Contraception, Sterilization and Abortion
advertisement
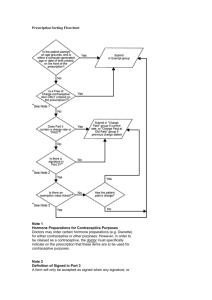
Contraception, Sterilization and Abortion Alternatives, Counseling and Management Suzanne Trupin, MD Women’s Health Practice Clinical Professor of Obstetrics and Gynecology Contraceptive Practices in USA The typical American woman wants only two children; she spends roughly five years pregnant or trying to become pregnant, and three decades trying to avoid unwanted pregnancy. Yet many women find it difficult to practice contraception consistently or correctly over the course of their entire reproductive lives and lack the information and services that would assist them in doing so. As a result, roughly one in three American women will have had an abortion by age 45. Counseling: GATHER Greet the patient in a warm and friendly manner, help her to feel at ease (Gather information on what she knows) Ask the patient about her needs and goals, STI risks nondirective counseling improves outcomes Tell the patient about her choices Help her decide Explain the correct use of the method or drug being prescribed Repeat important instructions and set up Return appointments World Population Growth Oct 12th 1999 we reached 6 billion, US just reached 300 million this year Mourning Picture for Polly Botsford and Her Children (c. 1813) Medical Evaluation for Contraception Prescription: WHO Class A: Mandatory Pelvic for IUD, Cervical Cap and Diaphragm, Sterilization STI risk for IUD BP screening for women getting sterilization Class B: Contributes substantially to safe and effective use, but consider context Hb for IUD and Sterilization Class C: does not contribute substantially to safe and effective use of the method U.S. Pregnancies: Unintended vs. Intended Intended 51% Unintended 49%: Unintended births 22.5% Elective Abortions 26.5% Henshaw: Fam Plann Perspect 1998;30:24-29. Incidence of Fatal Complication Pregnancy & Childbirth 11 2.6 Laparoscopic Sterilization Hormonal Contraception 1.5 1 6 11 Exposure Per 100,000 Woman Years Ory Fam Plann Perspect 1983;15:50-56. Long-Term Reversible Contraception: A dialogue among Andrew M. Kaunitz MD, David A. Grimes, MD, and Anita L. Nelson, MD, held on October 29, 2006. OBG Management: S1-S10, December 2006. Cost Estimates of Contraception & Pregnancy over 5 Years: No method over 5 yrs: 4.25 unintended pg at cost of %14, 663 $5,700 $5,730 $6,000 $4,872 $5,000 $4,102 $4,000 $3,278 $3,450 $3,000 $2,424 $2,584 $1,784 $2,000 $1,000 $3,666 $2,042 $1,290 $540 $764 $850 $0 Copper-T IUD Injectable Male Condom Periodic Abstinence Female Condom Trussel: Am J Public Health, 1995;85:494-503. Categories of Contraceptive Risk WHO Category 4 (old ‘contraindications’, now ‘refrain from use’) Condition which represents an unacceptable health risk if the contraceptive method is used. Do not use the method. WHO Category 3 (exercise caution) A condition where the theoretical or proven risks usually outweigh the advantages. Use of method is not usually recommended WHO Category 2 (advantages outweigh risks) Generally use the method with clinical judgement WHO Category 1 (no restrictions) Use of Contraception with Coexisting Medical Conditions FDA package labeling is the same for POP as COC without supporting evidence in many cases Current labeling for Norethindrone POP no longer lists history of thromobembolism as contraindication but does for norgesterel POP Conditions that expose a woman to increased risk as a result of unintended pregnancy Breast cancer or Estrogen Dependent Neoplasia Complicated valvular heart disease Diabetes: Vascular Complications WHO Category 4 most apply to COC, R, P Known thromobegenic mutations do not use COC or CIC Uterine Fibroids with cavity distortion do not use Cu-IUD or LGN-IUD PID or purulent cervicitis or active GC or CT do not Initiate IUDs For conditions of high risk of HIV and AIDS spermacide use is a category 4 Cerebrovascular or coronary artery disease multiple risk factors Migraines with Aura or migraines over the age of 35 Lactation (<6 weeks postpartum) do not use COC, P, R Liver disease Headaches with focal neurologic symptoms Major surgery and prolonged immobilization Age >35 years and smoke >14 cigarettes per day or more do not use COC, P, R Hypertension (blood pressure of >160/100 mmHg or concomitant vascular disease) Venous thromboembolism history Major surgery with prolonged immobilization WHO Category 3 (exercise caution) Postpartum <21 days Lactation (6 weeks to 6 months) Age >35 years and smoke <15 cigarettes per day History of breast cancer but no recurrence in past 5 year Interacting drugs (that affect liver enzymes) Gallbladder disease WHO Category 2 (advantages outweigh risks) CIN Severe headaches after initiation of oral contraceptive pills Undiagnosed vaginal or uterine bleeding Diabetes mellitus Major surgery without prolonged immobilization Sickle-cell disease or sickle-cell hemoglobin C disease Blood pressure of 140/100 to 159/109 mm Hg Undiagnosed breast mass Obesity Age >40 years High BP in Pregnancy Conditions predisposing to medication noncompliance Family history of lipid disorders Family history of premature myocardial infarction or DVT Uncomplicated valvular heart disease WHO Category 1 (no restrictions) Postpartum >=21 days Pos-tabortion, with abortion performed in first or second trimester History of gestational diabetes Varicose veins Mild headaches Irregular vaginal bleeding patterns without anemia Past history of PID Current or recent history of PID Current or recent history of STD Vaginitis without purulent cervicitis Increased risk of STD HIV-positive or at