3.10 CD-MH
advertisement
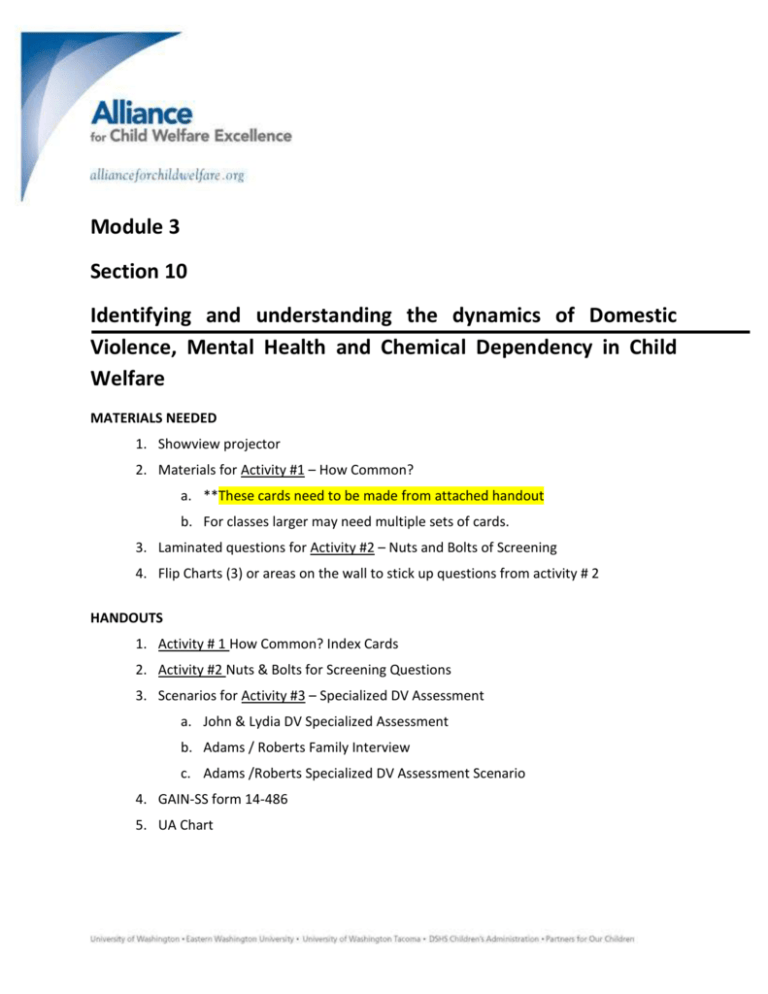
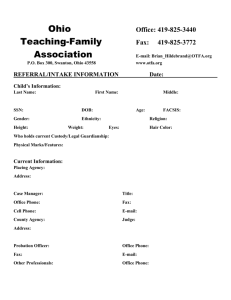
Module 3 Section 10 Identifying and understanding the dynamics of Domestic Violence, Mental Health and Chemical Dependency in Child Welfare MATERIALS NEEDED 1. Showview projector 2. Materials for Activity #1 – How Common? a. **These cards need to be made from attached handout b. For classes larger may need multiple sets of cards. 3. Laminated questions for Activity #2 – Nuts and Bolts of Screening 4. Flip Charts (3) or areas on the wall to stick up questions from activity # 2 HANDOUTS 1. Activity # 1 How Common? Index Cards 2. Activity #2 Nuts & Bolts for Screening Questions 3. Scenarios for Activity #3 – Specialized DV Assessment a. John & Lydia DV Specialized Assessment b. Adams / Roberts Family Interview c. Adams /Roberts Specialized DV Assessment Scenario 4. GAIN-SS form 14-486 5. UA Chart | 1 of 17 APPROXIMATE FLOW Time Activity/Topic 9:00 – 9:30 The context for understanding DV, MH and CD as a Child Welfare Professional 9:30 – 11:30 (incl. one 15 min break) Domestic Violence 11:30 – 12:00 Screening – GAIN SS and other screening approaches 1:00 – 2:00 Specific issues with Chemically Dependent Clients in Child Welfare 2:00 – 3:30 (incl. one 15 min break) Specific issues with Mentally Ill clients in Child Welfare 3:30 – 4:00 Applied practice and closure 6 hrs Total Time ANTICIPATORY SET This session is an INTRODUCTION to three concerns that are very frequently occurring in families involved in the child welfare system – adult/caregiver mental health problems, adult/caregiver chemical dependency, and domestic violence (intimate partner violence). The day is meant to orient participants as to how we understand these issues in child welfare work – gaining very basic tools and skills to perform rudimentary assessments, connect clients with local experts, and – most importantly – help gain an understanding of how the concern may be impacting the family’s ability to keep their child(ren) safe. Additional training as to each of these subjects will be provided during your first year on the job. PROCEDURES AND TEACHING POINTS The context for understanding DV, CD and MH issues as a Child Welfare Professional Activity #1 – How Common? Handout How Common index cards | 2 of 17 Divide class into small groups (ie 4 to a group) Handout the How Common? Index cards Ask workers to guess what percentage of people experience identified situation, and then order them based on greatest to least. Facilitate a large class debrief on how the class ordered, which one did most groups identify as highest etc. Provide the actual percentage from the How Common? Answer sheet. Variation - provide workers with the actual percentages, and have them try to match these to the statements. Trainer’s Notes: Note that two of the items reference “Serious Mental Illness”. This is a widely used distinction to differentiate people who are experiencing symptoms from a mental health problem that are causing significant disturbance in at least one life domain (family, work, health and hygiene, etc) from those who meet the diagnostic criteria for one or more mental illnesses but are able to function at a level where their major life domains are not disabled. Since about ¼ of the adult population qualifies under the diagnostic criteria for at least one mental illness at any given time, it’s an important distinction. It is additionally important to note that the distinction is entirely based on functioning and has nothing to do with what diagnosis the person has – so someone with an anxiety disorder might be considered to have SMI, or someone with Bi-Polar disorder may not be considered to have SMI. It’s all about current functioning and not about the label – this is a point that will be echoed later in the training. Many of the statistics speak to how commonly these problems co-occur. This is a theme in child welfare work and something that will be addressed today. These issues are shockingly common in families in the United States, and often co-occur Most cases with ongoing (FVS/CFWS) involvement will have at least one of these risk factors present. Many families served by our system struggle with most of these issues, along with a host of other barriers. Not all families with caregivers facing c/d, mh, or d/v have kids who are unsafe. o Our job is to identify whether kids are unsafe or not, and what role these issues may play in preventing a caretaker from adequately performing everyday life tasks | 3 of 17 Today we will address: o Identifying these concerns in the families we work with o Teasing out the relationship between these issues and child safety within each individual family o Some