MALE REPRODUCTIVE SYSTEM
advertisement

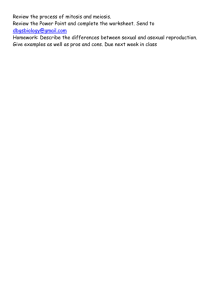
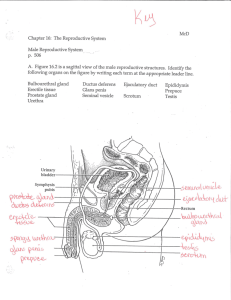
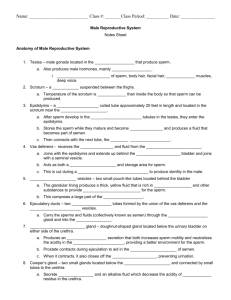
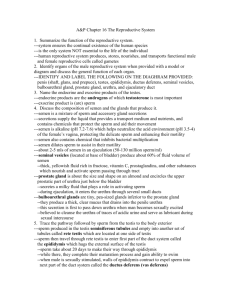
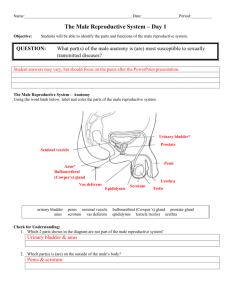
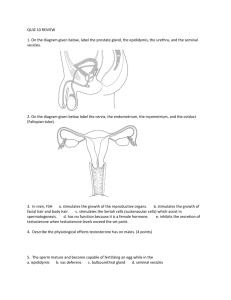
MALE REPRODUCTIVE SYSTEM Anatomy of the Male Reproductive System • The primary sex organs are the testes. • The accessory organs include a complex set of ducts and tubules leading from the testes to the penis. • The penis is the organ of copulation. Anatomy of the Male Reproductive System Figure 28.11 Scrotum • The scrotum is a skin-covered sac that provides the testes with a cooler environment than body temperature. • Sperm develop successfully at approximately 3 Celsius below normal body temperature. • The scrotum is homologous to the labia majora in the female. • A raphe separates the two scrotal sacs. • The dartos muscle is a layer of smooth muscle that is part of the wall of the scrotum. Scrotum Figure 28.12 Spermatic Cord The spermatic cord originates at the inguinal canal. It consists of the following: • Testicular artery—branch of the abdominal aorta • Pampiniform plexus—a network of veins surrounding the testicular artery • Cremaster muscle and fascia—formed from muscle fiber extensions of the internal oblique muscle • Autonomic nerves— travel with plexus and connect to the testes Spermatic Cord Figure 28.12 Testes • The function of the testes is twofold: 1.production of sperm 2.production and secretion of androgens (male sex hormones), the most common being testosterone • • Each testis is covered anteriorly and laterally by a serous membrane called the tunica vaginalis The tunica vaginalis has an outer parietal layer and an inner visceral layer Testes Figure 28.13 Testes • Located just deep to the visceral layer and in contact with the testis is a thick, whitish fibrous capsule covering the testis called the tunica albuginea. • The tunica albuginea projects into the interior of the testis as the mediastinum testis through which blood vessels, lymphatic vessels, and some nerves enter and leave the testis. Testes • The tunica albuginea projects internally into the testes to form septa. • The septa subdivide to form about 250 lobules. • Each lobule contains four convoluted seminiferous tubules. Seminiferous Tubules Seminiferous tubules contain two types of cells: 1. Sustentacular cells—nondividing support cells that assist with sperm development; connected to each other by tight junctions and form the blood-testis barrier 2. A population of dividing germ cells that continuously produce sperm beginning at puberty Interstitial Space • Spaces external to and in between seminiferous tubules • Interstitial cells reside in these space and produce hormones called androgens Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Interstitial cells Seminiferous tubule Tubule lumen Sustentacular cells Sperm cells Spermatids Spermatogonia Figure 28.13 LM 250x (b) Seminiferous tubule, cross section b: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Spermatogenesis and Spermiogenesis Figure 28.14 Spermatogenesis and Spermiogenesis Figure 28.14 Stages of Spermatogenesis Ducts in the Male Reproductive System Beginning at the testis and extending through the penis, the ducts are: • Rete testis • Efferent ductules • Epididymis • Ductus deferens • Ejaculatory duct • Urethra Ducts in the Male Reproductive System Figure 28.15 Rete Testis • Receive sperm from seminiferous tubules Figure 28.13 Efferent Ductules • Connect rete testis to epididymis Figure 28.13 Epididymis • • • Situated on the posterosuperior surface of the testes, the epididymis has three regions: - head - body - tail Internally, the epididymis contains a long convoluted duct of the epididymis The epididymis stores sperm and serves in the maturation process of sperm Epididymis Figure 28.13 Ductus Deferens • Sperm leaving the epididymis enter the ductus deferens (vas deferens). • This tube travels within the spermatic cord and enters the pelvic cavity through the inguinal canal. • As the ductus deferens approaches the prostate gland, it enlarges to form the ampulla. • The ampulla unites with the proximal portion of the seminal vesicle to form the ejaculatory duct. Ductus Deferens Figure 28.15 Ejaculatory Duct • Formed by a uniting of the ductus deferens and the seminal vesicle • Located within the substance of the prostate gland between 1–2 cm long and conducts sperm from the ductus deferens to the prostatic urethra Ejaculatory Duct Figure 28.15 Urethra • • Transports semen from both ejaculatory ducts to the outside of the body The male urethra is subdivided into three regions: 1. prostatic urethra 2. membranous urethra 3. spongy urethra Urethra Figure 28.15 Accessory Glands • • • There are three glands that secrete fluids to mix with sperm to create seminal fluid. These secretions nourish the sperm and neutralize the acidity of the vagina. The three glands are as follows: 1. 