high risk for HIV infection or AIDS Benign breast disease Family history of breast cancer or endometrial or ovarian cancer Cervical ectropion Viral hepatitis carrier Uterine fibroids Past ectopic pregnancy Thyroid conditions Oral Contraception Oral Contraceptives and Shorter Acting Steroid Contraception Contraceptive Cases A 16 year old wants pills but refuses a pelvic, do you give them to her? 19 year old U of I sophomore says her menses comes on Sunday, so she wants to know does she start this Sunday or next? To take a break from pills a 21 year old stops the pills for a month while her partner is off visiting medical schools. How long a break does she need? A 16 year old presents with her mother requesting pills for acne, the mother insists you give her the ones that are the cheapest, the patient wants the ones she sees on TV that are good for your skin, which do you choose? A 23 year old is getting monthly PMDD, what do you advise? A 55 year old comes in on birth control pills from her previous physician, is this dangerous? A 26 year old with three previous ME presents for contraceptive advice, she has a sister and a mom with breast cancer and she refuses to take the pills, can she use them? Prescription of Oral Contraceptives Counseling Begin COC or POP at any time if reasonably certain is not pg If begun within 5 days of bleeding no extra protection If not within 5 days use back up for 7 days if on COC, and for 2 days if on POP Begin immediately post abortion Rapidly reversible, within 2-3 months conceptions are seen Medical history and physical examination Selection of a particular preparation User instructions Missed pill instructions No evidence that obese patients suffer decreased efficacy Establishing that a patient is protected by her contraception Mode of action for contraceptive protection Molecular: P suppresses LH, E suppresses FSH Cellular: E increases intracellular P receptors Reproductive Organs: Endometrial atrophy, hostile cervical mucus Reproductive Processes WHO in last report said that it is not reliably known how accurately ultrasound findings, hormonal measurements or evaluation of the cervical mucus predict the risk of pregnancy during most contraceptive use Pharmacologic Actions of Progestin and Estrogen Progestin Estrogen Ovarian and pituitary inhibition Ovarian and pituitary inhibition Thickening of cervical mucus Thinning of/increase in cervical mucus Endometrial atrophy/transformation Endometrial proliferation Cycle control Cycle control Progestins in Oral Contraceptives 19-Nortestosterone Estranes Norethindrone Norethindrone acetate Ethynodiol diacetate Norethynodrel Lynestrenol* Gonanes Levonorgestrel Norgestrel Desogestrel Norgestimate Gestodene* *Not available in the United States. Adapted from Sulak PJ. OBG Management. 2004;Suppl:3-8. Spironolactone Drospirenone Multiphasic vs Monophasic Preparations* 1.0 20 18 0.75 Norethindrone (mg) 0.5 10 0.4 menses 0 0 7 14 Day of pill cycle 21 Endogenous progesterone (ng/mL) 5 28 Monophasic (Ovcon 35) Multiphasic (Ortho Novum 7/7/7) Endogenous progesterone * Ethinyl estradiol content is constant (35 µg) for level 3rd ed. Adapted from Goodman and Gilman’s The Pharmacological Basis of Therapeutics. both preparations. 1996:1416. Available Formulations Monophasic: consistent dose in each active pill Phasic Preparations: dosing of E/P varies through the cycle Biphasic Triphasic Shortened pill-free interval Progestogen only containing pills Greater percentage of cycles are ovulatory (>50%) Typical Use Issues 8/year Failure greater if pills are miss early in cycle Contraceptive Efficacy of all marketed pills are similar 0.3% failure perfect use about 8.0% failure typical use Benefits are identical in spite of package insert Cardiovascular Impact of Risk Factors Venous= VTE (DVT, PE) Arterial= Strokes and MI • Obesity • Smoking • Pregnancy • Diabetes • Malignancy • Hypertension • Recent Surgery • Obesity Cases per 100,000 Woman-Years CV Mortality Risk with Smoking and OC Use 30 25 Oral contraceptive nonuser Oral contraceptive user 20 15 10 5 0 Attributable Risk/100,000 User-Years Nonsmoker Smoker 0.06 1.73 < 35 years of age Nonsmoker Smoker 3.03 19.4 ≥ 35 years of age Sherif K. Am J Obstet Gynecol. 1999;180(Pt 2):S343-S348. Risks of Oral Contraceptives: Nonfatal VTE Estimated Average Risk/ 100,000 Women/Year 100 80 60 40 20 0 Non-Oral Contraceptive Users Oral Contraceptive Users Food and Drug Administration. FDA Talk Paper. Nov. 24, 1995. Pregnant Women Cardiovascular Impact of OCs Venous • No difference in risk between 2nd- and 3rdgeneration progestins • No difference in risk among low-dose OCs (20 µg to 35 µg) • Increased clotting factors Arterial • Estrogens increase HDL • Progestins lower HDL • High E/P ratio increases HDL • Estrogen has a dilating effect on arterial wall Reproductive Tract Cancers 1.24 risk of breast cancer in OC users Existing cancers may have earlier development Protective effect Relative risk of cancer T BREAST against colon cancer Endometrial and ovarian cancer risk reduction is greater with increasing duration of use Duration of OC use Oral Contraceptives and the Risk of Breast Cancer Results of a large epidemiologic study suggest that oral contraceptives do not cause breast cancer Breast cancer risk in women who have not taken oral contraceptives for ≥10 years is the same as those who have never used them There is a slightly increased risk of diagnosis in current users of oral contraceptives and in those who stopped taking them ≤10 years ago Tumors are more likely to be localized in oral contraceptive users than in nonusers Collaborative Group on Hormonal Factors in Breast Cancer. Lancet. 