specifics regarding C/D, MH, and DV, that are particularly important to child welfare work o Understanding our relationship with community experts - how they help us (and the family) and how we help them (and the family). EXAMPLES OF HOW THESE ISSUES PLAY OUT IN OUR SYSTEM Trainer’s Notes: The questions in these slides aren’t meant to be answered – there is not enough information to do so. They’re meant to illustrate how child welfare workers have to understand the intersection between these concerns and safe parenting. Summary of the learning from the above slides: Identifying these issues is important –we screen for them on all cases regardless of the concern on the intake (parent/caregiver functioning apart from the parenting role is one of the questions in the safety assessment so these concerns must be ruled in/out) HOWEVER, identifying these issues in and of themselves doesn’t tell us if the kids are safe Professional assessments of these issues and/or compliance with treatment for them ARE NOT proxies for safety assessment. Domestic Violence Slide 10 – Why it’s confusing | 4 of 17 Victim Advocacy Programs Victim Defendant Classic Victim People who are SURVIVING People who Legal Definition Legal System Other Systems GOT HIT People who HIT a family or HH member People who need help & resources, but are not being battered by a family or HH member People who are Classic Perpetrator BATTERING System Manipulator Batterer Intervention Programs WHY IT’S CONFUSING **Need a bit more for talking points here Trainer’s Notes: As you click through this slide, each layer adds to the initial picture. It’s a nice slide to try to demonstrate how everyone we initially identify as possibly experiencing DV is not impacted in the same way, AND, everyone who needs our support, advocacy and intervention are not captured by simple measures like “who got hit?” and “what is the charge?” It feels like this… Victim Defendant They all need help and resources Classic tailored Victimto their situation and circumstances SURVIVING SURVIVING and for the people involved in It feels the relationship, like this and for their friends and families… HIT HIT ? ? GOT GOT HIT HIT BATTERING Classic Perpetrator BATTERING System Manipulator DV IS A COMPLEX PROBLEM WITH NO SINGLE SOLUTION. EVERYONE HAS A ROLE TO PLAY IN ENDING ABUSE AND IN HELPING PEOPLE LEARN HEALTHY RELATIONSHIP SKILLS. By Mette Earlywine/WSCADV with thanks to the NW Network We’ll explore screening and assessment today so that we learn how to sort all this out Screening and Identification Activity: The Nuts and Bolts of Screening When DV is occurring we want to know as soon as possible | 5 of 17 Required to screen for DV with every family and again “periodically” as a case progresses We want to screen in a way that does not decrease anyone’s safety How might we figure out that DV is occuring, beyond talking to the caregivers or others about the family? Documents! – while we won’t spend much time addressing these, you may find this information documented in ACES, in the criminal history or (even more reliably) through requesting individual criminal incident reports), within CA records or even by asking local LE about whether law enforcement has gone to the address and why We are going to be gaining lots of information about DV from individual interviews with the family and collaterals. How do we approach these interviews so that the safety of everyone is protected? Solicit ideas based on their readings and make sure to highlight the following: o Present screening as routine, required o ALWAYS interview people separately and privately – that includes outside the presence of children who may be “used” to gain information by an abuser o Explain more about the CA case process and how that information will be used o Help people understand the limits of confidentiality – it might be better if they didn’t disclose certain things (particularly when the abuser is also a parent, and will have a right to an unredacted copy of the file) o Don’t demand “proof” of the DV or that allegations are true – we gather information and do our own assessment about what may be happening, but questioning a victim’s statement is a great way to ensure they don’t disclose anything more o Don’t confront the perpetrator with victim’s/kids’ statements – use any documentation, phrase concerns based on disclosures generally, use the batterer’s own statements when possible o Don’t try to force a disclosure – accept and expect that many batterers will not be honest and forthright upon first contact. Identify discrepancies between the batterrer’s statement and other information you have, as you would when working with other issues, but avoid outright