Chronic Renal Failure in Children
advertisement

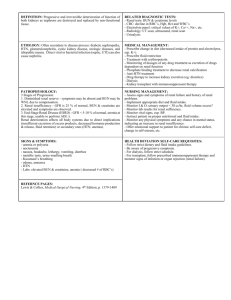
Chronic Renal Failure in Children Maria Ferris, MD August 2001 Chronic Renal Failure in Children • CRF is a stage of renal dysfunction with GFR ~ 75 ml/min/1.73 m2 to severe renal failure with GFR ~ 10 ml/min/1.73 m2 (ESRD) Epidemiology • The incidence of ESRD is about 1-3 children/million total population • Incidence in children 0-19 years of age adjusted for age, race and sex averages 10-12/million adjusted population • When examined by race, Asian, Pacific islanders and Native Americans have lower rates, and African Americans have higher rates of ESRD in 15-19 years of age Epidemiology • Current US data are thought to underestimate the true childhood incidence rate by about 10-13% because of under reporting • Over the past decade, ESRD in US children has remained constant between 0-4 years but has increased by 50% between the ages of 5-19 years Estimating Progression of Renal Disease • The relation of log serum creatinine (1/SCr) versus time has been used • Creatinine clearance can overestimate GFR for two reasons – Tubular secretion of Cr increases in a variable but significant manner – GI CrCl becomes a larger percentage of total clearance • In patients with CRI, both Cr secretion & excretion are affected by protein intake and HTN Rx Diet and CRI • Dietary protein intake is a potent modulator of GFR • It has been proposed that limiting protein intake may slow progression • Any decrease in GFR results in an in the transcapillary hydraulic pressure in snGFR within the remaining nephrons Diet and CRI • It has been proposed that glomerular hyperfiltration (although initially an adaptive response to maintain GFR) is responsible for the progression of glomerulosclerosis & renal function Dietary Protein and Renal Function • GFR is affected by both acute and sustained changes in protein intake • In rats, protein diets with partial renal ablation accelerates glomerulosclerosis (not in dogs or apes) • Because of growth, studies in children prescribe protein intake no lower than the RDA (0.6-0.8 g/kg/day up to 40 g/day) Dietary Protein and Renal Function • Adults and children with CRF maintain nutrition status when given very low protein diet supplemented with ketoacids • In adults, the MDRD study was unable to demonstrate that either low protein diets or very low protein diets supplemented with ketoacids were effective at slowing the rate of progression of disease Limiting Phosphorus Intake • Phosphorus intake is closely linked to protein intake • It is not clear whether there is a direct role of dietary phosphorus in accelerating progression of disease Limiting Lipid Intake • Hyperlipidemia is associated with development of glomerulosclerosis in animal models • Lipid lowering strategies appear to decrease renal injury in rats, but results are equivocal in humans • Mechanisms include uptake of Low Density lipoproteins by PMN’s within the glomerulus & production of renal thromboxanes in lipidemia Limiting Lipid Intake • Polyunsaturated fatty acids are precursors for prostacyclin (PGI2)and thromboxanes (TxA2): – PGI2 : a potent vasodilator and platelet antagonist – TxA2: a vasoconstrictor with platelet agonist properties • The specific inhibition (TxA2) preserves renal Fxn & histologic damage in rats Limiting Lipid Intake • PGI synthesis w/PO linoleic acid urinary PGI excretion & renal Fxn • Dietary fish oil w/ -3 fatty acids slows the rate of progression in adults with IgA GN Limiting HTN & Proteinuria • Proteinuria affects renal Fxn in glomerular diseases and DM • The mechanism of anti-HTN Rx is not clear: may be related to the improvement of systemic BP or the intrarenal BP • Even when proteinuria is not a clinical problem, BP control is effective in slowing the progression of renal failure Adaptation to Loss of Renal Mass: Glomerulal • As renal mass , the residual renal tissue undergoes physiologic and morphologic change that includes intraglomerular capillary