1996;347:1713-1727; Collaborative Group on Hormonal Factors in Breast Cancer. Contraception. 1996;54:1S-106S. Acne and Androgen Metabolism Total testosterone Sex hormonebinding globulin Free testosterone 5-reductase Dihydrotestosterone AR Sebum production AR = androgen receptor within the sebaceous gland Azziz R, et al. Semin Reproduct Endocrinol. 1989;7:246-254; Imperato-McGinley J, et al. J Clin Endrocrinol Metab. 1993;76:524-528; Murphy AA, et al. Fertil Steril. 1990; 53:35-39; Pye RJ, et al. Br Med J. 1977;2:1581-1582. Higher Bone Density More Likely in OC Users OC users Non-OC users 100 80 60 40 20 0 4 1 2 3 (High) (Low) Bone Mineral Density Quartile Kleerekoper M et al. Arch Intern Med. 1991;151:1971-1976. Slide Source: ContraceptionOnline www.contraceptiononline.org Noncontraceptive Benefits of Oral Contraceptives BENEFITS DUE TO CONTINUOUS PROGESTIN Less endometrial cancer Less benign breast disease 50% reduction in breast tumors Fewer uterine fibroids Regular uterine bleeding Less amount uterine bleeding less anemia less salpingitis 50% reduction in PID Less cyclic mood changes (PMS) BENEFITS DUE TO INHIBITION OF OVULATION Less ovarian cancer Less ectopic pregnancies Less functional ovarian cysts Suppression better with 35 mcg EE Less dysmenorrhea OTHER BENEFITS Less acne and hirsutism Less rheumatoid arthritis Increased bone density Discontinuation of Oral Contraceptives % Discontinuing 12 10 8 6 4 2 0 Irregular Bleeding Nausea Weight Gain Mood Changes Rosenberg MJ, et al. Am J Obstet Gynecol. 1998;179:577-582. Breast Tenderness Headaches Shortened Hormone-Free Intervals Brand Name Estrogen Dose Progestin Dose Regimen Seasonale® 30 µg EE 150 µg levonorgestrel 84/7 SeasoniqueTM 30 µg EE 150 µg levonorgestrel 84/7* *7 days 10 µg EE Yaz 20 µg EE 3 mg drospirenone 24/4 Loestrin 24 Fe 20 µg EE 1 mg norethindrone acetate 24/4* *4 days of iron Lybrel 20 µg EE 90 µg levonorgestrel 365 days (non-cyclic daily dosing) EE= ethinyl estradiol Median Number of Breakthrough Bleeding/Spotting Days/Cycle Breakthrough Bleeding and Spotting and Extended Regimen 12 10 8 6 4 2 0 Cycle Day 1 2 3 4 1-84 92-175 183-266 274-357 *30 µg ethinyl estradiol/150 µg levonorgestrel. Anderson FD, Hait H. Contraception. 2003;68:89-96. Vaginal Ring: NuvaRing NuvaRing releases 15 g of ethinyl estradiol and 120 g of etonogestrel daily Worn for 3 out of 4 weeks Self insertion and removal it is about 2.1 inches in diameter Pregnancy rate 0.65 per 100 woman–years If removed for >3hrs use back up method for 7 days Roumen FJ, et al. Hum Reprod. 2001;16:469475. www.contraceptiononline. Vaginal Contraceptive Ring: Administration If Ring Is removed If under three hours reinsert If over three hours 4 mm reinsert and use 1 week of back up Only 2.6% of women report ring expulsion 54 mm www.contraceptiononline. NuvaRing Compared to OC: Intended Bleeding Pattern ® 75 ** ** NuvaRing® * COC * * 4 5 50 25 0 *P<0.01 **P<0.0001 1 2 3 Cycle Bjarnadottir RI, et al. Am J Obstet Gynecol. 2002;186:389395. www.contraceptiononline. Contraceptive Patch: Ortho Evra Patch contains 6 mg norelgestromin and 0.75 mg ethinyl estradiol Delivers continuous systemic doses of hormones 150 -250 µg norelgestromin (NGMN) 20-25 µg ethinyl estradiol (EE) Direct comparisons to oral contraceptive delivery doses cannot be made but compliance enhanced Per day If patch is removed for >24 hours apply a new patch and use back up for 7 days and the day of the week for patch change is now the day you found the patch off www.contraceptiononline. Transdermal Patch: Disadvantages Application site reactions Not as effective in women weighing >198 pounds Side effects are similar to oral contraceptives except for: - higher rates of breast pain during first 2 months higher rates of dysmenorrhea May be difficult to conceal No protection against HIV or other sexually transmitted infections - Zieman M, et al. Fertil Steril. 2002;77(Suppl 2):S13-S18. Patch: Patient Counseling Application: Use a new location for each patch Apply to clean, dry skin Apply where it won’t be rubbed by clothing: on buttocks, abdomen, upper outer arm, upper torso Do not use on irritated or abraded skin Do not use on the breasts Avoid oils, creams, or cosmetics until after patch placement Bathe and swim as usual Anticipate more breast discomfort during the first 2 months Store at room temperature Do not cut, alter or damage the patch as if may alter contraceptive efficacy Do not flush a used patch into the water system; fold the used patch in half and place in the trash Patch: Managing 28-Day Cycle (Days 1-28) Patch #1 Patch #2 Patch #3 Days 1-7 Days 8-15 Days 16-21 Next 28-Day Cycle (Days 29-56) No Patch Patch #1 This patch was not removed: • Remove immediately • Start cycle on day 29 Patch application is 1 to 2 days late: • Apply new patch immediately; Make this the new “patch change day” • No backup protection is required Patch application is >2 days late: • Immediately start new 21-day application cycle •Use backup protection for 7 days •Consider emergency contraception This patch was not applied: • Apply a new patch immediately; this is the new “patch change day” • Use backup protection for 7 days • Consider emergency contraception Breakthrough Bleeding and/or Spotting:Patch Versus Pill 20 18.3 Percentage of patients 18 Contraceptive Patch 16 Oral Contraceptive 14 11.4 12 10.0 10 8.8 9.5 7.1 8 7.1 6.7 6 4.6 5.5 4 2 0 1 3 Audet MC, et al. JAMA. 2001;285:2347-2354. ©2001, American Medical Association. Cycle 6 9 13 Estrogen Exposure: Patch, OCs, Ring Ring (15 µg EE/day) Patch (20 µg EE/day) * * 40 OC (30 µg EE/day) *P<0.05 vs ring and OC 30 180 *P<0.05 vs patch and ring 150 †P<0.05 vs ring † 120 20 90 60 10 0 30 AUC 0-21 (ng.h/mL) 0 Cmax (pg/mL) OCs = oral contraceptive; EE = ethinyl estradiol van den Heuvel, et al. Contraception. 