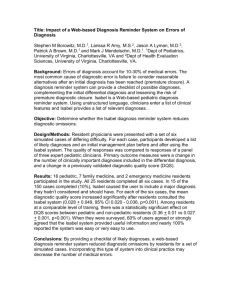
Slides - Health IT Safety Center Roadmap
advertisement

RTI International Health IT Safety Webinar Series How Can We Improve Diagnosis and Safety Using Health IT? May 8, 2015 1:00-2:30pm EDT RTI International is a trade name of Research Triangle Institute. 1 www.rti.org RTI International Housekeeping 2 For any technical questions, please type your question into the Questions panel at lower right. All telephone lines are muted. Due to the number of attendees, please use the Questions panel to ask any questions during the webinar. Closed captioning for today’s session is available at http://www.captionedtext.com/ Event #: 2618527 Q&A will take place at the conclusion of each presentation. Slides and a copy of the recording of this session will be posted at www.healthitsafety.org For general questions about the webinar series, please contact healthitsafety@rti.org RTI International Health IT Safety Webinar Series This series of 10 webinars focused on health IT and patient safety issues will occur monthly through September 2015. These webinars are funded by the Office of the National Coordinator for Health Information Technology (ONC) and are being conducted by RTI International, a non-profit research organization, as part of a year-long project to develop a road map for a Health IT Safety Center for ONC (contract HHSP23320095651WC). Additional information is available at: www.healthitsafety.org 3 RTI International Today’s Presentations Jason Maude, Founder and CEO, Isabel Healthcare Hardeep Singh, MD, MPH, Chief, Health Policy, Quality & Informatics, Michael E. DeBakey VA Medical Center and Baylor College of Medicine, Houston TX Michael Kanter, MD, Regional Medical Director of Quality and Clinical Analysis at Southern California Permanente Medical Group Mark Graber, MD, RTI International (Moderator) 4 RTI International Today’s Moderator 5 Mark Graber, a senior fellow in the Health Care Quality and Outcomes Program, joined RTI International in 2011, bringing more than 30 years of experience in academic medicine and health care research with a focus on quality of care and patient safety. Dr. Graber is an internationally recognized authority on diagnostic error in medicine and has published extensively in this area. He founded and chaired the first two Diagnostic Error in Medicine conferences in 2008 and 2009 and founded the Society to Improve Diagnosis in Medicine in 2011. The EHR - Enabling Diagnosis Collects & organizes all the relevant information Clear, legible record of notes, diagnostic tests and consults; Help organize thinking, planning, & follow-up Enables communication & care coordination Enables telehealth, research, predictive analytics Enables patient engagement (Open Records) 6 Using health information technology to reduce diagnostic errors. El Kareh, R; Hasan, O; Schiff, GD. BMJ Quality Safety 2013 doi:10.1136/bmjqs-2013-001884 Can electronic clinical documentation help prevent diagnostic errors? Gordon D. Schiff; David W. Bates; NEJM 2010; 362: 1066-9 7 How Health IT Improves Diagnostic Quality and Safety Decision support for DDX (DXplain, Isabel, VisualDX) Jason Maude, Founder of Isabel Trigger Tools -- Helps identify patients at risk for diagnostic error (revisits, admissions after a clinic appointment) Hardeep Singh – Baylor and Houston VAMC Safety Nets - Catching errors before there is harm Michael Kanter - Kaiser Permanente 8 RTI International Today’s Speakers Jason Maude serves as Chief Executive Officer and Founder of Isabel Healthcare Ltd, a company founded 10 years ago to develop tools to help physicians and patients improve diagnosis decision making after his daughter was badly misdiagnosed. Prior to founding Isabel Healthcare Ltd, Maude spent 12 years working in the finance industry in London at a number of top-ranked investment banks. Presentation: “Health IT to Enable Differential Diagnosis” 9 Isabel Healthcare “The right diagnosis and treatment-quicker” May 2015 Jason Maude CEO & Founder Isabel Healthcare 10 How it began - a nearly fatal misdiagnosis in 1999 Isabel Maude badly misdiagnosed as a toddler Isabel application inspired by this critical need to get the diagnosis right the first time. 11 Isabel Maude survived ~ and thrives today 12 Who is Isabel Healthcare? Isabel Medical Charity established 1999 Isabel Healthcare Ltd established 2004 Isabel Healthcare Ltd owned by charity (37%) and external investors (2 angels and 1 corporate) Established leader in diagnosis decision support systems for clinicians and patients Used by large health systems, hospitals, practices, individual clinicians and patients 13 Recognizing disease in time DX before = DX after = 14 Where do DX support tools fit? Even more specialists More specialists 10,000 to 12,000 diseases Specialists I just have these symptoms Emergency care PCP 200-300 diseases DX tools enable patients to be better informed about their symptoms and diagnosis and doctors to manage and refer more appropriately. 