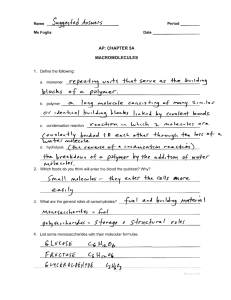
Why did this happen? - Healthcare Accreditation Consultants
advertisement

Sentinel Events 2014 Speaker John R. Rosing, MHA, FACHE Accreditation and Regulatory Compliance Consultant Vice President and Principal Patton Healthcare Consulting 262-242-3631 JohnRosing@PattonHC.com 2 Most Frequently Reported Sentinel Events, January 1–June 30, 2013 (Source: 10/13 Perspectives) • • • • • • • • • • Wrong-patient, wrong-site, or wrong-procedure—60 Unintended retention of a foreign object—56 Delay in treatment†—56 Falls†—48 Other unanticipated events† ‡—40 Operative/postoperative complication†—37 Suicide—35 Criminal event (assault/rape/homicide)—26 Medication error†—20 Perinatal death/injury†—15 – † Resulting in death or permanent loss of function – ‡ Includes asphyxiation, burns, choking, drowning, and being found unresponsive Most Frequently Identified Root Causes for Sentinel Events, January 1–June 30, 2013 (Source: 10/13 Perspectives) • • • • • • • • • • Human factors (such as fatigue or distraction)—314 Communication (such as among staff, across disciplines, or with patients)—292 Leadership (regarding, for example, lack of performance improvement infrastructure or community relations)—276 Assessment (such as patient observation processes or its documentation)—246 Information management (such as patient identification or confidentiality)—101 Physical environment (such as emergency management or hazardous materials)—70 Care planning (planning and/or interdisciplinary collaboration)—49 Continuum of care (includes transfer and/or discharge of patient)—48 Medication use (such as storage/control or labeling)—48 Operative care (such as blood use or patient monitoring)—45 Sentinel Event Defined • A sentinel event is an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes loss of limb or function. The phrase “or the risk thereof” includes any process variation for which a recurrence would carry a significant chance of a serious adverse outcome. • The terms “sentinel event” and “medical error” are not synonymous; not all sentinel events occur because of an error and not all errors result in sentinel events. RCA Value? • Root causes vs proximate causes – The barn door was left open and all the horses ran away. Close the barn door now – problem solved – Mary made a serious medication error, fire Mary – problem solved • Could someone else forget to close the barn door, could someone else make the same error as Mary? 6 RCA Value • Why was the barn door left open? – There was no automatic door closing mechanism, inadequate training, procedural noncompliance • Why did Mary make the medication error? – There was no bar coding support, inadequate orientation, inadequate training, no policy guidance, no secondary check on calculation – Procedural noncompliance – Mary duplicated all her patients wrist bands and unit dose bar codes. Still need to understand the why, but actions may be different • Action plan and measurement phase enables you to redesign for additional safety and monitor 7 RCA Value (cont’d) • Action plan – you create system changes that help protect against the same error being repeated • Measurement – you self assess to determine if the changes you designed are being used as anticipated and do they prevent the weakness you had previously seen. Have you sustained the improvement?? 8 RCA Process • The decision to pro-actively report or not report to the Joint Commission is voluntary…. • The decision to analyze or not analyze using RCA technique is not voluntary under the standards and SE policy • If the Joint Commission becomes aware of your sentinel event, reporting using one of their techniques, is mandatory 9 When To Conduct An RCA TJC Reportable All events that meet your internal definition, including near misses 10 RCA Process (cont’d) • Don’t confuse reporting responsibilities and deadlines with deadlines for completing the RCA – You must complete the RCA within 45 days of the event, or your becoming aware of the event 11 Do We Ever Skip The RCA? “It was evident that our problem was a physician performance issue, should we just make the referral to peer review and skip the RCA?” – Did your system for error prevention work as designed? – Did your OPPE, FPPE system identify this vulnerability? – Were prior peer evaluations thorough? – Were privileges granted appropriately? 12 What is a Root Cause Analysis? • A credible process for identifying the basic or causal factors that underlie variation in performance. • This process should be used to identify the risk that led to a sentinel event. • Use a RCA framework to drill down to root cause; complete within 45 days Starting With The Basics Define Your Goals • Your goal: To conduct a complete, thorough investigation of the event or near miss • Why? To ensure you have identified the real cause or causes of the incident • Why? So you can prevent this situation from occurring again 14 Starting With The Basics Getting Organized Organize your RCA efforts: – Centralize coordination and oversight responsibilities to one department • Allows for better trending of results • Provides for monitoring to ensure actions have taken place and results are achieved – Have a written process for conducting the RCA • • • • Maintains process consistency Prevents solution “short cuts” Ensures important steps are not forgotten Provides reporting structure and follow up 15 Putting Together The RCA Team Roles and Responsibilities • Team Leader – Select wisely – Usually someone in a leadership position • Director, manager or higher – Usually from one of the involved departments – Should be a strong, fair person who can reign in group members when needed – Someone who will not push to solve the problem before all the facts are uncovered 16 Putting Together The RCA Team Roles and Responsibilities (cont’d) • Team Facilitator • Often someone in Performance Improvement, Patient Safety or Risk Management • Experienced in facilitation • Understands how to conduct an RCA • Can provide “just in time” training for members • Familiar with tools such as brainstorming, Fishbone & Event Flow Diagrams • Organized 17 Putting Together The RCA Team Roles and Responsibilities (cont’d) • Team Members – Rule of thumb keep the group “workable” 6-8 members is ideal – When possible include those staff/physicians directly involved in event • Exceptions– Too emotionally or personally involved – May be an obstructionist to a good process 18 Starting The RCA Where Do You begin? • Step one: What happened? • Identify the key components in the event: – Who were the people/departments/areas involved in this event? – What Equipment, if any was involved? – What are the key Systems, Processes and Patient Safety Measures that were involved? 19 Gathering The Facts What Happened? • Gather the facts- and just the facts. Do not get bogged down in extraneous details that can actualize dilute or divert the focus off the key issues • Ways to gather the facts include: – – – – – Interviews Chart reviews On-line documentation Event reports Other data, policies, procedures 20 Gathering The Facts and Just The Facts – Interview Tips- focus on cooperation not interrogation – Chart reviews- documentation and sequencing of events, create a time line of events – Event reports- Making sure it is completed with documented follow up – Secure equipment- get it before it is gone – The other “Stuff” you need - policies, procedures, documents 21 How Deep Do You Dig? • Getting to the root cause is somewhat like peeling back the layers of an onion until you reach the core • A thorough RCA methodically asks the question “why” until there is no further to go- until every layer surrounding the core has been removed and you are comfortable you have reached the real root cause 22 Tools To Help With The RCA Constructing “What Happened”? Step two- Begin to put things together An event flow diagram is a great place to start putting the facts together – It is a tool that sequences the steps in the event and provides you with a chronology of the facts surrounding the event – It helps to focus the group on the actual steps in this event- not how things should occur – It helps the group identify where there may have been a breakdown in process that led to the event occurring 23 Tools To Help With The RCA • Let’s walk through a very simplified example to see how we would create the event flow diagram • This is a case of Near Miss in the emergency room 24 Tools To Help With The RCA (cont’d) • Sequence of Events – Mr. G, an unaccompanied patient, walked in the Emergency Room and signed in at the triage desk at 8:45 PM – Triage nurse was assessing another patient when patient signed in and did not see patient. Security guard was present at desk – 9:10 PM Patient with Chest Pain arrived in ED. Triage Nurse immediately assessed Chest Pain patient – 10 PM Nursed called for Mr. G. and patient did not respond – 10:10 Security checked waiting room and found patient unconscious. Waiting room was full of patients – 10:11 Emergency Code was called and patient was transported to treatment bay – 10:13 Blood sugar found to be 37 – Patient was treated, kept in observation overnight and discharged the next morning 25 Tools To Help With The RCA (cont’d) • Simplified Event Flow 8:45 Mr. G Signs in at Triage 10:11 Code Called Pt to TX bay 9:10 PT With CP Arrives At triage 10:13 Mr.G’s BS 37 10:00 Nurse Calls for Mr. G No response Mr. G treated Observed overnight 10:10 Security Finds Mr. G Unresponsive Mr. G D/C home in AM 26 Tools To Help With The RCA (cont’d) • Why did this happen? • Focus the group on trying to uncover “Why” this event happened • Identify all of the “whys” • Resist the temptation to jump to the solution • Keeping asking “Why” until you can literally go no further- there is no additional information to be gleaned from asking “Why.” 27 Tools To Help With The RCA Brainstorming • Brainstorming is a great way to surface potential “Whys” • It gets everyone involved in process • Unleashes and uncovers multiple ideassolutions or possible causes • Can be “free flowing” or “structured” 29 Tools To Help With The RCA Brainstorming (cont’d) • Free Flowing– Members speak up as they have ideas – Scribe or facilitator write ideas on flip chart • Structured– Members are asked to jot down ideas on sticky notes – Go around the room using a round robin to give each member a chance to speak. Keep going around until no one has any more ideas 30 Tools To Help With The RCA Cause and Effect Diagram • Constructing a Fishbone or Cause and Effect Diagram can help the group organize facts and information into a single picture – It helps establish possible relationships – It can help to elicit additional information 31 Constructing The Diagram Organize the results of your “Brainstorming” into the contributing factors EXAMPLE: – – – – – Human factors Equipment factors Controllable environmental factors