2005;72:168-174. Transdermal Contraceptive Patch:Risk for VTE Events* Relevant Studies Odds Ratio (95% Confidence Interval) Jick SS, et al., 2006 0.9 (0.5–1.6) Cole JA, et al., 2007 2.4 (1.1–5.5) *Women should be counseled that all combined contraceptive products increase the risk of venous thromboembolic events; use of these products should be discontinued if a patient becomes immobilized. Jick SS, et al. Contraception. 2006;73:223-228; Cole JA, et al. Obstet Gynecol. 2007;109:339-346. What is Emergency Contraception? “A therapy for women who have had unprotected sexual intercourse, including sexual assault.” –ACOG Not just the “morning-after pill” – hormonal EC can be given up to 72 hours after unprotected intercourse PREVEN, Plan B upto 120 hours post IC but effective is reduced 150 mg of Levo Copper IUD (up to 5 days after ovulation) Mifepristone (off label, up to 120 hours after unprotected sex) ACOG Practice Bulletin. Int J Gynecol Obstet. 2002;78:191-198. LaValleur J. Obstet Gynecol Clin North Am. 2000;27(4): 817-839. EPC Effectiveness If unprotected sex during wk 2 or 3 8% will become pregnant if not treated 2% will be pregnant following use of combined ECP (equivalent to a 75% reduction) 1% will become pregnant if use emergency POP (equivalent to an 88% reduction) 0.1% will become pregnant following emergency copper IUD insertion (99% reduction) Even late in the cycle a % chance of pregnancy is possible There is an algorithm to predict when menses will come Long-Acting Steroid Contraceptive Options Contraceptive Cases A 22 year old healthy patient wants to use DMPA but she cannot get in to the office on her menstrual week as that’s the week she travels, can she start the shots any other time? A 33 year old breast feeding mom wants DMPA before leaving the hospital after her delivery, is this permissible? A woman has been on DMPA for greater than 2 years, should she continue? Should she get a Bone Density test? Depot-Medroxyprogesterone Acetate Depo-Provera - 150 mg of DMPA via deep intramuscular injection in the gluteal or deltoid muscle Depo-subQ Provera 104 - 104 mg of DMPA via subcutaneous injection into the anterior thigh or abdomen Mechanism of action:Duration of protection: 3 m(13 wks) Inhibits ovulation Suppresses levels of follicle-stimulating hormone and luteinizing hormone Eliminates surges in luteinizing hormone Thickens cervical mucus Prevents sperm penetration Reduces sperm transport in the fallopian tubes DMPA depot-medroxyprogesterone acetate =Atrophies the endometrium Slide Source: Contraception Online www.contraceptiononline.org Percentage of Women Experiencing an Unintended Pregnancy Injectables: Failure Rate Among Typical Users 10 9 8 8% 8% 8% 7 6 5 4 3% 3 2 0.1% 0.05% 0.5% 1 0 Combined Oral Contraceptive Patch Ring Injectable Contraceptive Hatcher R. In: Contraceptive Technology. 18th rev ed. 2004:461-494. IUD Implant Female Sterilization Subcutaneous DMPA : Decreased Bleeding Over Time Bleeding Only Spotting Only Bleeding/Spotting Amenorrhea Percentage of Patients Reporting 100% 80% 60% 40% 20% 0% Month 3 Jain J, et al. Contraception. 2004;70:269-275. Month 6 Month 12 Mean Change in Lumbar Spine Bone Mineral Density (%) DMPA: Changes in Bone Mineral Density Over Time DMPA (150 mg) 1 Nonhormonal contraceptive 0 -1 -2 * -3 * * -4 * * -5 -6 * 24 48 96 * * 144 192 240 Kaunitz AM, et al. Contraception. 2006;74:90-99. 48 96 Posttreatment During Treatment *P<0.001 24 (Weeks) Return to Fertility Cumulative Contraception Rate (%) 120 100 80 50th Percentile 60 40 DMPA users 20 Nonhormonal contraceptive users* 0 0 5 10 15 20 25 30 35 Months after Removal or Since Last Injection *Intrauterine device or other barrier method. Schwallie PC, Assenzo JR. Contraception. 1974;10:181-202. Timing of DMPA Initial injection: On day 1 to 5 of menstrual cycle Within first 5 days of the postpartum period if not breastfeeding After the 6th postpartum week if breastfeeding Immediately or within the first 7 days after an abortion Reinjection: At week 11 to 13 If injection is missed or late (+14 weeks), back-up contraception should be used and absence of pregnancy should be confirmed Implants Implanon Contraceptive Implants: Characteristics Serum levels of etonogestrel are detectable within hours of insertion Suppresses ovulation Occurs within 1 day of insertion Ovulation in <5% of users after 30 months of use Rapid return of fertility Menstrual cycle returns within three months Continuous contraceptive protection for three years Does not contain estrogen Appropriate for lactating women after the fourth postpartum week No fluctuating hormone levels Inconspicuous Requires clinician visit for insertion and removal Does not protect against sexually transmitted infections Croxatto HB Eur J Contracept Reprod Health Care. 2000;5 Suppl 2:21-28; Reinprayoon D et al. Contraception. 2000;62:239-246; Diaz S. Contraception. 2002;65:39-46; Mascarenhas L. Eur J Contracept Reprod Health Care. 2000;5 Suppl 2:29-34. IMPLANON™ Single-rod implant (4 cm in length and 2 mm in diameter) made of ethylene vinyl acetate and contains 68 mg of etonogestrel Duration of use: 3 years Pearl index: 0.38 with typical use Croxatto HB. Eur J Contracept Reprod Health Care. 2000;5 Suppl 2:21-28; Le J, Tsourounis C. Ann Pharmacother. 