15 Brief history of DX support tools 1st generation started appearing in 1970’s ‘Artificial Intelligence’ (AI) or ‘Expert Systems’: if, then = DXplain, QMR, Internist New technology enabling 2nd generation tools from 2000 - Isabel Statistical Natural Language Processing (SNLP) = pattern matching Natural Language Processing (NLP) = what does it mean 3rd generation tools use NLP+SNLP = Isabel Active Intelligence/IBM Watson 16 Isabel Performs 2 Essential Functions 1. Hypothesis generation 2. Fast gateway (with no additional logins) to Clinical Reference Resources • Evidence Based content from Dynamed/ BMJ’s Best Practice and various external web based resources • Point of Care information on key symptoms, 1st and 2nd line tests and treatment guidelines. • Draws clinicians attention to knowledge when needed 17 When do Isabel? Why wait, clinicians useyou Isabel for… What we do Patients with whom there is a diagnostic doubt Referral for diagnosis Appropriate tests to order Latest treatment guidelines Training/Education 18 Long validation process- over 30 published articles • Study showed 22% increase in diagnostic skills in 4th Year Medical Students 22% Skills Improvement 29% of Doctors Reduced Referrals 36% Redirected Referrals • Study in UK primary care showed that after using Isabel, in 29% of cases GP did not need to refer and 36% of cases helped refer more appropriately • Recent systematic review by NIHR at Univ of Manchester highlighted Isabel as most accurate tool and concluded that “DDX tools are potentially an efficacious way of reducing or preventing diagnostic errors” 19 Demonstration-one portal for all questions 20 Demo: Get Checklist 21 Demo: Dynamed 22 3rd generation dx support within Cerner Differential Diagnoses within ‘Smart Zone’ Implementation…….the hard bit! 1. Must be part of institutional strategy 2. Clinical Leadership 3. A passionate champion 4. Made part of routine care 5. Continual awareness DX support is the means not the end 25 Every month 80% of population report symptoms 26 Google • 100 billion searches made through Google per month • 5% or 5 billion health searches made per month 27 For patient, Isabel performs 3 essential functions 1. Enables them to build own differential diagnosis and become informed - suggest that doctor thinks about a disease 2. Links to relevant and credible patient information 3. Helps them decide where to present 28 Hospital branded symptom checker 29 Hospital specific triage and venues 30 Engaging patient before visit Providing information previsit can improve efficiency and manage expectations • • • Data collected from symptom checker • Gets patient to think about their symptoms prior to visit • Allows patient to add other comments Customized questions to collect additional info that can assist during the visit Info can be sent to EMR, emailed to practice/physician pre-visit 31 Myth vs Our Experience What most think Consumers armed with material found on the internet are more difficult to deal with Most searches are done with one symptom Consumers get spooked when presented with conditions that are “scary” What we know Only 12-13% of searches on our public site consist of single symptoms Not a single complaint from organizations using the tool for engagement about difficult patients Almost 100% positive feedback from consumers! 32 Recognising disease in time - using DX support! DX before = DX after = 33 RTI International Today’s Speakers Dr. Singh is Chief of the Health Policy, Quality & Informatics research program at the Houston VA Center for Innovations in Quality, Effectiveness and Safety, and Associate Professor of Medicine at Baylor College of Medicine. He conducts multidisciplinary research on diagnostic errors, and on using health information technology to deliver safe and effective patient care. He co-developed the "ONC SAFER Guides" for safe and effective electronic health record use under a contract with Office of the National Coordinator for Health IT. He is a Fellow of the American College of Medical Informatics (ACMI) and received the 2012 Presidential Early Career Award for Scientists and Engineers from The White House. Presentation: “Measuring Missed Opportunities in Diagnosis in Health IT-Enabled Health Systems.” 