confrontation. Ratcheting up the pressure may have lots of negative consequences on the adult victim and child. | 6 of 17 Regarding DUTY TO WARN – in certain situations the legal requirement of confidentiality is superseded by a requirement to protect someone from serious harm. o When a client makes what you believe to be a credible threat to seriously harm or kill someone, you are required by law to make reasonable attempts to contact/warn that person about the imminent threat, and to alert law enforcement personnel. o RCW 71.05.120 (2) Activity #2 – The nuts and bolts of screening Handout Nuts & Bolts of Screening Questions Before the activity, label flip charts or areas around the room: Suspected victim, Suspected perpetrator, Collateral, youth/child Distribute the laminated questions randomly around to participants or stack them in a pile accessible to all. Ensure a way for the questions to stay fixed on the wall (tape, etc). In this exercise, you’ll have 3 (???) minutes to try to get all the questions up onto the wall sorted into the right category. Once the questions are sorted – have a different participant read questions in each category. Move questions as needed. Remember that, in all likelihood, you would ask both types of questions (perpetrator and victim) to each adult to get a full scope of behavior and understanding about that behavior in your assessment. Ask if there are other questions they can think of in each category. Screening is most effective when the person doing the interview feels comfortable with the questions and can put them into language that feels right for them. Accurately Identifying the Victim | 7 of 17 ACCURATELY IDENTIFYING THE VICTIM Who is afraid? is controlled? experiences repeated negative consequences? Who acts to protect the children when incidents happen? Who Who Page 30 Although DV can occur in any intimate relationship (hetero- or homo- sexual), and can be perpetrated by both men and women, the vast majority of DV is perpetrated by men against women in the context of heterosexual relationships. It’s important that in every case we accurately assess to determine who the victim is and who the perpetrator is. Getting this wrong has very, very serious consequences. It’s not uncommon that both partners have used violence, been arrested, reported that the other has been abusive, etc. How are we to sort this situation out? o By using these types of questions: Who is afraid? Who is controlled? Who is afraid? Who is controlled? Who experiences repeated negative consequences? Who acts to protect the children when incidents happen? o Help us focus on the why of the behavior (power and control, self defense, etc.) o The result of the behavior (being diminished, terrified, limited, isolated – or, being temporarily injured but maintaining the rest of your power and agency) Specialized DV Assessment | 8 of 17 SPECIALIZED DV ASSESSMENT Guides what information to gather (not a form or tool in FamLink) Informs conclusions about the impact of DV on the family Critical in determining if DV makes a child unsafe Documented in a case note specifically presenting information and conclusions Summarized on p. 34 Section 4, p. 33 - 53 Required by policy: a. Screen every family for DV b. Identify victim and perpetrator c. Specialized DV ASSESSMENT d. planning and engagement tailored to the specific safety threats and dynamics in the family SPECIALIZED DV ASSESSMENT helps us analyze what is going on, - ultimately, helps us assess child safety Remember that with DV we actually do the assessment, we don’t send clients out to community professionals Field Manual Review Workers were required to review the Social Worker’s Practice Guide to Domestic Violence as part of their field work. Facilitate a review of their work by asking the following questions: Are there distinguishing characteristics of domestic violence victims’ parenting approach, compared to the general population? Look for the following: • Unlike DV victims, DV perpetrators do differ from parents in general. DV perpetrators are much more likely than non-batterers to abuse their children physically (Straus,1983). • They are up to four times more likely than non-batterers to abuse their children sexually (McCloskey, Figueredo, & Koss, 1995). • DV perpetrators’ violent and controlling behavior can harm children by: | 9 of 17 Physically harming the children Endangering the children through neglect Psychologically terrorizing the children Coercing the children to participate in the abuse of their non-offending parent or other adult caretakers Preventing or undermining adult DV victims’ care of the children Undermining the ability of CA and community agencies to intervene and protect the children • DV perpetrators may also impact children negatively by: Creating role models that perpetuate violence Undermining DV victims’ parental authority Retaliating against DV victims for efforts to protect children Sowing divisions within their families Using children as weapons against DV victims o • (Bancroft & Silverman, 2002) DV perpetrators exhibit a broad range of parenting capacities: They may range from neglectful to rigid and/or authoritarian parents. Some may see their children and partners as extensions of themselves or objects they own, as opposed to vulnerable, individuals who are deserving of care and dignity in their own right. Other perpetrators may desire to be good parents. This may afford opportunities for social workers to engage DV perpetrators in making positive changes. What DV related questions should a social worker be considering while working on a case: Look for the following: Is there DV in this case or not? If so, who is the DV perpetrator and who is the adult victim? Does the DV perpetrator’s abusive behavior toward the adult DV victim place children in present or impending danger? How does the DV perpetrator’s abusive behavior toward the adult victim impact the ability of the family to address issues of concern for the children? | 10 of 17 How can CA work with the family to minimize the DV perpetrator’s ability to control and abuse the perpetrator’s intimate partner and therefore the children? How can CA help increase the protective capacity of the DV victim to create safety for the victim and the children? Handout the following: John & Lydia DV Specialized Assessment Adam-Roberts Family Interview Information (for Review only) Adams Roberts Specialized DV Assessment Scenario Activity #3 – Specialized DV Assessment Break class into groups of 2-4 Workers are likely already with the Adams-Roberts family. o The Interview information was used as an activity in creating the Safety Assessment. o This summary will serve as a refresher on the dynamics of the family. Have workers review the Adams Roberts Specialized DV Assessment Scenario which provides new information on the case. Workers will compile all of from both summaries to write a new Specialized Assessment. o Use the John & Lydia DV Specialized Assessment as an example/guide. o Workers can bullet the information under each area. Debrief the experience of creating a specialized DV assessment. • • What do you do when you can’t get much information about what is actually going on, but you still have a concern that DV might be happening? Your best. A great source of help is the local victims advocates in your area who could help you think through the actual information you know, and why you may not be able to pin down other information. | 11 of 17 Field Manual Review • • Workers were required to identify the local DV advocate programs in their area. • Facilitate a group conversation about what resources were identified, and if any workers have utilized these resources. This is also something you’d want to run by your supervisor – showing them the Specialized DV assessment you created with what you had and with some consultation and seeing what their thoughts are. How do you “use” the Specialized DV assessment? It informs your assessment of child safety, and the approach you take with engagement, support, case planning, visitation planning if any, and monitoring compliance. You will do all of these things differently: o With an eye on everyone’s safety o With a focus on diminishing the perpetrator’s ability to exert power, control, and physical violence o While increasing the adult victim’s own connection to resources and supports, and connection to the children. When do you do the Specialized DV Assessment and how often? • You are required to do a Specialized DV Assessment when information supports a possible concern about DV. • It might happen right after intake, or a year into a CFWS case when an adult discloses abuse for the first time. • Once a Specialized DV Assessment is done, it should be updated “periodically” and whenever circumstances indicate there may have been a significant change. What if I think that the adult is in serious danger right now? How do I go about helping that person stay safe? • In the DV services world, this is called “safety planning.” o It’s a different approach than how we safety plan for children, in that it’s a private conversation with an adult about what threats exist, how she can minimize the possible impacts and/or plan for a safe escape or to safely exit the relationship. | 12 of 17 • We don’t monitor an adult’s safety plan for compliance, it’s a personal plan to prepare for and minimize the potential impact of violence toward them. • While we