On Track Provider Self Assessment Tool
advertisement
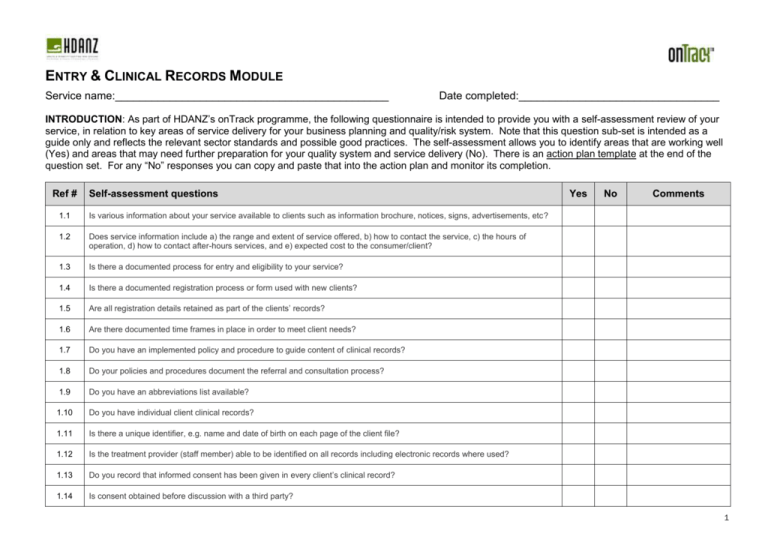
ENTRY & CLINICAL RECORDS MODULE Service name:_____________________________________________ Date completed:_________________________________ INTRODUCTION: As part of HDANZ’s onTrack programme, the following questionnaire is intended to provide you with a self-assessment review of your service, in relation to key areas of service delivery for your business planning and quality/risk system. Note that this question sub-set is intended as a guide only and reflects the relevant sector standards and possible good practices. The self-assessment allows you to identify areas that are working well (Yes) and areas that may need further preparation for your quality system and service delivery (No). There is an action plan template at the end of the question set. For any “No” responses you can copy and paste that into the action plan and monitor its completion. Ref # Self-assessment questions 1.1 Is various information about your service available to clients such as information brochure, notices, signs, advertisements, etc? 1.2 Does service information include a) the range and extent of service offered, b) how to contact the service, c) the hours of operation, d) how to contact after-hours services, and e) expected cost to the consumer/client? 1.3 Is there a documented process for entry and eligibility to your service? 1.4 Is there a documented registration process or form used with new clients? 1.5 Are all registration details retained as part of the clients’ records? 1.6 Are there documented time frames in place in order to meet client needs? 1.7 Do you have an implemented policy and procedure to guide content of clinical records? 1.8 Do your policies and procedures document the referral and consultation process? 1.9 Do you have an abbreviations list available? 1.10 Do you have individual client clinical records? 1.11 Is there a unique identifier, e.g. name and date of birth on each page of the client file? 1.12 Is the treatment provider (staff member) able to be identified on all records including electronic records where used? 1.13 Do you record that informed consent has been given in every client’s clinical record? 1.14 Is consent obtained before discussion with a third party? Yes No Comments 1 1.15 Is consent for treatment, change in treatment plan or change of provider documented? 1.16 If you accept students as observers in your service, do you have a policy and procedure to guide the process of teaching/observing/patient consent? 1.17 Are clients consulted and are their individual needs identified? 1.18 Is there a relevant assessment process which identifies the goals and needs of the client? 1.19 Are specific cultural values and beliefs of the consumer identified and recorded where appropriate? 1.20 Does the process for recording clinical information result in subjective and objective assessment, analysis, consumer goal setting, management and/or referral? 1.21 Are goals comprehensive, functional, client focused and SMART (Specific, Measurable, Attainable, Relevant and Time-framed) and is there evidence that these have been reviewed? 1.22 Are warnings, dosage and site location clearly annotated in the client record? 1.23 Are there risk and warning signs where appropriate (including warnings for use of gym equipment)? 1.24 Are warnings for treatment provided to clients for all modalities and recorded in records? 1.25 When referring clients to other service providers, do you record in the clinical record? 1.26 Is there a policy and procedure to guide when and how second opinions are accessed? 1.27 Are clients advised of their right to seek a second opinion as identified? 1.28 Is there a SOATAP clinical record for each visit? 1.29 Are clinical notes legible, dated and signed at each episode including electronic records (if used)? 1.30 Do policies and procedures guide the safe use and prescription of therapeutic goods and/or medical devices including procedures in place to guide the monitoring of adverse events? 1.31 Do you document allergies or adverse reactions in the client record 1.32 Is there evidence that clients are being appropriately instructed in the use of equipment, medicines or therapeutic goods supplied? 1.33 Do you have policies and procedure/s which guide the ongoing review of clinical practice 1.34 Are treatment interventions reviewed? 1.35 Are goals reviewed and evaluated with the client and do they have specific timeframes for achievement? 2 1.36 Do clinical records provide evidence that the client has received advice for post-treatment care/follow up? 1.37 Do you have a policy and procedure/s which guides the discharge process? 1.38 Are follow-up requirements recorded in the clinical record? 1.39 Are discharge summaries written? 1.40 Is there a recall system for clients? 1.41 Is there a system to manage DNAs? 1.42 Are case reviews/clinical records audits performed on a regular basis? Reminder: you can use the clinical records review format in the OnTrack tools resources located in Phase 4 (Act). 1.43 Does your service have a shredder or other appropriate resources for safe and secure document destruction? 1.44 Is there a policy and procedure for the removal and/or transportation of client records from the main site? 1.45 Is daily backup of your computer system undertaken and kept off site? 3 ACTION PLAN: ENTRY & CLINICAL RECORDS MODULE Ref # Self-assessment questions (for “No” responses above) Improvement action to be taken Due date Person responsible Date completed (Add additional rows as necessary) 4