2. 3. seminal vesicles prostate gland bulbourethral glands Seminal Vesicles • The paired seminal vesicles are located on the posterior surface of the urinary bladder lateral to the ampulla of the ductus deferens. • They secrete a viscous, whitish-yellow, alkaline fluid containing fructose and prostaglandins. Seminal Vesicles Figure 28.15 Seminal Vesicles and Prostate Gland Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Seminal vesicle Prostate gland Mucosal folds in seminal vesicle Tubuloalveolar glands in prostate gland LM 25x (a) Seminal vesicle LM 80x (b) Prostate gland a: © Carolina Biological/Visuals Unlimited; b: © The McGraw-Hill Companies, Inc./Photo by Dr. Alvin Telser Figure 28.16 Prostate Gland • The prostate gland is located immediately inferior to the urinary bladder. • It produces substances that are secreted directly into the prostatic urethra. • Prostatic secretion is slightly acidic and contains mucin, citric acid (nutrient for sperm), seminalplasmin (antibacterial),and prostaticspecific antigen (PSA, an enzyme that helps liquify semen). Prostate Gland Figure 28.15 Prostate Gland Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Ureters Urinary bladder Pubic symphysis Ampulla of ductus deferens Ductus deferens Seminal vesicle Ejaculatory duct Urogenital diaphragm Prostate gland Bulbourethral gland Urethra Anus Penis Epididymis Glans Testis Scrotum Figure 28.11 Bulbourethral Glands • The bulbourethral glands are located in the urogenital diaphragm on either side of the membranous urethra. • Mucin is secreted from these glands and enters the spongy urethra at the base of the penis. Bulbourethral Glands Figure 28.15 Semen • Seminal fluid from the three accessory glands combines with sperm from the testes to make up semen. • When released during intercourse, semen is called ejaculate. • Semen normally measures about 3–5 ml in volume and contains 200– 500 million sperm. Penis • The penis and the scrotum form the external genitalia in males. • Internally, the attached portion of the penis is the root forming both the bulb and the crura of the penis. • The body (shaft) is the elongated portion of the penis. • The tip of the penis is the glans, which surrounds the external urethral orifice. Anatomy of the Penis Figure 28.17 Penis The shaft of the penis is comprised of three parallel, cylindrical erectile bodies: 1. Paired corpora cavernosa are located dorsolaterally and terminate at the distal shaft of the penis 2. A single corpus spongiosum is inferior and midline and surrounds the spongy urethra 3. The distal end of the corpus spongiosum continues within the glans Anatomy of the Penis Figure 28.17 Circumcision Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Prepuce (a) Circumcised penis (b) Uncircumcised penis Erection and Ejaculation • The erectile bodies are composed of venous spaces, which fill with blood from a central artery to produce an erection. • Parasympathetic in nervation is responsible for penile erection. • Ejaculation is the expelling of semen from the penis, in part, by the rhythmic contraction of the smooth muscle of the urethra. • Sympathetic in nervation promotes ejaculation. Development of the Reproductive Systems Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Sexually Indifferent Stage Mesonephros Mesonephric duct Genital ridge Paramesonephric duct Kidney Cloaca Weeks 5–6 Female Male Testes Ovaries Efferent ductules Paramesonephric duct forming the uterine tube Epididymis Mesonephric duct (degenerating) Paramesonephric duct (degenerating) Mesonephric duct forming the ductus deferens Fused paramesonephric ducts forming the uterus Urinary bladder (moved aside) Urinary bladder Seminal vesicle Urogenital sinus forming the urethra Urogenital sinus forming the urethra and inferior vagina Weeks 10–12 Weeks 10–12 Uterine tube Urinary bladder Ovary Seminal vesicle Uterus Prostate gland Bulbourethral gland Ductus deferens Urinary bladder (moved aside) Vagina Figure 28.18 Urethra Epididymis Efferent ductules Testis Urethra Hymen At birth At birth Development of the Reproductive Systems Figure 28.19