aren’t addressing safety planning with adult victims here, it will be addressed in future trainings. • For right now, one option is to ask the adult survivor to call their local advocacy agency, 800-562-6025, or the national hotline, 800-799-7233. o You can call with the survivor or they can call themselves. o You don’t need to monitor the conversation or the plan – in fact it’s best that you not document anything in the plan. o What you should ensure is that the victim knows why you are concerned, and that they’ve had some opportunity to plan with an expert in DV to ensure their own safety, as well as that of their children. Children should also be informed of the following: o Never intervene, o Where they are safe in the home o Where they should go if violence occurs to be safe. Children should know how to call 911 and what adult nearby can help if something happens. o Many families have a “code word” that the adult survivor uses to tell the kids that they should put their safety plan into action now. Screening – GAIN-SS and other screening approaches Screening for MH and CD Both state law and policy require that every adult we work with be screened for C/D and MH concerns RCW 71.05.027 requires all DSHS administrations to use the same screening tool for substance abuse, mental health, and co-occurring disorders – the GAIN-SS was selected to be this tool | 13 of 17 Required unless the client is currently engaged in MH or CD services, or it’s been completed in the last 6 months by someone in CA Follow the directions for referral – but may refer even if the GAIN-SS threshold isn’t met if there are other indicators of a problem The suicide question may require immediate action – either contacting local crisis line or MHP’s How else are you going to find out whether these issues may be occurring within a family? o Documentation within a variety of systems, o Collaterals, o Observation of behavior and environment, o child interviews, o ROI to healthcare provider, other Activity #4 - Gain SS Provide the GAIN-SS form to participants and give them a few minutes to review it and the instructions. Have participants practice asking each other the questions in groups of two or three. This should take 5-10 minutes. Debrief the exercise by asking: o What they like and don’t like about screening in this way. o How else the information might be obtained. o Whether it’s a better idea to screen alone with a client or with the other members of the family present. o What are the potential problems with simply handing the form to the client and having them fill it out (which is common practice in some offices). Specific issues in Chemical Dependency within the Child Welfare Population Chemical Dependency Assessments | 14 of 17 How are clients referred to a chemical dependency assessment in your office? How are you able to provide additional information to the agency doing the assessment? Why might this be a good idea? ADATSA Assessment Centers - http://www.dshs.wa.gov/pdf/dbhr/da/APPNDXG.pdf UA’s - what they tell us and what they can’t UA’s test for the body’s reaction to the drug – the metabolite. They don’t test for the drug it’s self UA’s come back “positive” if the urine has an amount of metabolite for a particular substance that’s equal to or greater than the cutoff threshold. The amount of metabolite is not particularly telling in most drugs – that is, higher numbers don’t necessarily indicate more frequent or heavier use. UA’s are only helpful if the specimen provided actually belongs to the person we’re testing – for that reason most UA’s are requested to be observed. For obvious reasons, clients aren’t going to be excited about this. Many products are available to “clean” urine and allow an individual to pass a drug test – most of these are also tested for If an individual’s urine is too diluted, the sample will indicate that rather than indicating “negative” | 15 of 17 Whenever there are questions about a UA’s results, or a client provides a story about why their UA is positive that you are not sure about, you are always able to call Sterling Labs and discuss this possibility. A significant amount of information about understanding results is available on the website. The document “Understanding the Drugs of Abuse” has great information including whether “passive” exposure might result in a positive and a significant amount of information about results for marijuana. CA UA site: http://ca.dshs.wa.gov/intranet/sw/sterling.asp Go to : http://www.sterlingreflabs.com/ca/default.asp and use CAstaff as the user name and UAtest as the password Handout “UA Chart” from the Sterling site – includes good information about drugs of abuse and UA test results Legal Drugs Our