissue. It is a spongy network surrounded by a high amount of blood vessels that dilate during arousal and engorge the spongy tissues with blood. The veins that normally drain the penis are pressured shut by the expanding spongy tissue. The parasymphatetic branch causes the penis to become erect by stimulating vasodilation. The symphatetic branch cause ejaculation by stimulating contraction of smooth muscle along the reproductive tract. • II. The female reproductive system: These organs produce the ova (eggs), sex hormones, and provide an environment for internal fertilization and development of the fetus. They undergo changes according to the menstrual cycle. Mammary glands are considered part of this system because they nourish the infant. • A. The ovaries: the size of an almond, this paired organ is suspended by mesenteries and ligaments. It is surrounded by a fibrous capsule and can be divided into a cortex and medulla. The cortex houses the developing ova and the medulla holds vascular tissue. The ovary is the site of oogenesis and female sex hormone production. It responds to follicle-stimulating hormone that signals the maturation of an ovum. Typically only one egg is released from an ovary every month, the ovaries alternate in releasing the egg. Every time an egg is released the ovaries become scarred. Hormones that affect the menstrual cycle and female sex organs are also released by the ovaries; estrogen and progesterone. • 1. Ovarian cycle: this concerns the changes in the ovary during the menstrual cycle. Females are born with all the potential ova they can produce in a life time. These are called the primordial follicles which consist of a single immature oocyte and a single layer of follicular cells. These cells respond to FSH and being the maturation of an oocyte. • Follicular phase: during the first two weeks of the menstrual cycle one follicle matures up until the stage when it is able to release an oocyte. Other primordial follicles may get activated but die out along the way. The primordial follicle becomes the primary follicle and continues to develop until it becomes the vesicular follicle. At this point the oocyte is surrounded by follicle cells that the form a fluid filled cavity. • • Ovulation (midpoint) phase: at about the mid cycle LH is release to signal the follicle to rupture and release the oocyte from the ovary. The ovum is surrounded by a group of cells that continue to nourish it, they are called the corona radiata. When the egg cell is released it enters the peritoneal cavity but is swept into the fallopian/uterine tubes by fimbriae. Luteal phase: after ovulation and during the last two weeks of the cycle the follicle that held the oocyte becomes the corpus luteum, it is now considered an endocrine gland that releases progesterone. If no implantation occurs it becomes the corpus albicans (now scar tissue). • 2. Oogenesis: while in men spermatogenesis happens in about a month, in females oogenesis takes several years. During fetal development oocytes undergo meiosis I but do not completel it; at this point they are called primary oocytes. At ovulation the primary oocyte completes meiosis I and begins meiosis II which is completed only if fertilization occurs. At the completion of meiosis II the oocyte is called an ovum. • B. Uterine tubes: also called fallopian tubes, they take the oocyte and provide a site for fertilization. The tube is lined with ciliated epithelium that gently guides the oocyte towards the uterus. There are also peristaltic waves caused by smooth muscle contraction to aide the movement of the oocyte. There are also non-ciliated cells the nourish the oocyte or embryo on its way to the uterus. sometimes a fertilized egg can implant in a uterine tube and cause a life threatening ectopic pregnancy. Uterine Tube Histology • C. The uterus: a thick muscular pouch about the size of a pear that lies in the pelvic cavity superior to the bladder. The function of the uterus is to receive an embryo and provide an environment for its development. During pregnancy it stretches to accommodate the growth of the fetus. When there is no pregnancy the cavity within the uterus is small. The opening of the uterus is at the cervix, during child birth it dilates to allow the child to pass by. The cervix tissue may become infected by a virus called HPV human papilloma virus. It can cause abnormal tissue growth including cervical caner. The purpose of pap-smears is to check the cervical tissue for abnormal growth. • 1. Supports of the uterus: The uterus, cervix, and vagina are supported by ligaments and mesenteries. Most uterine support is provided by muscles of the pelvic floor. Sometimes these muscles are torn during child birth and the unsupported uterus results in a prolapsed uterus. In this condition the tip of the cervix protrudes through the opening of the external vagina. • 2. Uterine wall: composed of three layers: perimetrium (outer= serous membrane), myometrium (middle= layers of smooth muscle), and endometrium (inner= simple columnar epithelium). The thick layer called stratum functionalis (above myometrium) undergoes most of the changes during the uterine cycle. • 3. Uterine cycle: also called the menstrual cycle, it relates to changes occurring in the endometrium of the uterus that are induced by female sex hormones. • Menstrual phase: (days 1-5) during this phase the endometrium is shed • Proliferative phase: (days 6-14) during this phase the endometrium builds a new stratum functionalis as it responds to rising estrogen levels. As the layer thickens glands release a clear sticky mucus secretion that assist the sperm in finding the egg. • Secretory phase: (days 15-28) during this point the stratum functionalis is highly vascularized and there is secretion of glycoproteins to support a developing embryo in case fertilization occur. These changes are a response to progesterone released by the corpus luteum in the ovary. If there is no fertilization the progesterone levels drop signaling changes