2001;35:329-336. Slide Source: Contraception Online www.contraceptiononline.org Contraceptive Implant: Tolerability A 2-year study investigated the efficacy and tolerability of IMPLANONTM (N=330) Reasons for discontinuing participation in the study: Irregular bleeding: 13% Other adverse events: 23% Adverse events attributed to the study medication: Acne: 14.5% Emotional lability: 14.2% Headache: 12.7% Weight gain: 12.1% Dysmenorrhea: 9.7% Depression: 7.3% Implant site symptoms: Mild pain of short duration: <5% The IMPLANON US Study Group. Contraception. 2005;71:319-326. Slide Source: Contraception Online www.contraceptiononline.org Contraceptive Implant: Noncontraceptive Benefits Percentage change from baseline Changes in Acne (n=315) 50% 70% 40% 60% 50% 30% 40% 20% 30% 20% 10% 10% 0% 0% Decrease Changes in Dysmenorrhea (n=315) No Increase Change Funk S, et al. Contraception. 2005;71:319-326. Decrease No Increase Change Intrauterine Contracetion IUD IUS IUC Contraceptive Case A patient wants to get her pap and her IUD but the nurse insists she come on her period for the IUD insertion, who is right? A 29 year old exotic dancer comes for an IUD insertion, her most frequent partner has offered to pay for it, do you recommend this method for her? The nurse asks you if you want to give the patient antibiotics before or after IUD insertion? A patient wants to know fertilization rates with IUDs? IUC History Guidelines overly restrictive in the past. These obsolete recommendations reflected concerns about infection and resultant infertility. This cloud of suspicion concerning infection has now been lifted from the IUD by data from both cohort and case-control studies. A landmark case-control study from Mexico City showed that among nulligravid women, use of a copper IUD was not associated with tubal infertility; in contrast, prior exposure to Chlamydia trachomatis was associated with a significant increase in risk.[1] Cohort studies from Norway[2] and New Zealand[3] have found that upon discontinuation of an IUD, women had problems with unwanted fertility, not involuntary infertility. Almost any woman interested in highly effective contraception can use an IUD. IUDs today are appropriate for women who have never been pregnant as well as for those who have had upper genital tract infection or a prior ectopic pregnancy. For example, the World Health Organization Medical Eligibility Criteria give nulliparity a category 2 rating, meaning that, in general, the benefits of IUDs for such women outweigh the potential harms. A few contraindications exist, such as an established pregnancy, undiagnosed uterine bleeding that might represent cancer, mucopurulent cervicitis, etc. Leukocytic Infiltration of Superficial Layers of Endometrium in Contact with IUD: Day 16 of Cycle LNG-IUS (Mirena®) Contraceptive efficacy due to cervical mucus change and sperm motility and function inhibition plus weak foreign body action. 20 mcg/d LNG (30 would suppress ovulation). 5 year cumulative failure rate 0.71/100 in 12,000 US women. Spotting for first 3-6 months of use. Low EP rate (0.2-0.6/1000) Rapid return to fertility. LNG IUS 1. As with other progestin- only methods, persistent follicles can occur (in less than 8 % of women). They do not require treatment. 2. Produces both cervical barrier and intrauterine barrier to fertilizaiton Pakarinen et al. Fertil Steril 1997;68:59 Candidates for IUDs: ParaGard T380 Nulliparous or parous women No longer a requirement to be mutally monogamous, but do avoid if high risk for STD or PID. Appropriate for all stages of reproductive life whether young, pg spacing or finished with childbearing. Not for someone with post-pg or post-ab infection within the past three months Uterine or cervical cancer Cervical infection Allergies. Possible Complications: IUS Symptoms Consider Return of menstruation Expulsion Fever/chills Infection Continuous bleeding and/or pain after first month post-insertion Irregular bleeding and/or pain in every cycle Missing string Perforation, infection, or partial expulsion Dislocation or perforation Dislocation or perforation PID Rate by Insertion IUD Combined WHO clinical trial data for all IUDs - 22,908 IUD insertions 8 (per 1000 woman years) 6 4 2 0 1 2 3 4 5 6 7 8 9 Month (first year) 10 11 12 2 3 4 5 6 7 8 Year Time Since Insertion Farley et al. Lancet 1992;339:785 IUD Counseling No risk of infertility after discontinuing IUC No increased risk of PID except in the first 20 days after insertion No difference in complications for parous or nulliparous women IUD Counseling, continued Cu IUD at any time in the cycle if it is reasonably sure she is not pg, no additional protection is necessary It is not known exactly how soon it becomes effective If she is less than 48 hours postpartum she can have a CuIUD, or 4 or more weeks post partum and amenorrhoeic she can have a either IUD inserted Immediately post first trimester abortion and post second trimester she can generally have the IUD inserted Cu-IUD can be inserted within 5 days of unprotected intercourse, not farther as the risk of serious pelvic infection and septic spontaneous abortion If the LNG-IUD has been inserted more than 7 days into the cycle use protection for 7 days Bleeding with IUD use Spotting or light bleeding is common during first 3-6 months for either IUD NSAIDs Amenorrhea with Mirena doesn’t require treatment Persistent problem work up for gynecologic causes Heavier than normal menses with the Cu-IUD NSAIDs Tranexamic acid (a hemostatic agent) Do NOT use Asprin Treat anemia If anemia persists remove the IUD Barrier Methods Contraceptive Cases A 18 year old reports that she and her partner were mutually stimulating each other and suddenly