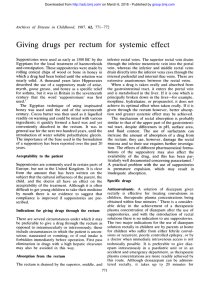
Suppositories and Pessaries
advertisement

Suppository Development and Production • Marion Gold Centerchem, Inc., Stamford, Connecticut. • Murti VePuri Able Labs, South Plainfield, New Jersey • Lawrence H. Block Duquesne University of, Pittsburgh, Pennsylvania 1 Introduction Oral route of administration is the most acceptable and common compared with other routs of administration. Oral route is not without limitations. Some medication cause local stomach irritation. Dose limitation. Certain patients, children, elderly, and those with swallowing problems, are difficult to treat with oral tablets and capsules. Target the medication to the affected area. Ophthalmic, Nasal, Otic, Dermal, Vaginal and Anorectal tissues. 2 Suppositories The suppositories are the neglected dosage form. Although lots of research done on this drug delivery system, there are continues to be a general rejection of the rectal delivery system. There are important reasons to consider suppositories as a preferred route of administration in many situation. 3 Why the rectal route? When the patient is unable to use the oral route Through, unconsuous, irritation in the stomach When the drug is less suited to oral administration 4 Definition Solid or semisolid dosage forms used for rectal, vaginal, or urethral administration of therapeutic agents. 5 Typically consist of dispersion of the active ingredient in an inert matrix generally composed of a rigid or semi-rigid base. This matrix should be inert not to interact with the active ingredients and the excipients. The dispersed phase can be incorporated into the suppository as: Solid (Powder). Liquid (either aqueous, alcoholic, or glycolic solutions, oils, extracts, etc. 6 The material for the base, are selected on the bases of its ability to soften, melt, or dissolve at body temperature. Finished suppositories are manufactured in a variety of shapes and sizes to best suit the treatment requirements (nature of the active ingredients, site of administration. Suppositories are available in a range of physical forms (molded or compressed, foil or plastic wrapped, or gelatin encapsulated. 7 Rectal administration & Applications 1. 2. For local Systemic drug delivery. 8 Drugs administered by rectal route Local Effect Astringents. Anti-septics. Local anaesthetics. Vasoconstrictors. Anti-inflammatory. Soothing agents. Protective agents. laxatives Systemic Effect Analgesic & antipyretic. Anti-inflammatory. Anti-asthmatic. Anti-convulsant. Anti-emetic. Nausea Narcotic analgesia (Oxymorphone HCL) 9 Advantages Reduce hepatic first-pass elimination Enhance drug bioavailability. Alcoholic and aqueous solution can be rapidly absorbed, and this is used to considerable advantage, for example, to administer diazepam in the treatment of acute convulsive attacks. 10 Comparison with Oral Delivery Many studies have attempted to compare the oral dosage form with the rectal administration. The results are inadequate, because of the different parameter used to make the studies, the experiment conditions and choice of excipient. Certain active ingredients are just not well suited for suppository dosage. 11 Diazepam (as an alcoholic solution & propranolol have been shown to exhibit greater bioavailability when administered rectally. Theophylline suppositories was found bioequivalence to oral administration when microcrystalline drug was used. Bioequivalence between pentobarbital despite its slower rectal absorption. In case where there is no first pass metabolism, it has been shown that rectal administration of drugs in solution can provide BE equivalent to that seen with oral administration. 12 Absorption of the materials is via passive diffusion; (no carrier-assisted means take part in the passage of drug through lipid membrane). Thus, success or failure of therapeutic delivery is a function of lipo-solubility of the agent as well as its vehicle, because the partition coefficient of the drug between suppository base and the lumen contents influences the latter's release into the bowel and eventually the actives passage through the wall of the intestine. 13 Enhancement agents that affect the mucous membrane similarly affect absorption and are useful for boosting delivery of poorly absorbed agents such as antibiotics and high M.W materials. 14 The use of suppositories in the world Rectal as well as urethral and vaginal delivery of drugs via suppositories makes excellent therapeutic sense, and there use can be traced as far back as in the writings of Hippocrates. In Japan, rectal dosage forms are more acceptable by the patient than other route of administration. More than 7.5% of all prescriptions in France were formulation intended for rectal administration. 