that cause death of the stratum functionalis. The arteries constrict cutting out blood supply and suddenly open again but the weak capillaries fragment and the menstrual phase begins again. D. The vagina: also known as the birth canal. It is the opening that leads into the cervix and is located anterior to the anus but posterior to the clitoris and urethral opening. The vagina is also the site where sperm is deposited. This canal is very flexible and it composed of three layers: adventitia, muscularis, and mucosa. It also has ruggae to stimulate the penis during intercourse and stretch out during childbirth. The mucosa is made up of stratified squamous epithelium. It secretes glycogen to maintain healthy beneficial bacteria that produce lactic acid. This creates an acidic environment that is not beneficial to other bacteria or sperm. • E. External genitalia: also called the vulva and often incorrectly referred to as the vagina. It includes the mons pubis (fatty rounded pad over the pubic symphisis), the labia majora (thick skin fold analogous to the scrotum), the clitoris (erectile tissue analogous to the penis), and vestibule associated structures( the vaginal and urethral orifice and vestibule glands). The vestibule are protected by the mucus membrane sheathes called the labia minora. • F. Mammary glands: modified sweat glands that are active in pregnant females to produce milk for the infant. These first appear as rudimentary structures in both men and women. When females reach puberty the ducts grow but the glands do no fully develop; the mas of the breast is mostly adipose. During pregnancy glandular alveoli form and produce milk shortly after childbirth. The breast include the nipple and the areola (ring around nipple). The glands consist of lobes that drain into the nipple by lactiferous ducts and lactiferous sinuses where milk accumulates during breastfeeling. Lymoph vessels drain into the parasternal and axillary lymphonodes. • • III. Pregnancy and childbirth: This section briefly describes the evens that occur in the woman’s body during fertilization, pregnancy, and childbirth. A. Pregnancy: occurs once an egg is successfully fertilized and successfully implants. • 1. Events leading to fertilization: Sperm swims from the vagina through the cervix, through the uterine wall until it reaches the oocyte in the uterine tubes. When burrows into the zona pellucida of the oocyte enzymes digest it way to allow the sperm to reach the egg. The plasma membranes fuse and sperm nucleus enters the oocyte’s cytoplasm. This initiates the cortical reaction in which the egg destroys other sperm receptors so no other sperm binds and fertilizes the egg. When the male and female chromosomes come together fertilization has been completed and the zygote will begin to divide. Once it is large enough and has formed a blastocyst it enters the uterus to implant. •2. Implantation: Six days after fertilization the blastocyst implants as it burrows into the endometrium. At this point some cells will become the developing embryo and some the placenta. As the trophoblast burrow into the endometrium it causes bleeding (about 10-12 days after fertilization). • 3. Formation of the placenta: The embryonic tissues from finger like projection called chorionic villi that come in contact with the area of the bleeding endometrium (lacunae) and the embryo connect to the chorionic villi via the body stalk which will become the future umbilical cord. By the end of the first month the embryo’s blood is in close contact with the mother’s blood and exchange of nutrients and waste is happening at the chorionic villi. At the start of the 4th month the endometrium and the chorionic villi make a thick disc called the placenta. This is the site where nutrient and waste exchange occur. After childbirth the placenta detaches from the uterus. • 4. The placenta: produces hormones such as progesterone and human chorionic gandotropin HCG that keep the placenta attached. It prevents bacteria from the mother to transfer to the child, allows nutrients and antibodies to flow from mother to child, and the transfer of waste from child to mother. Viruses and drugs do cross the placenta. As soon as one week after fertilization HCG can be detected in blood test and two to three weeks in urine. • B. Childbirth: also known as parturition, labor is the events prior to childbirth. When the fetus grows so much that the placenta cannot meet its nutritional needs stress hormones are release to signal the beginning of labor. Oxytocin and prostaglandins cause the uterus to contract. Stages of labor: • Dilation stage: begins when the uterus first contracts and ends when cervix dilates (10cms). Cervical dilation can take 6-12 hours. • Expulsion stage: from the time the cervix is fully dilated until the child leaves the mother’s womb. There are strong placental contractions, this process can take up to 2 hours. • Placental stage: uterine contractions discharge the placenta. The umbilical cord is checked for the presence of two arteries and one vein (one indicates a heart disorder). • IV. Disorder of the reproductive system: Study on your own the section on reproductive system cancers in males and females STD STATS • Chlamydia- (bacteria) 3 million new cases per year- 75% have no symptoms. Painful frequent urination, discharge, painful sex, sore throat, fever, nausea • Gonorrhea- (bacteria) 700,000 cases/year 50% have no symptoms or the same simptoms as Chlamydia • Herpes (virus) 1 million new cases/year, 45 million already have it. 1 in 4 pregnant women have herpes HSV-1 (oral sores) HSV-2 genital • HIV- 7,000 women give birth per year. 20% of infected babies develop AIDS and die by age 4 • HPV- 75% of the reproductive population is infected ( 3 in 4 people) • Syphilis- 32,000 new cases/year. A pailess sore is followed by a rash, followed by rough “copper penny” spots on the palm and bottom of feet • Trichomoniasis- a bacteria that affects 5 million women/year. Foul smell, green discharge, itching,redness