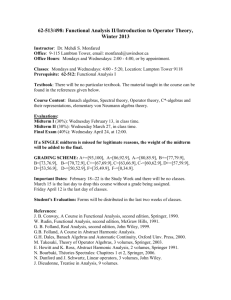
HSSP 104: Health Economics
Heller School for Social Policy and Management
Brandeis University
Spring 2014
SYLLABUS
Instructor: Dominic Hodgkin
Office: Heller 264
Email: hodgkin@brandeis.edu
Telephone: 6-8551
Teaching Assistant: Ramandeep Kaur
Office: Heller 144
Email: rkaur@brandeis.edu
Description: This course will teach students to apply economic analytical approaches to the health
sector, in areas where this adds insights. Relevant tools include cost-benefit and cost-effectiveness
analysis, theories of demand, supply, adverse selection, moral hazard and price discrimination.
Learning goals: After taking this class, students should be able to use the tools of economic analysis
to evaluate issues in health care policy and research.
Prerequisite: Econ 2a.
Evaluation: The course grade will be determined by a midterm (25%), a final exam (30%), a research
paper (15%), responses to readings (10%), homework assignments (15%), and attendance/
punctuality/participation (5%).
The requirements for the responses to readings are outlined in a separate document posted on Latte.
The schedule of due dates for assignments is posted on Latte too.
Laptops are allowed in class for note-taking purposes, but use for non-class related purposes is
discouraged, and will affect your participation grade negatively.
Academic integrity: You are expected to be familiar with and to follow the University’s policies
on academic integrity (see http://www.brandeis.edu/studentlife/sdc/ai ). Any suspected instances
of alleged dishonesty may be referred to the Office of Student Development and Conduct.
Instances of academic dishonesty may result in sanctions including but not limited to, failing
grades being issued, educational programs, and other consequences.
Disabilities: If you are a student with a documented disability on record at Brandeis University and
wish to have a reasonable accommodation made for you in this class, please see me immediately.
Textbook: Folland S., Goodman A. and Stano M., Economics of Health and Health Care. 7th edition.
Pearson Prentice-Hall, 2013.
We will also read portions of:
The Economics of Health Care Reconsidered, 3rd edition, by Rice T. and Unruh L. The relevant
portions are available on the course website. So are the other assigned readings listed below.
3/14/2016
1
CLASS SCHEDULE AND READINGS
1. Introduction
1/14
Folland et al, chapters 2-3. This is a review of relevant microeconomics and statistics tools. If you
have not had much exposure to this material, you are strongly recommended to review it now.
2. US health care sector
1/16
Folland et al, chapter 1.
Martin, A. B., Hartman M., Whittle L., Catlin, A. (2014). National Health Spending In 2012:
Rate Of Health Spending Growth Remained Low For The Fourth Consecutive Year. Health
Affairs, 33(1), 67-77.
Cutler, D. M., & Sahni, N. R. (2013). If slow rate of health care spending growth persists,
projections may be off by $770 billion. Health Affairs, 32(5), 841-850.
3. Production of health
1/21
Folland et al, chapter 5.
Cutler D., Deaton A., Lleras-Muney A. (2006). The Determinants of Mortality. Journal of Economic
Perspectives 20(3): 97-120.
Garber A.M., Skinner J. (2008). Is American Health Care Uniquely Inefficient? J Econ Perspectives
22(4): 27–50.
4. Production/cost of health care
1/23
Folland et al, chapter 6.
Schneider J.E., Miller T.R., Ohsfeldt R.L. et al (2008). The economics of specialty hospitals. Medical
Care Research & Review 65(5): 531-53.
Guterman S. (2006). Specialty hospitals: a problem or a symptom? Health Affairs: 25(1):95-105.
5. Cost-benefit analysis
1/28
Folland et al, chapter 4, pp.63-76.
3/14/2016
2
Hueston W.J., Benitch J.J. (2004). A Cost-Benefit Analysis of Testing for Influenza A in High-Risk
Adults. Annals of Family Medicine 2:33-40 (2004).
6. Cost-effectiveness analysis
1/30
Folland et al, chapter 4, pp.76-81.
Shepard D.S., Thompson A.S. (1979). First principles of cost-effectiveness analysis in health. Public
Health Reports 94(6): 535-543.