15 Anglo-Saxon countries, where social convention preclude greater use of rectal delivery (generally do not prescribe suppositories). Latin American and Mediterranean Europeans use suppositories far more routinely. In summary the use of rectal suppositories is limited and are vary between nations. 16 Factors affecting the absorption from Rectal Suppositories 1. 2. 3. Physiological factors. Physicochemical factors of the drug substance. Physicochemical factors of the base. 17 1. Physiological Factors 1. Colonic content. 2. Circulation route. 3. pH, and lack of buffering capacity of the rectal fluids. 1. When systemic effects are desired, greater absorption may be expected from a rectum that is void then from one that is distended with fecal matter. An evacuant enema could be use before the administration of a suppository. 18 Physiological Factors continued Diarrhea, which case tissue dehydration of the rectum can influence the absorption. Colonic obstruction due to tumorous growths, influence the rate and the degree of drug absorption from the rectal site. 2. Circulation Route, drugs absorbed rectally, bypass the portal circulation during their first pass into the general circulation 19 3. pH and lack of buffering capacity of the rectal fluids. The rectal fluids are neutral in pH (7-8), and have no effective buffering capacity. The drug is administered will not generally be chemically changed by the rectal environment. The suppository base used has major influence on the release of active constituents incorporated into it. 20 Physicochemical Factors Includes: 1. Solubility of the drug in lipid and in water. 2. Particle size of dispersed drugs. 3. Physicochemical factors of the base include its ability to: Melt. Soften. Dissolve at body temperature. Release the drug substance, and its hydrophilic or hydrophobic character. 21 Lipid-water solubility: The lipid-water partition coefficient of a drug is an important factor in the selection of the suppository base and in drug release from that base. A Lipophilic drug that is distributed in a fatty suppository base in low concentration has less of a tendency to escape to the surrounding aqueous fluids than the hydrophilic substance presents in a fatty base. Water soluble base such as, PEG, which dissolve in the anorectal fluids, release for absorption both water soluble and oil soluble drugs. 22 Physicochemical Factors Continue… Particle size: Particle size of drugs present in the suppository in the undisclosed stat, the smaller the particle size the more readily the dissolution of the particles and the greater the chance for rapid absorption. Nature of the base: Melting point, softening, or dissolving to release its drug components for absorption, interacting with the drugs substance. 23 Ratio of Components Once the correct excipient has been selected, the proper proportion of the components needs to be established. One important aspect to consider in suppository formulation is that of displacement. Suppositories generally weigh between 1 to 4 g, and displacement of the excipient by the active ingredient must be calculated when the product is formulated. 24 Simply, this step takes into account the volume of suppository base that will be displaced by an insoluble drug dispersed into it. This is necessitated by the practice of placing weighed quantities of suppository ingredients into molds whose contents are measured volumetrically. 25 M = F - (f * S) M = the quantity (weight) of suppository base needed. F = the total capacity of the suppository mold. f = the displacement factor of the active ingredients. S = the quantity of the active ingredient per suppository. 26 Calculation of Displacement Value M = the quantity (weight) of suppository base needed. F = the total capacity of the suppository mold. f = the displacement factor of the active ingredients. S = the quantity of the active ingredient per suppository. 27 Displacement Value The volume of a suppository from a particular mould is uniform. The weight is vary according to the density of the medicaments. The displacement value of a drug is the number of parts by weight of drug which displaces one part by weight of the base. Could be calculated and could be found in the literature. 28 Displacement Factors of Selected Materials Acetylmorphine Hydrochloride 0.71 Acetylsalicylic acid 0.63 Beeswax 1.0 Benzocaine 0.68 Bismuth subgallate 0.37 Bismuth sbnitrate 0.33 0.33 Codeine phosphate 0.8 Glycerin 0.78 Phenacetin 0.6 Phenobarbital 0.84 Phenobarbital sodium 0.62 Procaine 0.8 Quinine chlorohdrate 0.83 Sulfamide 0.6 Theophylline 0.63 Zinc oxide 0.2 29 Formulation OK A. Choice of drug: What makes a particular drug a candidate for administration in the form of a suppository? 1) It must be sufficiently absorbed through the rectal mucosa to permit therapeutic blood levels. 