Uncontrollable environmental factors Other factors 32 Constructing The Diagram (cont’d) • Simplified example of Fishbone or Cause and Effect Diagram: Human Factors Sign in policy does not ensure pt is seen before sitting down Second triage nurse on breakrelief nurse did not show Equipment Factors Panic button in private waiting room nonfunctional Other Factors Environmental Factors Private waiting room design- poor visualization 33 Identify the Root Cause(s) Prune the list of Root Causes – Would the problem have occurred if cause #1 had not been present? – Will the problem recur due to same causal factor if cause #1 is corrected or eliminated? – Will correction or elimination of cause #1 still potentially lead to similar events? • Yes = contributing cause, No = root cause Taking Action • The Hardest Step In The RCA: Installing effective error prevention strategies • Make the right thing to do the easiest thing to do and then hard-wire it • Make the process fool-proof recognizing that nothing is outside the capability of a sufficiently talented fool! Taking Action Just Do It!! What can we do to prevent this from happening again? • You know what has happened • You know why it happened • Now you need to decide what you can do to prevent this from happening again • AND… actually take the steps to make the changes happen! 36 Taking Action Just Do It!! (cont’d) • Develop an action plan – List the Root Causes with the actions needed to prevent this event from happening again • Present the plan – Reporting structure should be established in your RCA policy- i.e. Patient Safety Committee • Assign responsibilities for action steps – These can be assigned prior to reporting to designated committee or afterwards 37 Taking Action Just Do It!! (cont’d) • Follow up on assignments – Usually facilitator or someone in PI, RM or PS keeps a tracking log • Report back – Require follow up to be reported back to designated committee • Close the loop – Monitor for lasting impact 38 Taking Action Step Common Obstacles and Problems • • • • • • • Fear Rushing to the solution Not gathering enough information Solving the wrong problem Making tough recommendations Implementing actions Doing the follow up- making sure the changes stick 39 Taking Action • You have completed your RCA • You have your team’s list of root causes for this event • You have drafted your action plan and measurement strategy – Who is going to approve the RCA? – Who is going to approve the action plan? – Who is going to approve the measurement strategy? • This should all be hard coded before you have a sentinel event 40 Importance of Approvals? • You need people to take action, change behaviors, change policy, potentially provide resources and support • You have a responsibility to measure change in accordance with your action plan – If there is inadequate buy in, your changes won’t be accepted, your measurement will not work, your accreditation can be downgraded and your patients may remain at risk 41 Action Plans • If your root causes include improper patient identification techniques….. – Is it lack of training, orientation, system to accomplish the technique, procedural non compliance or failure to provide leadership? • If your root causes include procedural non compliance or a failure to lead or fund, your action plan will be different 42 Broad The Scope? • Your SE involved incorrect patient identification in cardiac cath lab • Your root causes identified mis-application of the 2 identifier technique in cardiac cath • Your planned actions will focus on cardiac cath or on your organization? – Implement actions where ever you have risk, not just where this event occurred 43 Measurement Strategy • You identify a statistically valid sampling methodology before starting to measure and you collect audit data using that system – Try to collect passively, retrospectively – Concurrent data collection by responsible staff with new forms may create under reporting or artificial findings – Concurrent external observer studies may be more thorough • You average your 4 months of data and must achieve A or C level performance or if not linked to a standard 85% • Be sure to provide rapid, departmental and aggregate feedback each month and consider graphical analysis to promote change and improvement 44 Building On Success • Fostering the blame free atmosphere – Talk about your RCA process, the system changes, the resources that flowed, display the improvement data, the enhanced safety – This can be a positive change experience • Do analyze procedural noncompliance, was your design reasonable? 45 Root causes, failures, defects, workarounds, or undesired variation…… Are usually caused by one or more of the following…… • • • • • Poor process design Poor transfer of knowledge Poor validation of competency Poor measurement of conformance Poor management intervention 5 Steps to doing the Right Thing Well Sustained Execution=Continuous Readiness Measure conformance • Poor design? Intervention (appropriate action) • Inadequate education • Ineffective competency validation • Variation due to work-arounds • Variation due to unit, day of week, time of day, FT/PT/agency staff, etc. John R. Rosing, MHA, FACHE PI staff Measure conformance Staff dev. Validate competency Patton Healthcare Consulting Educate Focus/PDSA/Rapid cycle design Staff dev. PI team QUESTIONS? JohnRosing@PattonHC.com JenCowel@PattonHC.com Kurt@PattonHC.com Please visit and bookmark www.pattonhc.com 48