34 MEASURING MISSED OPPORTUNITIES IN DIAGNOSIS IN HEALTH IT-ENABLED HEALTH SYSTEMS HARDEEP SINGH, MD, MPH HOUSTON VETERANS AFFAIRS CENTER FOR INNOVATIONS IN QUALITY, EFFECTIVENESS & SAFETY MICHAEL E. DEBAKEY VA MEDICAL CENTER BAYLOR COLLEGE OF MEDICINE 35 Objectives 36 In context of health IT-enabled health systems: Discuss lessons learned in measurement of missed opportunities in diagnosis Discuss how we can make progress in reducing them Key to Reducing Misdiagnosis 37 We cannot improve what we cannot measure And We cannot measure what we cannot define! Early Work 38 Evaluated evidence of ‘errors’ in an integrated system Detailed review of comprehensive EHR to evaluate diagnostic process in the patient’s journey across the continuum of care Data available from primary care, specialty (secondary) care, ER, hospital, diagnostics (lab/imaging/pathology), procedures 39 39 High Level Findings 40 Common conditions missed in outpatient settings despite clear red-flags (1 in 20 US adults/year) Abnormal test results missed about 8-10% of the time Better understanding of where to focus Singh et al BMJQS 2014; Singh et al Am J Med 2010 & Singh et al Archives of Int Med 2009 Defining Preventable Diagnostic Harm 41 MISSED OPPORTUNITIES A Missed opportunities in diagnosis due to system and/or cognitive factors HARM (from delayed or wrong treatment/test) B Preventable diagnostic harm C NO MISSED OPPORTUNITIES D Delayed/wrong diagnosis associated with patient harm but no clear evidence of missed opportunities Delayed/wrong diagnosis but no clear evidence of missed opportunities Adapted from Singh Jt Comm J Qual Patient Saf 2014 Intersection of Health IT & Diagnostic Safety 42 Our goals are to use health IT to measure and reduce diagnostic errors and harm, but .. Current Reality: Trying to ensure health IT itself is being used ‘safely’ Adapted from Sittig & Singh N Engl J Med. 2012 43 Diagnostic Safety in the EHR Era 44 EHRs must support provider cognition and decision-making What else besides innovation getting in the way? Use of templates and documentation issues Reduced physician efficiency Data display issues leading to ambiguity “iPatient” and effect on critical thinking skills? E-Communication breakdowns persist Sittig et al JAMIA 2015 45 And More Digital Data Is on the Way 46 Smartphone Wearables “Patients can now continuously monitor their data real-time and send it to their docs” Lessons from Research 47 EHR-based systems better than paper Not achieving full potential Need sociotechnical approaches to improve diagnostic safety Sittig and Singh JGIM 2012; Sittig and Singh QSHC 2010 8-dimensional Socio-Technical Model of Safe & Effective Health IT Use 48 Workflow & Communication External Rules & Regulations Organizational Policies, Procedures, & Culture Content Personnel Hardware & Software Measurement & Monitoring Sittig and Singh QSHC 2010 To Enable Rigorous Measurement 49 Missed opportunity measurement must reflect real-world practice more than just what’s in “the doctors head” systems, team members, and patients, all inevitably influence clinicians’ thought processes Singh BMJQS 2013 50 Safer Dx Framework for Measurement & Reduction Singh & Sittig BMJQS 2015 50 ‘Triggers’ Facilitate Measurement & Reduction 51 Patient-Primary Care Provider Encounter Diagnostic Tests Trigger More Patient-Provider Encounters Trigger Consultations to Sub-specialists Trigger Correct Diagnosis Certain Diagnosis Uncertain Diagnosis Singh & Thomas AHRQ Special Report 2009 Why Triggers Are a First Step? 52 Algorithms to select high-risk patient records for further reviews to look for missed opportunities Picking up ‘needles in a haystack’ by making the haystack smaller Application retrospective or prospective surveillance Singh et al JAMA IM 2013 Electronic health record-based triggers to detect potential delays in cancer diagnosis Daniel R Murphy,1,2 Archana Laxmisan,1,2 Brian A Reis,1,2 Eric J Thomas,3 Adol Esquivel,4 Samuel N Forjuoh,5 Rohan Parikh,6 Myrna M Khan,1,2 Hardeep Singh1,2 53 Time for Surveillance & Safety Net? 54 Creating ‘intelligence’ related to diagnostic safety needs resources and time investment Institutions/practices have many competing priorities Will it give bang for the buck outside of research? Contacting docs Unintended consequences need to be monitored More (or unnecessary) testing/treatment could occur Zwann and Singh Diagnosis 2015 55 The Checklist is structured as a quick way to enter and print your self-assessment. Your selections on the checklist will automatically update the related section of the corresponding recommended practice worksheet. 