2) Drug that are poorly absorbed after oral dosage. 3) Drugs that cause irritation to the gastrointestinal mucosa. 4) Certain antibiotics cause major changes to the balance of intestinal flora, and there would be better given as suppositories. 30 5) Small polypeptides-normally subject to the enzymatic activity of the upper GIT, can often be OK better administered via the rectum. 6) The pH of the upper GIT causes inadequate or otherwise undesirable uptake. 7) For local conditions achieved using a suitable suppository formulation. 31 1. NO Nature of the active. Three principal factors that define formulation requirements: 1. 2. 3. The actives physical state under ambient conditions. The solubility characteristics of the active. The physicochemical activity with regards to potential excipients. 32 1. Physical State. NO The active can be either liquid, pasty, or solid in nature. Bulk Density. the big difference in the density between the active and the base cause problem during filling and homogeneity of the suppositories. Solubility: 33 B. Choice of the Base NO 1) They enable a selected active to be fabricated in a manner appropriate to both its physicochemical characteristics and the requirements of the manufacturer. 2) They are used to control delivery of the medication at its site of absorption. 3) For this reason the bases manufacturers offer a wide selection of raw materials in order to anticipate a correspondingly broad range of product needs. 34 Selection criteria of the baseNO A. Nature of the active ingredient. B. Manufacturing capabilities. C. Desired release characteristics. D. Chemical no-reactivity with the active. E. Nontoxic and nonirritant, and stable when formulated. 35 Selection of the appropriate Base NO I. During Production: Slight contraction upon cooling in order to facilitate removal from the mold. Inertness no chemical interaction between the base and the active ingredients. Solidification (should be optimum). Viscosity: to be viscose to prevent sedimentation during filling until cooling. 36 II. During Storage: NO Impurity. Bacterial/Fungal contamination should be minimized by selecting a non-nutritive base with minimal water content. Softening. The suppositories should be formulated so that it does not soften or melt under transportation and storage conditions. Stability. The selected materials can not oxidize when exposed to air, humidity, Or light. 37 III. During Use: NO Release. Choice of the proper base provides optimal delivery of the dispersed active into the target site. Tolerance. The finished suppository should have minimal toxicity and not be irritating to sensitive rectal mucosal tissue. 38 Suppository Basis Suppository bases plays an important role in the release of the drug they hold and therefore in the availability of the drug for absorption for systemic effects or for local action. And because of the possibility of chemical and or physical interactions between the drug and the base, which could affect the stability and or bioavailability of the drug, the absence of any drug interaction between the two agents should be ascertained before formulation 39 Suppository Bases From the point of view of composition, suppository bases can be described as falling into one of the three categories: 1. Naturally derived. 2. Synthetic. 3. Semisynthetic. 40 I. Natural Bases All naturally derived suppository bases used today are produces from Cocoa Butter, it’s a fatty material composed of a mixture of C16 to C18 saturated and unsaturated fatty acid triglycerides obtained from the roasted seed of Theobroma cacao. Fatty bases are the most frequently used suppository bases. These bases melt at body temperature. 41 In addition to cocoa butter, other natural materials such as: Gelatin, Agar, and Waxes have been employed as suppository bases. Their uses are limited and often relegated to special applications because special problems are encountered with their use. 42 Advantages: 1. It is readily liquefies on heating but sets rapidly when cooled down. 2. Melt at body temperature. 3. It is miscible with many ingredients. 4. It is bland, therefore no irritation occurs. 43 Disadvantages: Despite Theobroma oil been used for over 200 years, however it is not without limitations. And those limitations are: 1. Theobroma oil is polymorphic i.e. when it is heated and cooled it solidifies in a different crystalline form. 2. Theobroma oil shrinks slightly on cooling, adherence to the walls of suppository mold. 3. The relatively low melting point makes it unsuitable for use in hot climates. 44 4. The melting point is reduced if the active ingredients are soluble in the base. 5. Theobroma oil deteriorates on storage and is prone to oxidation. 