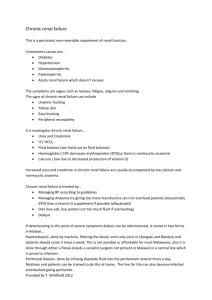
Renal
advertisement

MCC NURSING Diana Blum MSN • Play role in: • • • • Maintaining fluid balance Maintaining acid/base balance Producing erythropoiten Secreting renin • Renin angiotensin cycle • Activating vitamin D • Regulating ADH • Eliminating metabolic wastes Congenital: Polycystic Kidney Disease • Medical treatment • Supportive treatment is recommended to preserve kidney function, treat UTI, and control hypertension • Infections treated promptly with antibiotics • Dialysis, nephrectomy, and transplantation once end-stage renal disease develops • Inflammation of the renal pelvis • Acute pyelonephritis most often caused by ascending bacterial infection, but it may be blood borne • Chronic pyelonephritis often the result of reflux of urine from inadequate closure of the ureterovesical junction during voiding • Medical treatment • • • • Antibiotics, urinary tract antiseptics, analgesics, and antispasmodics Drink at least eight 8-ounce glasses of fluids daily Intravenous fluids may be ordered if nausea and vomiting Dietary salt and protein restriction for patient with chronic disease • Patho • Complications of UTI; tissue necrosis leads to scarring—wall off infection • Strept is usual cause s/s fever, flank pain, dysuria • Interventions • antibiotics • Patho • Spread by hematogenesis route from pulmonary disease • Usually bilateral s/s few, males more than females; dormant for years; pain in pelvis Interventions INH • Pathophysiology • Immunologic disease: inflammation of the capillary loops in the glomeruli • Signs and symptoms • Urine becomes tea colored as output decreases • Peripheral and periorbital edema • As glomerular filtration decreases, mild to severe hypertension occurs and hypervolemia results • Medical diagnosis • Patient assessment and laboratory tests • Urinalysis, BUN, creatinine, and albumin • Renal ultrasound, renal biopsy, or both • Assessment • Signs and symptoms, recent infections, and changes in urine • Nursing Diagnosis • • • • Excess Fluid Volume Activity Intolerance Self-Care Deficit Anxiety • Patho • Rapid, causes damage to small structures that filter waste • s/s • Edema, blood in urine, abd pain, joint pain, htn, proteinuria Interventions corticosteroids, plasmaphoresis, watch for kidney failure • Patho • Due to repeated episodes of acute glomerulonephritis, hyperlipidemia, hypertensive nephrosclerosis and chronic tubulointerstitial injury • s/s • Progressive; acute nosebleed, stroke or seizure; malnourished, edema, diminished DTR, mucous membranes pale, gallop rhythm, distended neck veins • Interventions • Fluid and electrolyte imbalance (labs);emotional support; anxiety high; teaching client about treatment plan and need for follow up. • Patho • Cluster of findings: Increase protein, decrease albumin, edema, high serum cholesterol; serious damage to the glomerular capillary membrane; occurs with intrinsic renal disease; disorder of childhood; caused by DM, lupus, Multiple myeloma • s/s • Edema: periorbital, lower extremity, abdomen (ascites); patients have irritability, HA and malaise • Interventions- treat underlying cause • Early stages: similar to acute glomerulonephritis • Late stages: Chronic Renal Failure • Patho: • Malignant: associated with malignant hypertension • Young adults, men>women; progress is rapid • Benign: associated with atherosclerosis and hypertension • Older adults • s/s • Rare early in the disease; renal insufficiency occurs late in the disease • Interventions • Aggressive antihypertensives; ACE inhibitors • Patho • 3-16% of arteries become blocked and shrinkage of the kidney occurs leading to HTN and reduced blood flow causing release of excess renin and reinitiates the cycle. • s/s • HTN above 180/100 and resistent to 2 or more meds • Interventions • Lipid management, Smoking cessation, antiplatelet therapy, weight reduction, ACE-I, • Endovascular therapy (stents) • Monitor VS, monitor insertion site, etc. • Patho • Characterized by a period of hyperfiltrationand increased GFR to proteinuria and decreased GFR with increase in creatinine • s/s • Asymptomatic, found on routine lab screen with microalbuminuria, BP starts increasing, neurogenic bladder, infection, • Interventions • ACE-I/ARB, monitor BP, monitor UO, monitor Lab values, dialysis, transplant, monitor Wt, Monitor A1C, Sodium Restriction • Early symptoms: • anemia, weakness, and weight loss; painless, gross hematuria classic sign, but usually occurs in the advanced stage. A dull ache in the flank area also is a late symptom • Medical diagnosis • Excretory urography, IVP, retrograde pyelography, ultrasound, arteriography, computed tomography, magnetic resonance imaging, and renal biopsy • Medical treatment • Radical nephrectomy • In general, renal tumors are not responsive to radiation or chemotherapy; radiation is sometimes used as a palliative measure for inoperable cancer • Biotherapy with alpha-interferon and interleukin-2 for metastatic disease • Nursing Diagnoses • • • • • • • Acute Pain Risk for Deficient Fluid Volume Ineffective Breathing Pattern Risk for Injury Risk for Infection Ineffective Coping Deficient Knowledge • Causes • Prerenal failure: decreased blood flow to glomeruli • Intrarenal failure: nephrotoxic agents, kidney infections, occlusion of intrarenal arteries, hypertension, diabetes mellitus, or direct trauma to the kidney • Postrenal failure: obstructions beyond the kidneys that cause urine to back up • Onset stage • Short (1-3 days); increasing BUN and serum creatinine with normal to decreased urine output • Oliguric stage • • • • The urine output decreases to 400 mL/day or less Serum values for BUN, creatinine, potassium, and phosphorus increase Serum calcium and bicarbonate decrease