decided to have intercourse, she didn’t want to fuss with her diaphragm so she inserted a vaginal film immediately before penetration, was she protected? A woman’s cervical cap was discolored so she’s been cleaning it with Listerine, is it ok? Your patient is worried about HIV she makes her partner use two condoms but he thinks this is unsafe, who’s right? Phases of the Cervical Mucus Method Calendar (or calculation) method Basal body temperature (BBT) method Cervical mucus method (the Billings method) Sympto-thermal method Barrier Methods Not as effective as hormonal methods No hormonal side effects Most require concomitant spermicide Some methods available without prescription Efficacy is highly dependent on consistent and correct use Some require partner cooperation Vaginal insertion and removal may be unacceptable Increased risk of urinary tract infection when used with a spermicide Some require fitting by a clinician Most are less effective in parous women Some reduce sexually transmitted infections Diaphragm Efficacy: In a 28-week multicenter, randomized, parallel group study of unadjusted typical use (with spermicide), the probability of pregnancy was 7.9% Advantages: Can be inserted hours before intercourse Does not require removal between acts of intercourse Cost: Approximately $30.00 Mauck C, et al. Contraception. 1999;60:71-80; Trussell J, et al. Fam Plann Perspect. 1993;25:100-105, 135; Cates W Jr, Raymond EG. In: Contraceptive Technology. 18th rev ed. 2004:355-363; Cates W Jr, Stewart FH. In: Contraceptive Technology. 18th rev ed. 2004:365-389. Diaphragm: Disadvantages Some are made of rubber, a potential allergen Must be prescribed and fitted by a clinician Requires vaginal insertion and removal Spermicide must be reapplied before each act of intercourse Must be worn for at least 6 hours after last intercourse, but not more than 24 hours May increase risk of urinary tract infections and toxic shock syndrome, based on the package insert of the Ortho All-Flex® diaphragm Cates W Jr, Raymond EG. In: Contraceptive Technology. 18th rev ed. 2004:355-363; Cates W Jr, Stewart FH. In: Contraceptive Technology. 18th rev ed. 2004:365-389; Association of Reproductive Health Professionals. Non-hormonal Contraceptive Methods: A Quick Reference Guide for Clinicians. Available at: http://www.arhp.org/files/QRGNonHormonalContraception.pdf. Inserting a Diaphragm and Correct Position of a Diaphragm Contraindications to Diaphragm Use Uterine prolapse Large cystocele or rectocoele or poor pelvic musculature Retroversion of the uterus History of toxic shock syndrome Insert up to 6 hrs prior, keep for 24 hrs Current vaginitis or cervicitis Avoid antifungals, antibiotics, petrolum products Repeated urinary tract infections Allergy to latex rubber or spermicide Must use 2 tlbs spoons ( 2/3 full) Today® Sponge Efficacy: 12-month cumulative life-table pregnancy rate is 17.4% Parity affects failure rate: Nulliparous – 9% to 10% Parous – 19% to 21% Advantages: Made of latex-free material (polyurethane) One size fits all Cost: $17.00 for pack of six sponges Does not require a prescription Preloaded with nonoxynol-9 spermicide Can be inserted up to 24 hr before intercourse Can be left in place for up to 30 hours Kuyoh MA, et al. Contraception. 2003;67:15-18; Trussell J, et al. Fam Plann Perspect. 1993;25:100-105, 135. Today® Sponge Disadvantages: Vaginal insertion and removal Should remain in place for six hours after last intercourse May increase risk of urinary tract infections and toxic shock syndrome Not recommended for use more than once per day Reduced efficacy among parous women Cates W Jr, Stewart FH. In: Contraceptive Technology. 2004:365-389; Association of Reproductive Health Professionals. Non-hormonal Contraceptive Methods: A Quick Reference Guide for Clinicians. Available at: http://www.arhp.org/files/QRGNonHormonalContraception.pdf. Types of Cervical Caps Prentiff Lea’s Shield (Yama Inc) Oves Cervical Cap (Veos plc) FemCap (FemCap, Inc) Insert behind the pubic bone as far as it can go If greater than 8 hours since insertion give some vaginal estrrogen Female Condom Efficacy: . During the first year of typical use, 21% of women experience an unintended pregnancy Advantages: Provides some protection against sexually transmitted infections Does not require a prescription Can be inserted well before intercourse Made of latex-free material (polyurethane) Trussell J, et al. Fam Plann Perspect. 1994;26:66-72. Female Condom Disadvantages: May not be as effective against pregnancy as the male condom . Must be inserted and removed by woman Available in only one size Labeled for single use May be noisy Outer ring may be visually unappealing and uncomfortable Cates W Jr, Stewart F. In: Contraceptive Technology. 2004:365-389; Association of Reproductive Health Professionals. Non-hormonal Contraceptive Methods: A Quick Reference Guide for Clinicians. Available at: http://www.arhp.org/files/QRGNonHormonalContraception.pdf. Male Condom Efficacy: 6-month typical-use pregnancy probability: Two Types: Latex Polyurethane Latex condom - 5.4% Polyurethane condom – 9.0% Advantages: Provides greater protection against sexually transmitted infections than any other method of contraception Provides substantial protection against pregnancy when used with a spermicide Does not require a prescription Can be used with other methods Inexpensive and widely available Steiner, MJ, et al. Obstetrics & Gynecology 2003;101:539-547. Association of Reproductive Health Professionals. Non-hormonal Contraceptive Methods: A Quick Reference Guide for Clinicians. Available