6. The quality of Theobroma oil may vary from batch to batch, and it can be expensive. For these reasons, the use of cocoa butter as a suppository base is becoming increasingly less attractive, particularly in the of the availability of more modern alternatives. 45 II. Synthetic & Semi-synthetic Bases Chemically they are usually derivatives of fatty acids that undergo chemical alteration (transesterification) to enhance their use for this application Such chemical reactions yield a range of products with controllable characteristics making them suitable to be used as suppository bases. 46 For example: Hydrogenation is typically carried out to improve stability (enhance stability to oxidation and to increase chemical inertness). Hydrogenating suitable vegetable oils such as (Palm kernel oil and cottonseed oil) are used. Melting point ranges can be more precisely tailored to specific requirements. Examples of semisynthetic suppository bases: Novata, Suppocire, Wecobee and Witepsol types. 47 Advantages: The base is more flexible and not brittle. More stable on oxidation and hydrolysis. Less irritant compare with other bases. 48 Disadvantages 1. The viscosity of the synthetic fats, when 2. 3. 4. 5. melted, is lower than that of Theobroma oil. this may lead to. Sedimentation risk of the active ingredients during the preparation process. Lack of uniformity of the active ingredients. These bases become very brittle if cooled too rapidly, so should not be refrigerated during the preparation period. There is more than one grade of synthetic fatty basis. 49 Water soluble & water miscible bases 1. Glycerol-gelatin bases: These bases is a mixture of glycerol and water, which is stiffened with gelatin. Mass of Glycerol suppositories BP has 14% w/w gelatin and 70% w/w glycerol. In hot climates gelatin content can be increased to 18%. Gelatin is purified protein produces by the hydrolysis of the caliginous tissue of animals such as skins and bones. There is two types of gelatin: Type A and Type B. 50 This type of base is less frequently used than the fatty bases for a variety of reasons. Disadvantages of this type of bases: 1. Glycerol-gelatin base have a physiological effect. This is useful if a laxative effect is required but otherwise is undesirable. 2. Difficulties in preparation and handling. 3. The dissolution time depends on the content and quality of the gelatin and also the age of the suppository. 51 4. They are hygroscopic and therefore require careful storage and may cause rectal irritation. 5. Possibility of microbial contamination is more likely than with the fatty bases. 52 2. Macrogols These are different types of polyethylene glycols which are blended together to produce suppository bases which vary in: Melting point. Dissolution rates. Physicochemical characteristics. High polymer produce preparation which release the drug slowly (they are brittle). A combination of different polymer release the drug more readily can be prepared by mixing high polymers with medium and low polymers. (Less brittle) 53 Drug is release as the base dissolves in the rectal contents. Advantages: 1. 2. 3. 4. 5. They have no physiological effect, e.g. do not produce a laxative effect. They are not prone to microbial contamination. Some polymers have a high melting point. They have a high water-absorbing capacity. In solution, viscosity is high, which means there is less likelihood of leakage from body. 54 Disadvantages: 1. They are hygroscopic which means they must be carefully stored. 2. They are incompatible with several drugs and materials, e.g. bnzocaine, penicillin and plastic. 3. They become brittle if cooled too quickly and also may become brittle on storage. 4. Crystal growth occurs with some active ingredients. 55 Hydrogels Currently, an alternative vehicle for rectal delivery is being actively investigated. Hydrogels are among them, and it defined as macromolecular networks that swell, but do not dissolve, in water. The swelling of hydrogels, i.e., the absorption of water, is a consequence of the presence of hydrophilic functional groups attached to the polymeric network. The aqueous insolubility of hydrogels results from the cross-links between adjacent macromolecules. 56 The use of hydrogel matrix for drug delivery involves the dispersal of the drug in the matrix, followed by drying of the system and simultaneous immobilization of the drug. When the hydrogel delivery system is placed in an aqueous environment, e.g., the rectum, the hydrogel swells, and drug is then able to diffuse out of the macromolecular network. 57 Selection Criteria Melting Temperature Range. Iodine Value. Hydroxyl Index. 58 Suppository Production Methods 1. Melting. 2. Compression. 3. Injection. Injection molding production process involving PEGs as the base might proceed as follows: The PEGs are first melted and mixed in a vessel equipped with a stirrer and a heating device at about 60°C to 80°C . 