Follows onset stage and continues for up to 14 days • Diuretic stage • Urine output exceeds 400 mL/day; may rise above 4 L/day • Kidneys excrete BUN, creatinine, potassium, and phosphorus and retain calcium and bicarbonate • Recovery stage • As renal tissue recovers, serum electrolytes, BUN, and creatinine return to normal • This stage lasts 1 to 12 months • Medical treatment • Fluid and dietary restrictions, restoration of electrolyte balance, and dialysis • Drug therapy • Diet • Fluids • Hemodialysis and peritoneal dialysis • Continuous renal replacement therapy • ARF: • Hypovolemia; hypotension; reduced cardiac output; obstruction of the kidney; obstruction of the renal arteries or veins • CRF: • DM; hypertension;polycystic kidney disease, vascular disorders, infections, meds, environmental agents (lead, mercury, chromium) • Progressive nephron destruction of both kidneys • Creatinine clearance: important measure of renal function • <15 mL/min, dialysis or transplantation necessary • Uremia: when kidneys unable to maintain fluid and electrolyte or acid-base balance • Also called end-stage renal disease • Causes: hypertension, diabetes mellitus, and atherosclerosis • • • • • • • • • Azotemia Hyperkalemia Hypocalcemia Metabolic acidosis Fluid balance (hypernatremia and hypervolemia) Insulin resistance Anemia Suppressed immunologic function Cardiovascular system (CHF and dysrhythmias) • Neurologic system (mental status changes) • Integumentary system (accumulation of waste products) • GI system (irritation, nausea, vomiting, a metallic taste in the mouth, and bleeding) • Musculoskeletal system (renal osteodystrophy) • Reproductive system (sex hormones decline and libido is diminished) • Endocrine function (hyperparathyroidism) • Emotional and psychological effects • IV glucose and insulin, calcium carbonate, calcium acetate, or sodium polystyrene sulfonate to treat hyperkalemia • Calcium, active vitamin D, and phosphate binders to treat hypocalcemia • Fluid restriction and diuretics to treat hypervolemia • Diuretics, beta blockers, calcium channel blockers, and ACE inhibitors for hypertension • Iron supplements, folic acid, and synthetic erythropoietin to treat anemia • Hypertonic glucose to treat disequilibrium syndrome • High-carbohydrate, low-protein diet to prevent excess urea Hemodialysis Blood is removed and circulated through an “artificial kidney” to remove excess fluid, electrolytes, wastes Dialyzed blood then returned to the patient Requires vascular access By catheter, cannula, graft, or fistula Subclavian or femoral catheters for temporary access for dialysis during acute renal failure while a graft or fistula matures (dilates and toughens) or for patients on peritoneal dialysis who need immediate access for hemodialysis • Arteriovenous fistula: is formed by creating a surgical incision and anastomosing a vein and an artery usually in the forearm • Arteriovenous graft: a Gortex tube is surgically implanted into to the forearm with the vein and artery • Hemodialysis (during and post care) • • • • • • • • Aseptic technique Do not cannulate new sites Watch for pseudoaneurysms Do not obtain blood pressure/ iv access on AV fistula site Teach client how to develop fistula thru exercise like squeezing a ball Monitor weight and vitals Monitor meds and diet before and after Monitor labs before • Peritoneal dialysis • Uses the patient’s own peritoneum as a semipermeable dialyzing membrane • Fluid instilled into peritoneal cavity • Waste products drawn into the fluid, which is then drained from the peritoneal cavity • May be temporary or permanent • Temporary: catheter inserted into the peritoneal cavity through the abdominal wall • Long-term: catheter is implanted into the peritoneal cavity • Assessment • • • • Frequent monitoring for changes important Fluid balance evaluated closely Accurate intake and output records Signs and symptoms of fluid volume excess that can lead to cardiac failure: increasing edema, dyspnea, tachycardia, bounding pulse, rising blood pressure • Signs and symptoms of electrolyte imbalances • Appetite, usual daily intake, weight gain or loss pattern, and prescribed diet • Kidney donation • • • • Healthy kidney from live donor (a relative) or cadaver Tissues must match or recipient will reject new kidney Matching based on ABO blood groups and human leukocyte antigens Crossmatching reveals any cytotoxic preformed antibodies—would certainly result in organ rejection • Kidney donors must be at least 18 years of age, free of systemic disease or infection, have no history of cancer or renal disease, have normal renal function, and be without major medical problems • Preoperative nursing care • Patient must be prepared mentally and physically • Recipient and live donor have complete diagnostic workups to rule out other medical problems and evaluate function of the urinary tract • Recipient given medications to bring blood pressure within normal limits • Immunosuppressants: to control the body’s response to foreign tissue • Postoperative nursing care • Assessment • Fluid intake, urine output, weight changes, and vital signs • Interventions • Impaired Urinary Elimination • Deficient Fluid Volume • Risk for Infection • Ineffective Management of Therapeutic Regimen • Anxiety • • • • Physical care of the donor similar to that for a nephrectomy Nephrectomy may be conventional or laparoscopic Pain worse with conventional approach; provide good pain control Conventional approach: patient hospitalized 4 to 7 days and return to work in 6 to 8 weeks • Laparoscopic approach: donor hospitalized 2 to 4 days and can return to work in 4 to 6 weeks • Donor usually feels good about the experience • If kidney fails, donor may be disappointed; be sensitive