Canning D. (2006). The economics of HIV/AIDS in low-income countries: the case for prevention. J
Econ Perspectives 20(3):121-42.
Boelaert M., Van Damme W., Meessen B., Van der Stuyft P. (2002). The AIDS crisis, costeffectiveness and academic activism. Trop Med Int Health 7(12):1001-2.
Kahn, J.G.., et al. "Cost-effectiveness of antiretroviral therapy for prevention." Current HIV research
9.6 (2011): 405.
7. Demand for health insurance
2/4
Folland et al, chapter 8.
Rice and Unruh, chapter 4, pp. 57-81.
Baicker, K., Congdon, W. J., & Mullainathan, S. (2012). Health Insurance Coverage and Take‐Up:
Lessons from Behavioral Economics. Milbank Quarterly, 90(1), 107-134.
8. Equity, efficiency and need
2/6
(NOTE: At Sherman Hall)
Folland et al, chapter 18
Rice and Unruh, chapter 9: Equity and redistribution.
Cohen, J. P., Stolk, E., & Niezen, M. (2008). Role of budget impact in drug reimbursement
decisions. Journal of Health Politics, Policy and Law, 33(2), 225-247.
Ubel P.A., Loewenstein G. (1996). Public perceptions of the importance of prognosis in allocating
transplantable livers to children. Med Decis Making 16(3):234-41.
9. Demand for health care
2/11
Folland et al, chapter 9.
Rice and Unruh, chapter 4, pp. 82-116.
3/14/2016
3
Nyman J.A. (2004). Is 'moral hazard' inefficient? The policy implications of a new theory. Health
Affairs 23(5):194-199.
Baicker K., and Finkelstein A. "The effects of Medicaid coverage—learning from the Oregon
experiment." New England Journal of Medicine 365.8 (2011): 683-685.
Mahoney, J. J., Lucas K., Gibson, T. B., Ehrlich, E. D., Gatwood, J., Moore, B. J., & Heithoff, K. A.
(2013). Value-Based Insurance Design: Perspectives, Extending the Evidence, and Implications for the
Future. American Journal of Managed Care, 2013.
10. Insurance game
[no readings]
2/13
[no class on 2/18, 2/20: February break]
11. Asymmetric information
2/25
Folland et al, chapter 10.
MIDTERM EXAM
2/27
12. Physician services markets
3/4
Folland et al, chapter 15.
Phelps C.E. (1992). Diffusion of information in medical care. Journal of Economic Perspectives 6(3):
23-42.
Hollingsworth, J.M., et al. "Physician-ownership of ambulatory surgery centers linked to
higher volume of surgeries." Health Affairs 29.4 (2010): 683-689.
Dartmouth Atlas of Health Care (2010). Trends and Regional Variation in Carotid Revascularization.
13. Health insurance markets
3/6
Folland et al, chapter 11.
Buchmueller T.C., Monheit A.C. (2009). Employer-sponsored health insurance and the promise of
health insurance reform. Inquiry 46(2): 187-202.
Lavarreda, S. A., Brown, E. R., & Bolduc, C. D. (2011). Underinsurance in the United States:
An interaction of costs to consumers, benefit design, and access to care. Annual Review of
Public Health, 32, 471-82.
14. The uninsured
3/11
Gruber, J. ( 2008). Covering the Uninsured in the United States. Journal of Economic Literature 46(3):
571-606.
3/14/2016
4
Kaiser Family Foundation (2013). The Uninsured: A Primer - Key Facts about Health Insurance on the
Eve of Coverage Expansions.
15. Provider reimbursement
3/13
Folland et al, chapter 20 (pp. 412-424).
McClellan, M. (2011). Reforming payments to healthcare providers: The key to slowing
healthcare cost growth while improving quality?. The Journal of Economic Perspectives,
25(2), 69-92.
Werner R.M., Dudley R.A. (2009). Making The ‘Pay’ Matter In Pay-For-Performance: Implications
For Payment Strategies. Health Affairs 28(5): 1498-1508.
16. Managed care
3/18
Folland et al, chapter 12.
Burns, L. R., Pauly, M.V. (2012). Accountable care organizations may have difficulty
avoiding the failures of integrated delivery networks of the 1990s. Health Affairs, 31(11),
2407-2416.
