Popma_TRACER
advertisement
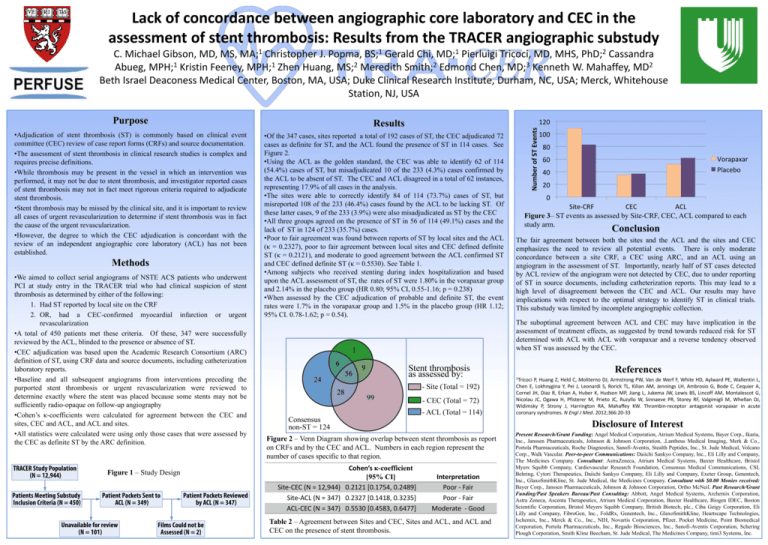
Lack of concordance between angiographic core laboratory and CEC in the assessment of stent thrombosis: Results from the TRACER angiographic substudy C. Michael Gibson, MD, MS, MA;1 Christopher J. Popma, BS;1 Gerald Chi, MD;1 Pierluigi Tricoci, MD, MHS, PhD;2 Cassandra 1 1 2 2 3 2 Abueg, MPH; Kristin Feeney, MPH; Zhen Huang, MS; Meredith Smith; Edmond Chen, MD; Kenneth W. Mahaffey, MD Beth Israel Deaconess Medical Center, Boston, MA, USA; Duke Clinical Research Institute, Durham, NC, USA; Merck, Whitehouse Station, NJ, USA Purpose •Adjudication of stent thrombosis (ST) is commonly based on clinical event committee (CEC) review of case report forms (CRFs) and source documentation. •The assessment of stent thrombosis in clinical research studies is complex and requires precise definitions. •While thrombosis may be present in the vessel in which an intervention was performed, it may not be due to stent thrombosis, and investigator reported cases of stent thrombosis may not in fact meet rigorous criteria required to adjudicate stent thrombosis. •Stent thrombosis may be missed by the clinical site, and it is important to review all cases of urgent revascularization to determine if stent thrombosis was in fact the cause of the urgent revascularization. •However, the degree to which the CEC adjudication is concordant with the review of an independent angiographic core laboratory (ACL) has not been established. Methods •We aimed to collect serial angiograms of NSTE ACS patients who underwent PCI at study entry in the TRACER trial who had clinical suspicion of stent thrombosis as determined by either of the following: 1. Had ST reported by local site on the CRF 2. OR, had a CEC-confirmed myocardial infarction or urgent revascularization •A total of 450 patients met these criteria. Of these, 347 were successfully reviewed by the ACL, blinded to the presence or absence of ST. •CEC adjudication was based upon the Academic Research Consortium (ARC) definition of ST, using CRF data and source documents, including catheterization laboratory reports. •Baseline and all subsequent angiograms from interventions preceding the purported stent thrombosis or urgent revascularization were reviewed to determine exactly where the stent was placed because some stents may not be sufficiently radio-opaque on follow-up angiography •Cohen’s κ-coefficients were calculated for agreement between the CEC and sites, CEC and ACL, and ACL and sites. •All statistics were calculated were using only those cases that were assessed by the CEC as definite ST by the ARC definition. Figure 1 – Study Design Results •Of the 347 cases, sites reported a total of 192 cases of ST, the CEC adjudicated 72 cases as definite for ST, and the ACL found the presence of ST in 114 cases. See Figure 2. •Using the ACL as the golden standard, the CEC was able to identify 62 of 114 (54.4%) cases of ST, but misadjudicated 10 of the 233 (4.3%) cases confirmed by the ACL to be absent of ST. The CEC and ACL disagreed in a total of 62 instances, representing 17.9% of all cases in the analysis. •The sites were able to correctly identify 84 of 114 (73.7%) cases of ST, but misreported 108 of the 233 (46.4%) cases found by the ACL to be lacking ST. Of these latter cases, 9 of the 233 (3.9%) were also misadjudicated as ST by the CEC •All three groups agreed on the presence of ST in 56 of 114 (49.1%) cases and the lack of ST in 124 of 233 (35.7%) cases. •Poor to fair agreement was found between reports of ST by local sites and the ACL (κ = 0.2327), poor to fair agreement between local sites and CEC defined definite ST (κ = 0.2121), and moderate to good agreement between the ACL confirmed ST and CEC defined definite ST (κ = 0.5530). See Table 1. •Among subjects who received stenting during index hospitalization and based upon the ACL assessment of ST, the rates of ST were 1.80% in the vorapaxar group and 2.14% in the placebo group (HR 0.80; 95% CI, 