HTN, glomerular hyperfiltration & hypertrophy. • Although the initial effects of this adaptation is to restore renal Fxn, it may be ultimately causing long-term damage to the kidney. Adaptation to Loss of Renal Mass: Na • Na homeostasis is well maintained throughout the course of CRI • Under normal circumstances, healthy children can adapt to Na intake of < 1 to >500 mEq/day (25,000 mEq Na filtered/day or 180 L/day x 140 mEq Na/L) • More than 99% of the filtered Na is reabsorbed, < 1% is excreted Adaptation to Loss of Renal Mass: Na • Each glomerular reabsorbs less and excretes more Na • Although patients with CRI retain their ability to alter Na balance w/change in Na intake, they can’t adapt rapidly (in acute Na load is excreted less efficiently, so ECF volume ; in acute in Na intake to ECF volume contraction) Adaptation to Loss of Renal Mass: Na • In CRI, Na conservation is less efficient • In obstructive uropathy and GFR, Na is not retained effectively ECF contraction • Na losses then contribute to poor growth – Can be treated with Na supplementation Adaptation to of Renal Mass: K • Normally, 90% of daily K intake is excreted in urine (the balance in stool) • K homeostasis is usually maintained until GFR is < 10% of normal by a combination of colonic and distal tubular K secretion • In CRF, aldo excretion stimulates Na-K exchange in the distal tubule and colon Adaptation to of Renal Mass: K • Spironolactone or ACE inhibitor (Inhibite aldo) should be used with caution K • Some patients with CRI have hyperreninemia (unknown cause), hypoaldosteronism & are vulnerable to K Hyperkalemia • A common cause of hyperkalemia and CRI is dietary or the use of K-salt substitutes • Seen in CRI with the development of ECF volume depletion, acidosis or oliguria • May occur due to transient pseudohypoaldo with ACE inhibitors or with obstructive nephropathy • Children with renal salt wasting are more prone to hyperkalemia, particularly when salt supplements are omitted Hypokalemia • Uncommon in children with CRI • Children receiving diuretic therapy or those with RTA sometimes develop K requiring K supplements • As renal function declines, a tendency for hypokalemia decreases and K supplements may be discontinued Hydrogen+/ Bicarbonate • Maintenance of normal acid-base balance is due to reabsorption of filtered bicarbonate by proximal tubule and secretion of acid equivalence by the distal tubule • Net acid production is from bone formation & catabolism of sulfa-containing amino a. • Metabolic acidosis is common in patients with CRI when GFR to < 50 ml/min/1.73 m2 Hydrogen+/ Bicarbonate • Net acid excretion varies in adults from 1-2 mEq/kg/day & in children 2-3 mEq/kg/day (bone & dietary net acid input) • With bone reabsorption, Ca and hydroxyl ions are released; hydroxyl ions accept hydrogen ions • In acute acidosis, bone buffering occurs but in chronic acidosis is less certain Hydrogen+/ Bicarbonate • Total ammonia synthesis as GFR & the ability to excrete acid • In humans, the threshold for bicarbonate reabsorption is and bicarbonate wasting urine may be alkaline despite acidosis • Renal bicarbonate excretion is in hyperparathyroid states, with ECF volume expansion and Fanconi syndrome Alkalosis • When ECF volume is maintained, renal bicarbonate excretion is large and metabolic alkalosis from alkali treatment is unusual. • Only with very low GFR does alkali therapy exceed this capacity and result in metabolic alkalosis • ECF volume (diuretics or renal salt wasting) usually is associated with NaCl depletion. • If alkali is given without giving chloride then contraction metabolic alkalosis results Water • Most patients maintain normal water balance until late in the course of CRI • Concentration ability is limited if the patient has dysplasia or medullary tissue disorder • Total osmolar clearance is unchanged and free water clearance as GFR • As GFR urine becomes isotonic or hypotonic Water • Patients with high salt & protein intake and polyuria will