at: http://www.arhp.org/files/QRGNonHormonalContraception.pdf. Male Condom Two Types: Latex Polyurethane Disadvantages: Can be used for only one act of intercourse Can tear or slip during use, but this is less frequent with lubricated condoms May decrease sexual pleasure May interfere with spontaneity Requires cooperation of male partner Association of Reproductive Health Professionals. Non-hormonal Contraceptive Methods: A Quick Reference Guide for Clinicians. Available at: http://www.arhp.org/files/QRGNonHormonalContraception.pdf. Contraception: Spermicides N-9 (menfegol, benzalkonium chloride, chlorhexidine, sodium dousate) Surfactant that destroys sperm cell membrane in concentrations ranging from 1-18%. Insert no more than 1 hour prior to intercourse. FDA mandates that warnings say this product won’t protect against STDs or HIV May damage vaginal mucosa or cervical epithelium, and can and increase STI vulnerability, and FDA mandates these products warn that these products may increase the risk of getting HIV/AIDS from an infected partner Contraception Condoms Over 100 products available in the US 90% are made of latex Animal skin products or polyurethane make of the rest of the products Most are lubricated Note: anal intercourse doubles risk of breakage Extra thick condoms blunt sensation and reduce premature ejaculation $0.50 for latex, 0.80 for poly, several dollars for designer condoms Spermacide reduces shelf life to 2 years, 5 normally Condoms, counseling Latex are the best protection against STI, including HIV and HSV Apply over an errect penis immediately before intercourse with half-inch reservoir at the tip of the condom should be created by carefully pinching the tip of the condom after placement Withdrawal should occur prior to loss of erection Hold the rim during withdrawal to prevent spillage Only water based lubricants should be used with the latex condoms Putting it on inside out, taking it out, flipping it over and wearing during intercourse. Completely unrolling it before wearing. Removing the condom during intercourse. Putting the condom on after IC has begun. Using too large a condom. Sterilization Contraceptive Cases A 25 year old after delivery wants to know how likely it is she’ll regret it if she has you perform a post partum tubal ligation. A 20 year old G4 P4 says her previous doctor refused to perform her tubal ligation, and she says she’s got insurance from the state now and she wants it done. What do you recommend? A 33 year old wants permanent contraception what technique should you select? A woman wants to know what is her chance of needing a hysterectomy if she gets a tubal? % of Women Using Method Usage of sterilization Female Sterilization Male Sterilization Condom Oral Contraceptive Other Methods Injection 60 50 40 30 20 10 0 15-19 20-24 25-29 30-34 Age Chandra A, et al. Vital Health Stat. 2005;23(25). 35-39 40-44 Advantages of Sterilization Ideal for those desiring no more children Quick recovery Lack of long-term effects Cost-effective No need to remember to use contraception before intercourse No need for partner compliance High degree of safety; low mortality rates Failure rate 0.5 to 3.6% Disadvantages of Sterilization Permanence Reversal is expensive, requires major surgery, and is not guaranteed Regret for the decision Expense at time of procedure Procedure requires aseptic conditions, surgical equipment, trained clinicians, and anesthesia Does not protect against HIV or other sexually Complications Associated With Sterilization 1 to 2 deaths/100,000 women when compared to a maternal mortality rate of 12.1/100,000 live births Procedural complications Excessive bleeding or hemorrhage Infection Anesthesia-related complications Trauma – tears, perforations, and burns to abdominal organs Ectopic pregnancy – but the risk is lower than for nonsterilized women Peterson HB, et al. Am J Obstet Gynecol. 1983;146:131-136 Female Sterilization: Techniques Clips – block the fallopian tubes by clamping down and cutting off the blood supply, thereby causing scarring or fibrosis Filshie clip – titanium with a silicone rubber lining Wolf (Hulka) clip – plastic Rings – cinch a loop of the midportion of the fallopian tube Fallope ring – small Silastic band Microinserts – two concentric expanding metal coils surrounding PET mesh fibers that produce a local inflammatory response Hulka JF, et al. Am J Obstet Gynecol. 1976;125:1039-1043; Yoon IB, et al. Am J Obstet Gynecol. 1977;127:109-112. Hysteroscopic Placement of Permanent Birth Control Micro-Insert Within Tubal Lumen Taken from Kerin, Carignan & Cher. The safety and effectiveness of a new hysteroscopic method for permanent birth control. Aust N Z J Obstet Gynaecol 2001;41:364-370. Regret After Sterilization Years After Sterilization* Characteristic 3 7 14 3.9 7.5 12.7 18-30 5.1 10.5 20.3 >30 2.6 4.8 5.9 No 4.5 9.4 20.4 Yes 3.6 6.8 10.2 White 3.5 6.0 7.4 Black 4.3 10.2 21.7 Postpartum – vaginal 5.6 10.2 17.8 Postpartum – cesarean 8.8 14.0 16.1 15 d-1 yr 3.3 8.8 17.6 2-3 yrs 4.5 8.2 12.6 4-7 yrs 3.4 7.0 9.5 Overall (N=744) Age at sterilization Married Race Time between birth of last child and sterilization Interval * Cumulative probability/100 procedures Hillis SD, et al. Obstet Gynecol. 