Temporal Trends in Clinical Trials of NSTE ACS over 15 Years Mark
advertisement

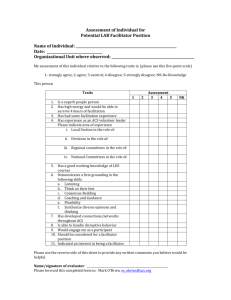
Temporal Trends in Clinical Trials of NSTE ACS over 15 Years Mark Y. Chan, Jie-Lena Sun, L. Kristin Newby, Harvey D. White, David J. Moliterno, Pierre Théroux, E. Magnus Ohman, Karen S. Pieper, Robert P. Giugliano, Paul W. Armstrong, Robert M. Califf, Frans Van de Werf, Robert A. Harrington Funding Sources • This work was supported by the Merck/Schering-Plough Alliance. Merck/ Schering-Plough was not involved in the design and conduct of the study, or the collection, management, analysis, and interpretation of the data. • The individual trials were funded by the following sponsors: GUSTO IIb: Ciba–Geigy, (Summit, N.J.), Boehringer Mannheim (Indianapolis), and Guidant (Redwood City, Calif.), PURSUIT: COR Therapeutics and Schering-Plough Research Institute, PARAGON-A: Hoffman La-Roche (Basel, Switzerland), PARAGON-B: F. Hoffman-La Roche Ltd. (Basel, Switzerland), PRISM: Merck & Co, Inc., PRISM-PLUS: Merck & Co, Inc., GUSTO IV ACS: Eli-Lilly and Co. Inc (Indianapolis, IN), SYNERGY: Sanofi-Aventis (Paris, France) Early ACS: Schering-Plough (Kenilworth, NJ). Disclosures HD White: grants from Schering-Plough, Merck; DJ Moliterno: grants, consulting from Schering-Plough; P Théroux: grants, speaker fees from Schering-Plough; RP Giugliano: grants, advisory board, honoraria from Schering-Plough, Merck; PW Armstrong: consulting for Merck Frosst Canada Ltd, grants from Schering-Plough, Merck; F Van de Werf: grants from Schering-Plough, advisory board, speakers fee from Schering-Plough, Merck. MY Chan, JL Sun, KS Pieper: none. Disclosures for LK Newby, EM Ohman, RM Califf, & RA Harrington may be viewed at http://www.dcri.duke.edu/research/coi.jsp. Background • • • • • Over the last 2 decades, phase III randomized controlled trials (RCT) of antithrombotic therapy in non-ST-segment elevation acute coronary syndromes (NSTE ACS) have defined contemporary treatment strategies for NSTE ACS. Concurrently, in part due to these and other trials, standard therapy for NSTE ACS has evolved and population characteristics and trial inclusion criteria have reflected progressively higher risk. We described temporal trends in study population risk and background therapy and outcomes in large randomized trials of antithrombotic therapy in ACS conducted consecutively over a 15year period. We also described the relationships between baseline risk profiles and background treatment trends and trends in clinical outcomes over this 15-year period. We hypothesized that, in a large series of consecutive NSTE ACS clinical trials, changes in risk profiles of study subjects would be counterbalanced by use of evidence-based background therapy and result in similar clinical outcomes over time. Methods • • • • • • We used data from 9 consecutive phase III, international, RCTs of antithrombotic therapy in NSTE ACS coordinated by the DCRI from 1994 to 2009. Data from GUSTO IIb, PURSUIT, PARAGON-A, PARAGON-B, PRISM, PRISM-PLUS, GUSTO IV, SYNERGY and EARLY ACS were merged at the patient level. 27,550 (47%) were diagnosed with unstable angina and 31,072 (53%) were diagnosed with NSTEMI. Baseline characteristics, discharge medicines, and in-hospital, 30day, and 6-month outcomes were trended across 15 years. Time trends were analyzed across 5 equal 3-year time periods, to maintain sample size homogeneity across comparison groups. Time trends were tested at a significance level of α=0.05. Year of Subject Randomization in Each Trial Time Trends in Population Characteristics Time Trends in Background Pharmacotherapy Pre-randomization Pharmacotherapy: 15-year Trend % 100 80 Aspirin 60 Thienopyridine ACE-Inh 40 β-blocker 20 Statin 0 1994-1996 1997-1999 2000-2002 2003-2005 2006-2008 Year Inhospital Pharmacotherapy: 15-year Trend % 100 80 Aspirin 60 Thienopyridine ACE-Inh 40 β-blocker 20 Statin 0 1994-1996 1997-1999 2000-2002 2003-2005 2006-2008 Year Discharge Pharmacotherapy: 15-year Trend % 100 80 Aspirin 60 Thienopyridine ACE-Inh 40 β-blocker 20 Statin 0 1994-1996 1997-1999 2000-2002 2003-2005 2006-2008 Year Time Trends in Outcomes Inhospital Bleeding: 15-Year Trend 35 30 25 Mild bleeding % 20 Moderate bleeding 15 Severe bleeding 10 5 0 1994-1996 1997-1999 2000-2001 Year 2003-2005 2006-2008 Inhospital, 30-day and 6-month Death: 15-Year Trend 7 6 % 5 Inhospital death 30-day death 6-month death 4 3 2 1 0 1994-1996 1997-1999 2000-2002 2003-2005 2006-2008 Year % Thirty-day Death or MI: 15-year Trend 16 14 12 10 8 6 4 2 0 30-day death 30-day MI 30-day death or MI 19941996 19971999 20002002 Year 20032005 20062008 Invasive Management: 15-year Trend 100 Cardiac catheterization % 80 60 Percutaneous coronary intervention 40 Coronary artery bypass grafting 20 0 19941996 19971999 20002002 Year 20032005 20062008 Conclusions • This analysis of 58,771 subjects from 9 consecutive large multinational phase III RCTs demonstrates an overall increase in subject risk and a rapid increase in the use of evidence-based background pharmacotherapies post-randomization and at discharge. • These trends were associated with a consistent decline in early and late mortality over 15 years. • Non-fatal MI rates increased over the 15-year observation period • Declining mortality rates and increasing non-fatal MI rates, the latter possibly driven by more sensitive cardiac biomarkers, greater procedural use andchanges in MI definition, warrant consideration of novel study designs and reassessment of MI adjudication strategies in future RCTs.