concern remains how the use impacts their ability to parent Treatment addresses these substances as well as illegal substances – clients can still access treatment Prescription drug abuse What works when working with people who abuse prescription drugs? | 16 of 17 Opiate replacement therapy Typically Methadone Addresses physical impacts of addiction Lowers risks associated with illegal use Highly monitored – program compliance required Particularly common for pregnant mothers Trainer’s Notes: Opiates include Heroin, Opium, morphine, prescription drugs like hydrocodone (vicodin) oxycodone (oxycontin), codeine, and Meperidine (Demerol) Replacement therapy uses a more stable, long acting drug to eliminate physical symptoms associated with stopping use (people aren’t getting high and coming down, they are receiving enough opiate to not get sick and it lasts all day) When those addicted to opiates are able to have their needs addressed via replacement therapy – they reduce all sorts of physical/health risks that they took on when they were using Provided as part of a medically managed treatment program – participants are typically working with programs to address many aspects of their addiction and regain social and life skills their addiction has compromised When women are pregnant, detoxing from opiates will often cause spontaneous abortion. For that reason, pregnant women are generally monitored on methadone and when they deliver their babies may have to detox Trainer Resource: http://www.drugabuse.gov/publications/research-reports/heroinabuse-addiction/what-are-treatments-heroin-addiction Substance Exposed Newborns | 17 of 17 CAPTA requires us to develop a “Plan of Safe Care” whenever we are notified that a child was born substance exposed. This plan must include: o Medical care for the child o Safe housing o Childcare if the parent plans to work or attend school o Emergency and community contacts for the parents o Referrals to drug/alcohol services and other services that are needed Because these are our most vulnerable children, and their mother’s are almost always addicted o Often means a safety plan of out of home care, o Or an in-home safety plan with a responsible adult (the other parent or a family member) monitoring or providing daily care and supporting the addicted parent in managing their addiction and their parenting tasks In each case, we do an individualized assessment of the situation to determine the best way to ensure that the child has his or her needs met and the family experiences the least intrusion possible There are several treatment centers in our state that accept women with their infants and these clients are high priority for admissions into treatment – so it’s a good idea to take advantage of any indication that they are interested in treatment ASAP An Array of Treatment Approaches While some individuals with mental health disorders will need to participate in treatment for the rest of their lives to manage their illness, others will see their illness lift on its own with little or no “formal” treatment | 18 of 17 No single approach to treating mental illness works for everyone or for every disorder, but there is a strong evidence base supporting certain approaches for certain concerns Often, particularly in cases where mental illness has significant impacts in a variety of life spheres – a combination of therapeutic work with a counselor and psychotropic medication may have the best chance for producing significant and long lasting positive changes Life changes can also have a significant impact on mental illness Circumstances like living in poverty, living with a chronic illness, and living in a violent context have significant impacts on people’s mental health. Significant evidence exists that addressing these contexts (providing concrete resources, getting a chronic condition under control, helping someone get safe housing or escape a violent relationship) has a significant impact on mental health functioning. Further, there is good evidence that regular exercise is as effective at treating mild depression and anxiety disorders as is medication. Psychotropic medications Medications have greatly increased quality of life for many people – particularly those suffering from psychotic and mood stabilization disorders Psychotropic medications are not a panacea – they carry possible benefits as well as risks. Some medications may lose their effectiveness over time, and others can be used indefinitely with good results In most cases, psychotropic medications don’t restore functioning, they improve functioning. Much work may still have to be done by the person living with mental illness to gain skills and coping mechanisms to deal