0.55-1.16; p = 0.238) •When assessed by the CEC adjudication of probable and definite ST, the event rates were 1.7% in the vorapaxar group and 1.5% in the placebo group (HR 1.12; 95% CI. 0.78-1.62; p = 0.54). Figure 3– ST events as assessed by Site-CRF, CEC, ACL compared to each study arm. Conclusion The fair agreement between both the sites and the ACL and the sites and CEC emphasizes the need to review all potential events. There is only moderate concordance between a site CRF, a CEC using ARC, and an ACL using an angiogram in the assessment of ST. Importantly, nearly half of ST cases detected by ACL review of the angiogram were not detected by CEC, due to under reporting of ST in source documents, including catheterization reports. This may lead to a high level of disagreement between the CEC and ACL. Our results may have implications with respect to the optimal strategy to identify ST in clinical trials. This substudy was limited by incomplete angiographic collection. The suboptimal agreement between ACL and CEC may have implication in the assessment of treatment effects, as suggested by trend towards reduced risk for ST determined with ACL with ACL with vorapaxar and a reverse tendency observed when ST was assessed by the CEC. References 1Tricoci P, Huang Z, Held C, Moliterno DJ, Armstrong PW, Van de Werf F, White HD, Aylward PE, Wallentin L, Chen E, Lokhnygina Y, Pei J, Leonardi S, Rorick TL, Kilian AM, Jennings LH, Ambrosio G, Bode C, Cequier A, Cornel JH, Diaz R, Erkan A, Huber K, Hudson MP, Jiang L, Jukema JW, Lewis BS, Lincoff AM, Montalescot G, Nicolau JC, Ogawa H, Pfisterer M, Prieto JC, Ruzyllo W, Sinnaeve PR, Storey RF, Valgimigli M, Whellan DJ, Widimsky P, Strony J, Harrington RA, Mahaffey KW. Thrombin-receptor antagonist vorapaxar in acute coronary syndromes. N Engl J Med. 2012;366:20-33 Disclosure of Interest Figure 2 – Venn Diagram showing overlap between stent thrombosis as report on CRFs and by the CEC and ACL. Numbers in each region represent the number of cases specific to that region. Cohen’s κ-coefficient [95% CI] Site-CEC (N = 12,944) 0.2121 [0.1754, 0.2489] Site-ACL (N = 347) 0.2327 [0.1418, 0.3235] ACL-CEC (N = 347) 0.5530 [0.4583, 0.6477] Interpretation Poor - Fair Poor - Fair Moderate - Good Table 2 – Agreement between Sites and CEC, Sites and ACL, and ACL and CEC on the presence of stent thrombosis. Present Research/Grant Funding: Angel Medical Corporation, Atrium Medical Systems, Bayer Corp., Ikaria, Inc., Janssen Pharmaceuticals, Johnson & Johnson Corporation, ,Lantheus Medical Imaging, Merk & Co., Portola Pharmaceuticals, Roche Diagnostics, Sanofi-Aventis, Stealth Peptides, Inc., St. Jude Medical, Volcano Corp., Walk Vascular. Peer-to-peer Communications: Daiichi Sankyo Company, Inc., Eli Lilly and Company, The Medicines Company. Consultant: AstraZeneca, Atrium Medical Systems, Baxter Healthcare, Bristol Myers Squibb Company, Cardiovascular Research Foundation, Consensus Medical Communications, CSL Behring, Cytori Therapeutics, Daiichi Sankyo Company, Eli Lilly and Company, Exeter Group, Genentech, Inc., GlaxoSmithKline, St. Jude Medical, the Medicines Company. Consultant with $0.00 Monies received: Bayer Corp., Janssen Pharmaceuticals, Johnson & Johnson Corporation, Ortho McNeil. Past Research/Grant Funding/Past Speakers Bureau/Past Consulting: Abbott, Angel Medical Systems, Archemix Corporation, Astra Zeneca, Ascenta Therapeutics, Atrium Medical Corporation, Baxter Healthcare, Biogen IDEC, Boston Scientific Corporation, Bristol Meyers Squibb Company, British Biotech, plc., Ciba Geigy Corporation, Eli Lilly and Company, FibroGen, Inc., FoldRx, Genentech, Inc., GlaxoSmithKline, Heartscape Technologies, Ischemix, Inc., Merck & Co., Inc., NIH, Novartis Corporation, Pfizer, Pocket Medicine, Point Biomedical Corporation, Portola Pharmaceuticals, Inc., Regado Biosciences, Inc., Sanofi-Aventis Corporation, Schering Plough Corporation, Smith Kline Beecham, St. Jude Medical, The Medicines Company, timi3 Systems, Inc.