56 SAFER Guides ; Sittig, Ash, Singh. Am J Manag Care. 2014 The Worksheet provides guidance on implementing the Practice. Take Home Messages 57 Health IT needs to be leveraged to start exploring, understanding and possibly reducing missed opportunities in diagnosis Plenty of tools and strategies available to start addressing diagnostic safety related to missed follow-up issues Thank you… 58 Funding Agencies Department of Veterans Affairs Agency for Health Care Research & Quality National Institute of Health Office of National Coordinator (SAFER Guides) Multidisciplinary team at Houston-based VA Health Services Research Center of Innovation Contact Information… Hardeep Singh, MD, MPH hardeeps@bcm.edu @HardeepSinghMD RTI International Today’s Speakers Dr. Kanter provides oversight of quality activities to improve care for the 3.5 million members in the Southern California Kaiser Permanente Region, including HEDIS results, JCAHO core measures, Leapfrog survey results, peer review, and hospital quality and performance improvement. His interests include patient safety, risk management, population care management, technology assessment and deployment of new technology, creation and implementation of evidence-based guidelines, laboratory utilization management, and analysis of outpatient access and patient satisfaction data. Presentation: “Using Health IT as a Safety Net for Diagnostic Errors.” 59 USING HEALTH IT AS A SAFETY NET FOR DIAGNOSTIC ERRORS MICHAEL H KANTER MD MEDICAL DIRECTOR FOR QUALITY AND CLINICAL ANALYSIS SOUTHERN CALIFORNIA PERMANENTE MEDICAL GROUP 60 Types of Diagnostic Errors Availability heuristic Anchoring heuristic Failure to follow up abnormal tests Information overload Visual diagnostic errors Diagnostic Errors Framing effects Blind obedience Premature closure 61 Kaiser Permanente SCAL SureNet A regional program that systematically identifies patients who have inadvertent lapses in care Using a small, centralized team with limited clinical scope capacity to intervene before harm reaches the patient As well as several automated electronic tools, consistently used by accountable frontline staff, to track certain abnormal results for all members 62 Current Portfolio Diagnosis Detection/ Follow Up • PSA Electronic Safety Net • +FIT Electronic Safety Net • Abnormal Pap Electronic Safety Net • Kidney Disease (Repeat Creatinine) • High Risk CKD Follow-up • Colon Cancer (Iron Deficiency Anemia/Rectal Bleeding + No colonoscopy) • Maternal Hepatitis B • Abdominal Aortic Aneurysm Tracking • Post Splenectomy Immunizations • Positive Chlamydia Follow up • Down Syndrome Care Coordination • Sickle Cell Care Coordination • Hepatitis C (+Antibody + No confirmatory test ) • Newborn Hearing Screening • Lung Nodules • Unintended Pregnancy Follow up Medication Safety • Annual Lab Monitoring: Digoxin (K+, level and SCr), Diuretics (K+ and SCr) • Amiodarone (Preventive monitoring plan) • Acetaminophen Overuse • Elderly Care Drug-Disease (Falls) • Elderly Care Drug-Disease (Dementia) • Elderly Care High Dose Digoxin Conversion • Interacting Statin Combinations (Gemfibrozil and/or Amiodarone) Counseling / • Diuretic MedicationPost-TAB Induced Hyponatremia Birth Control • Medication Induced Hyperkalemia • NSAIDs in CKD 4-5, Dialysis, Kidney Transplant • INH ALT monitoring • Monitoring Plaquenil Eye Monitoring • Metformin B12 monitoring • Ethambutol eye monitoring 63 PSA Safety Net • Identify cases of elevated PSA • Remove those with a diagnosis of prostate cancer • Remove those with a follow up appointment in urology, oncology, or radiation therapy • Remove those in hospice or palliative care • Remaining cases require chart review using existing prostate cancer case managers 64 PSA SureNet: Results Three Year Period 8,076 patients for case management 3,833 patients received Urology appointments 2,204 patients underwent prostate biopsy 745 Prostate Cancers diagnosed Zero claims related to missed abnormal PSA’s • 65 CKD Diagnosis Detection: Unrepeated Creatinine 12,396 lab orders placed for patients with an abnormal creatinine not repeated after 90 days 6,981 total labs repeated within 90 days (56.3%) 3,668 (52%) New CKDs identified • 66 Diagnosis Detection and Follow Up : Rectal Bleeding w/o Colonoscopy Chart review revealed delays in diagnosis of colorectal cancer due to lack of follow up on patients with a history of rectal bleeding with endoscopy • • • • M/W 55-75 (not terminally ill) No colonoscopy in past 10 years GFR > 60 History of rectal bleeding • Outpatient encounter with ICD9 diagnosis code of 569.3x or 