with the impact of the mental illness that isn’t addressed/mitigated by the medication. | 19 of 17 Co-Occurring Disorders and What works with this population Employ a recovery perspective Adopt a multi-problem viewpoint Develop a phased approach to treatment Address Specific Real-Life Problems early in Treatment Plan for the client’s cognitive and functional impairments Use support systems to maintain and extend treatment effectiveness SAMSA publication TIP #42 – Substance Abuse Treatment for Persons with Co-Occurring disorders Employ a recovery perspective o Taking the long view of recovery, recognizing the importance of settings other than the treatment milieu for gradual progress, building and reinforcing connections to these ongoing support systems (self-help groups, positive peer support systems, extended family, cultural, spiritual or civic groups) Adopt a multi-problem viewpoint o Many people with co-occurring disorders have significant gaps in life skills, concrete resources, healthy relationships, emotional self-regulation and employment skills, as well as outstanding medical problems. o All of these areas must receive attention in order for long term recovery to be supported. o Programs which have built in components focusing on these, or which allow staff to focus on these areas as part of the overall treatment approach, have better outcomes. Develop a phased approach to treatment o Again, a long view to treatment where everything from initial experiences with the counselor/agency which build trust and prove helpful through supports and continued aftercare when a client is not receiving ongoing services from the agency are included in the model. o In this way clients are widely conceived as “eligible” for services and as benefiting from an array of supports that treatment can offer. Address Specific Real-Life Problems early in Treatment | 20 of 17 o Housing, legal, and family matters have often been identified by clients as the most pressing issues they currently face. o Programs that address these areas early, when a client identifies that they are at a crisis point, are able to retain clients in treatment at greater rates than those programs that use a “recovery first” model. Plan for the client’s cognitive and functional impairments o Clients with co-occurring disorders often, and particularly initially, present with functional impairments that impact their ability to comprehend information and complete tasks. o Generally, relatively short and highly structured treatment sessions work best. Gradual pacing, visual aids, and repetition can also be key in impacting clients’ retention of information and skills. Use support systems to maintain and extend treatment effectiveness o Counselors within programs serving these clients may offer some services to an entire family system, and often also helps the client identify new systems/groups where membership can be achieved and healthy support attained. Slide 30 - The intersection of chemical dependency, mental health, and trauma Experiences of trauma increase the likelihood that a person will experience a mental health disorder Because people with mental health disorders and chemical dependency issues are often quite vulnerable, both of these increase the likelihood that a person will have a traumatic experience Among high risk groups (those who have experienced rape or family violence, military combat, and immigrants fleeing ethnic/political persecution) the percentage of people qualifying for a PTSD diagnosis ranges from 1/3 to ½. | 21 of 17 It’s estimated that at least 55% of women in substance abuse treatment have had a traumatic experience (most commonly childhood physical/sexual abuse, domestic violence or rape). Women with substance abuse disorders are about twice as likely as men to qualify for a PTSD diagnosis. Of women in substance abuse treatment who have a past traumatic experience, 33-59% are experiencing current symptoms of PTSD. Becoming abstinent from substances DOES NOT generally improve symptoms of PTSD (though it does reduce the likelihood of future traumatic experiences), and clients should receive concurrent or integrated help for these symptoms in order to improve long term odds for sobriety Teaching specific coping skills for PTSD symptoms early in treatment is often associated with better outcomes in substance abuse treatment (all the above from SAMSA publication TIP #42 – Substance Abuse Treatment for Persons with Co-Occurring disorders ncbi.nlm.nih/gov/books/NBK64197/) Direct participants back to the first slides in the slideshow. How would you think differently about these questions now? What information might you want in order to make these calls? | 22 of 17 | 23 of 17