Chernew, M.E., et al. "Private-payer innovation in Massachusetts: the ‘alternative quality
contract’." Health Affairs 30.1 (2011): 51-61.
17. Nonprofit firms
3/20
Folland et al, chapter 13.
Schlesinger M., Gray B.H. (2006). How nonprofits matter in American medicine, and what to do
about it. Health Affairs. 2006 Jul-Aug;25(4):W287-303.
Cram, P., Bayman, L., Popescu, I., Vaughan-Sarrazin, M. S., Cai, X., & Rosenthal, G. E. (2010).
Uncompensated care provided by for-profit, not-for-profit, and government owned hospitals. BMC
health services research, 10(1), 90.
3/14/2016
5
18. Pharmaceutical industry
3/25, 3/27
Folland et al, chapter 17
Berndt, E. R., McGuire, T., & Newhouse, J. P. A Primer on the Economics of Prescription
Pharmaceutical Pricing in Health Insurance Markets. In Forum for Health Economics & Policy (Vol.
14, No. 2, p. 10).
Wood, A. J. (2006). A proposal for radical changes in the drug-approval process. New
England Journal of Medicine, 355(6), 618-623.
Berndt E.R., Donohue J.M. (2008). Direct to consumer advertising in health care: an overview of
economic issues. In: Sloan FA, Kasper H; Incentives and choice in health care. MIT Press.
19. Government intervention
4/1
Folland et al, chapter 19; chapter 20 (pp. 407-412)
Rice and Unruh, chapter 3 (role of government)
Ho, V., & Ku-Goto, M. H. (2013). State Deregulation and Medicare Costs for Acute Cardiac Care.
Medical Care Research and Review, 70(2), 185-205.
20. Social insurance
4/3
Folland et al, chapter 21
Brecher, C., & Rose, S. (2013). Medicaid's Next Metamorphosis. Public Administration
Review, 73(s1), S60-S68.
Duggan M., Healy P., Scott Morton F. (2008). Providing Prescription Drug Coverage to the Elderly:
America's Experiment with Medicare Part D. Journal of Economic Perspectives 22(4): 69–92.
21. International comparison: Other developed countries
4/8
Folland et al, chapter 22.
Rice and Unruh, chapter 10.
Ellis, R. P., Chen, T., & Luscombe, C. E. (2013). Comparisons of Health Insurance Systems in
Developed Countries. Encyclopedia of Health Economics; Culyer, AJ, Ed.; Elsevier: Amsterdam, The
Netherlands.
Stolpe M. Containing Public Health Spending Through Market-Based Health Reform in
Germany. In: Coady, D., & Gupta, S. (2012). The economics of public health care reform in
advanced and emerging economies. International Monetary Fund.
3/14/2016
6
22. US health system reform
4/10
Folland et al, chapter 23
Emanuel, E., Tanden, N., Altman, S., Armstrong, S., Berwick, D., de Brantes, F., ... & Spiro,
T. (2012). A systemic approach to containing health care spending. New England Journal of
Medicine, 367(10), 949-954.
Antos, J. R., Pauly, M. V., & Wilensky, G. R. (2012). Bending the cost curve through market-based
incentives. New England Journal of Medicine, 367(10), 954-958.
Buchmueller, T., Carey, C., & Levy, H. G. (2013). Will employers drop health insurance
coverage because of the affordable care act?. Health Affairs, 32(9), 1522-1530.
Hsiao, W. C., Knight, A. G., Kappel, S., & Done, N. (2011). What other states can learn from
Vermont’s bold experiment: Embracing a single-payer health care financing system. Health
Affairs, 30(7), 1232-1241.
(No class on 4/15, 4/17, 4/22: April break)
23. International comparison: Developing countries
4/24
Mills A. health systems in low- and middle-income countries. In: Glied S, Smith PC (2011): The
Oxford Handbook of Health Economics.
Bitrán R., Muñoz R., and Prieto L. "Health insurance and access to health services, health services use
and health status in Peru." The Impact of Health Insurance in Low and Middle Income Countries
(2011): 106-21.
24. Review session
4/29
Final exam: 5/5, 6-9 pm
3/14/2016
7