455.xx 67 Diagnosis Detection and Follow Up : Rectal Bleeding w/o Colonoscopy 168 patients with a history of rectal bleeding and no colonoscopy identified 26 completed colonoscopy 6 had normal results 1 patient had an adenocarcinoma with spread to local lymph node, 1 had a carcinoid tumor 7 had one or more tubular adenomas, 11 had one or more hyperplastic polyps, hemorrhoids or colitis 68 Why are abnormal results not followed up? • Huge volume of testing requires > 6 sigma level of reliability • Formatting of reporting results may not be conducive to seeing abnormalities • Lack of systems to manage abnormal results • The patient is a critical part of the system • EMR does not solve the problem • Handoffs between physicians and/or providers • Problem requires future study. 69 IT Issues to Consider • Use discrete data whenever possible while avoiding free text comments • Understand what data you have access to • • • • • • • • Claims Laboratory Radiology Pharmacy Office visits Hospitalizations Diagnosis/diagnostic codes Procedure codes • Understand where you can get help – physician office staff, case managers, etc. 70 Process for New Electronic Clinical Surveillance Programs – Kaiser Permanente SureNet In addition to Subject Matter Experts, SMES panel always includes: • Leadership • Clinical guidelines • 71 Criteria for Evaluating Electronic Clinical Surveillance Programs • CLINICAL IMPACT—Will it improve patient safety or quality? • If yes, • How many people will be affected? • What is the severity of the potential safety gap? • IDENTIFICATION—Is the potential safety gap readily identifiable using existing electronic health data? That is: • Is the information required discretely coded? • If the information required is not discretely coded, is it noted consistently in a way that makes natural language processing a reasonable option? • If the potential safety problem is not readily identifiable, is it important enough that revisions to existing documentation should be considered? • 72 Important Cultural Issues for Diagnostic Errors • Blame-free culture • Feedback to physicians needs to be such that the physician will stay engaged with closing the loop on the diagnostic error (inform the patient and provide appropriate follow up care) • Diagnostic error continues until the correct diagnosis is made • Encourage reporting errors and near misses by rapidly building new safety nets based on these reports • Transparency is required • Initial launch of new program may identify larger prevalence of cases of errors even if the annual incidence is not so great 73 Important Practical Issues for SureNet Program Success • SureNet programs should have small impact on the physicians practice • Need to balance the false positive notification of a possible error against the sensitivity of the net but for the most part favor specificity over sensitivity • Do as much as possible for the physicians, which may include notifying the patient to get repeat labs or other studies • Get buy in to new programs prior to implementation • Use physician champions to help promote programs 74 Justifying the Cost of a SureNet Program • Create some that will decrease malpractice litigation • Minimize manual review of records which is costly • If possible measure errors identified • allows for assessing if program is achieving anything • allows for improvement over time and removal of waste • 75 Problems Likely to Occur in a SureNet Program • Angry Patients • May discover errors many years old in HCV and creatinine safety nets • May discover delay in diagnosis of cancer • Angry Physicians • May be upset if they are notified of a potential error and, in fact, no such error occurred • May be upset if the patient gets upset and blames the physician • Upset staff managing the program • Conversations with upset patients or physicians are difficult • Ethical issues may arise on when to notify patients of bad outcomes vs. risk of getting sued • 76 Summary • Harms from failure to follow up on abnormal results can be mitigated using Health IT • Every delivery system will have a somewhat different approach • It is not necessary to know the baseline rate of errors • Cultural issues need to be addressed 77 RTI International Questions and Wrap Up Speaker Contact Information Next Webinar – planned for Jason Maude Jason.Maude@isabelhealthcare.com Hardeep Singh hardeeps@bcm.edu Michael Kanter Michael.H.Kanter@kp.org 78 EHR Usability and Health IT Safety June 18, 2015 1-2:30p EDT Please visit: www.healthitsafety.org or contact healthitsafety@rti.org for more information on the entire webinar series