urine volume if they salt and protein intake • Children with obstructive uropathy need to be encouraged to drink water ad lib ast hey do not concentrate their urine Calcium • In children with CRI, both dietary Ca uptake and urinary Ca excretion are • GI Ca absorption is as a result of circulating 1,25 hydroxy Vitamin D levels • PTH increases both bone Ca release and renal Ca reabsorption Calcium • In severe renal failure, total urinary Ca excretion remains low and FeCa • When Vitamin D is given to prevent renal osteodystrophy, hypercalcemia, hypercalciuria and decreased GFR may occur Phosphorus • Serum phosphorus levels are maintained WNL until GFR decreases to about 25% of normal • If phosphorus intake remains high, the release of phosphate is in patients with CRI • The FePO4 • It is proposed that a decrease in renal phosphate excretion secretion of PTH Phosphorus • PTH levels cause an increase in fractional excretion of phosphorus • The FePO4 does not depend on hyperpara, as it can occur in parathyroidectomized animals in which PTH is absent or at base-line level Metabolic Toxins • High Urea may be toxic • If SUN is 100 = weakness, malaise, lethargy & platelet dysfunction • Even if SUN is 190 few adtl/ uremic symptoms occur not a major metabolic toxin • ?PTH, guanidines, methylamines, phenols & polyamines Metabolic Adaptation Anemia (Causes) • EPO by the peritubular interstitial cells within the inner cortex and outer medulla. • Fe • RBC Survival, bone marrow inhibition • Intestinal and later HD-related loss Anemia in Children • With GFR 20-35 ml/min/1.73m2 • Hgb in pre-pubertal children is 2g/dL lower than adults • Rx with r-HuEPO (prior to ESRD) appetite but not Wt and Ht SDS. Side effects: Fe and HTN Growth and Development Malnutrition • Anorexia is a major c/o (? Taste sensation altered) • When diet <80% RDA = growth retardation • Catch up growth does not catch up to peers • Calorie use less efficient in CRF ? • Intakes > 100% RDA are not desirable Nitrogen Balance • N intake = loss (stool, urine, skin) normally • Children have a higher protein requirement than adults (greater lean body mass) & need to be in (+) N balance to support growth Nitrogen Balance • Uremia alone may increase protein catabolism and/or be associated with poor utilization of protein • With azotemia, PO protein should be progressively reduced to minimal levels in an attempt to keep the SUN <100 Nutrition • With CRF recommended diet is CHO’s 50, fat 35-40, and protein of high biologic value 5-10 gm/day ( protein intake to 0.6 gm/ kg/day, or to 0.3 gm/kg/day if combined with a.a. or k.a.) • The CHO consumption should be at the within four hours of protein ingestion, to prevent protein catabolism Statural Growth Failure • Malnutrition plays a major role in growth failure in infants but not in older children • In pre-ESRD pubertal children the growth spurt is delayed and has a smaller Pk Ht velocity, so mean Ht gain is 50% of normal • CRI children are less affected than ESRD Intellectual Development Neurologic and Cognitive Function • • • • In first 2 years brain vol. doubles to 80% final In CRI Performance IQ worse than verbal IQ Test scores improve after Txp EEG Changes w/ PTH which respond to parathyroidectomy • Psychosocial adjustments Care of a Child with CRI Setting • Diet records q. 2-6 months • Multidisciplinary care • Continued education and monitoring Care of a Child with CRI Measurements • Growth and GV • Triceps skin folds thiickness and mid-arm circumference difficult in infants • BUN/Cr >20 = vol/Protein, <10 malnutrition • Labs & Bone age • Developmental evaluations Care of a Child with CRI Caloric Intake • • • • Feeding strategies Supplements Feeding tube TPN Drugs/Medications Therapy for Growth Failure • • • • • Nutrion Fluid and electrolytes PTH EPO Psychological Rx Drugs/Medications Therapy for Growth Failure • Growth Hormone at 0.35 mg/Kg or 30 Units/m2 Drug Use in Children with Decreased Renal Function • Correction of doses by GFR • Drug interactions