59 Additional viscosity -plasticity –adjusting ingredient, auxiliary ingredients, and actives are added while stirring. Once blending is complete, the melt is extruded into precision-machined multi-cavity molds. Rapid solidification of the melt is followed by ejection of the molded units from the mold cavities. Very fast, Precise metering and molding. Range of shapes and sizes 60 In-Process Control Proper monitoring of product physical characteristics is necessary to ensure that the production process remains under control throughout filling. Visual Examination: Examination of physical defects of finished suppositories provides valuable information for process monitoring. Color variations, chips, cracks, depressions, and surface irregularities are evidence of problems that require attention. 61 1) Weight checks: periodic weighing of individual suppositories will reveal problem in the filling operation. (in each filling needle). 2) Leak Test 3) The quality of the seal is a parameter that can affect the stability of the product (vacuum test). 62 Quality Control A. Physical Analysis: 1. Visual Evaluation, surface appearance and color can be verified visually to assess: Absence of fissuring, pitting, fat blooming, exudation, and migration of the active ingredients. The last test accomplished by taking a longitudinal section of the suppository to verify the homogeneity of the active ingredients within the mass. 63 2. Melting Point. The melting point is a critical factor in the determination of the release rate of the active ingredients from the suppository. The melting point of the finished suppository should generally; not be greater than 37°C. 64 3. Liquefaction Time. This is an important element indicates the physical behavior of a suppository subjected to its maximum functional temperature 37°C. It measures the time necessary for a suppository to liquefy under pressures similar to those found in the rectum (30g) in the presence of water at body temperature. A rule of thumb is that liquefaction time should be no longer than 30 minutes. 65 4. Mechanical strength: This is the determination of the mechanical force necessary to break a suppository, and it indicates whether a suppository is brittle or elastic. The mechanical strength should in no case be less than 1.8 to 2 kg. 66 5. Melting and Solidification: The most commonly used methods are: Open capillary tube. U-Tube. Drop Point. These methods are similar in principle, differ somewhat in their methodologies. all require the introduction of a sample into a specified place in the apparatus, after which heat is applied in a controlled manner. Means are provided for the determination of the point at which the test material undergoes a change in physical state, (i.e., melts). 67 1. 2. 3. 4. 5. 6. 7. 8. 9. An ideal suppository base must: Melt at or just below body temperature or dissolve in body temperature. Solidify quickly after melting. Be miscible with many ingredients. Be bland, i.e. non-toxic and non-irritant. Be stable on storage. Be resistant to handling. Be stable to heating above its melting point. Release the active ingredients readily. Be easily molded and removed from the mold. 68 Release Process of drug from suspension suppository Suppository Melting and Spreading Sedimentation Wetting Dissolution 69 Factors affecting drug release process Temperature Contact area Release medium Movements Membranes 70 Formulation of suppositories Different types – rectal, vaginal, and urethral. Different shapes and sizes Usually between 1-4g Drug content varies widely – 0.1% to 40% Vehicle (base) in which drug is incorporated – sometimes contain other additives 71 Mould Calibration The capacity of the mould is determined by filling the mould by the chosen base. The total weight of the perfect product is taken and a mean weight calculated. This value is the calibration value of the mould for the particular base. 72 7. 8. 9. 10. 11. 12. 13. 14. 15. Melt 2/3 of the base and then remove form the heat, the residual heat will melt the rest of the base. Reduce the particle size of the active ingredients. Weigh the correct amount of medicament and place on a glass tile. Add half of the molten base to the powdered drug and rub together with a spatula. Scrape this mixture off the tile, using the spatula and place back into the porcelain basin. Quickly pour into the mould, slightly overfilling each cavity. Leave the mould and its contents to cool for 5 min. Allow to cool for further 10-15 min. Unscrew the mould and remove the suppositories. 73 Packaging and Storage Plastic (PVC) or aluminium foil pack Protection against moisture and oxygen Store in cool place High humidity – absorb moisture – spongy Low humidity – lose moisture - brittle 74