1999;93:889-895. Surgical Abortion Pregnancy Termination Counseling • Discuss all options regarding pregnancy • Discuss decision-making process • Provide information Offer medical abortion • Review medical history and discuss previous procedures • Referral for long-term counseling • Issues in Elective Termination of Pregnancy • Sonography Need for more comprehensive evaluations Neonatal advances Fetal tissue research Rise in infertility Dearth of adoptive children Advances in assisted reproductive technologies (ART) Selective Termination Rarely medically indicated • • • • • • • • (Contraceptive) Cases A 24 year old with NYHA Class 4 CVD presents because she was told she “has to have an abortion,” do you agree? A 13 year old patient who has never had a pelvic examination presents requesting an abortion under general anesthesia, is this as safe as under local anesthesia? A 28 year old Russian woman presents for her 7th surgical abortion, how do you counsel her? Preoperative Evaluation Targeted History • Pelvic examination Falls within preset dating criteria Adequate cervical visualization and uterine palpation Patient suitable for local anesthesia Rh typing Hemoglobin Sonography GC/CT testing Review counseling session and the contraceptive alternatives Vacuum Aspiration Complications • Inability to dilate cervix • Severe postoperative pain Endomyometritis Salpingitis Uterine subinvolution • No tissue or villi obtained • Obvious uterine perforation • Immediate hemorrhage Cervical Uterine • • • • Pregnancy continues Ectopic gestation Molar pregnancy Ovarian cyst pathology Medical Abortion Abortion performed without primary surgical intervention Rachel Benson Gold discusses a particularly troubling aspect of state laws in “The Implications of Defining When a Woman is Pregnant,” which appears in the same issue of TGR. According to both the scientific community and long-standing federal policy, a pregnancy is established when a fertilized egg has implanted in the wall of a woman’s uterus. However, definitions of pregnancy in state law vary widely. And although they have not yet been used to impede women’s access to legal hormonal contraceptive methods, such restrictions are a goal of at least some antiabortion and anticontraception activists. To date, 22 states have enacted one or more laws that include a definition of “pregnancy.” The definitions found in 18 of these laws are based on the idea that pregnancy begins at fertilization or conception. The ongoing debate around emergency contraception–a concentrated dosage of the same hormones found in birth control pills–has brought the question of when pregnancy prevention ends and disruption of an existing pregnancy begins to the forefront of public discussion. Attempts to define pregnancy as beginning before implantation could have serious implications for women’s access to both emergency contraceptives and other hormonal contraceptive methods. “The fact is the majority of Americans have sex before marriage; virtually all U.S. women (98%) use a contraceptive method at some point in their lives; and most women rely on contraception, not abstinence, to help them responsibly manage their sexual lives in the long term,” says Dailard. “As long as politicians continue to ignore the realities of women’s lives, the United States will continue to have the highest rates of unintended pregnancy and abortion in the developed world–a dubious honor that most Americans would prefer not to have.” (Contraceptive) Case A 21 year old patient presents for an abortion but she doesn’t have a positive pregnancy test, she wants a medical abortion, what do you give her? Medical Abortion Regimens Prostaglandin Mifepristone + Antiprogesterone Misoprostol Antimetabolite Methotrexate + Misoprostol Medical Abortion Advantages Can be performed without delay Avoids surgical and anesthetic risk Potential to increase access through expanding providers (not true) Potential to shield abortion providers (also not true) Increases choice Medical Abortion Disadvantages Longer waiting period for completion Requires multiple visits (2-3) Less effective than surgical (95% vs 99%) Not available after about 7 weeks Expense (Cumbersome) regimen Surgical Abortion Advantages More effective Shorter time to completion Fewer visits Shorter bleeding duration Always has pathologic confirmation Can be performed in later gestation Surgical Abortion Disadvantages More serious risks involved Limited access Requires more equipment and investment Providers more vulnerable to risk Medical Abortion Counseling Desires termination of pregnancy Usual method and efficacy of alternatives Risks, side effects, tetarogenicity and adverse events for each medication and for failed medical Informed consent and administer the MifeprexTM Medication Guide and Patient Agreement Medical ascertainment of contraindications to the medications Clarify the amount of pain and the number of visits and the possibility of need for outside medical care at own expense Mifepristone: Mechanism Softens and dilates the cervix Causes decidual necrosis by affecting the capillary endothelial cells of the decidua and detachment of pregnancy Increases prostaglandin release Increases uterine contractions and sensitivity to exogenous prostaglandin Mifepristone + Misoprostol Medical history and physical exam Pregnancy dating (HCG titers if no sac) Rh status and administration of Rhogam Hematocrit or hemoglobin Counseling/informed consent Offer surgical abortion Explain 4 hour waiting requirements of visit 2? FDA wanted both drugs administered in the office Explain only placenta and blood will be visible to the naked eye Mifepristone + Misoprostol Administer mifepristone 200 mg Schedule the next visit The literature supports home administration safety for the misoprostol, the FDA is not supportive Instructions on self care and how to contact the clinic Provision of emergency contact, verbal and written use instruction Mifepristone + Misoprostol Confirm with sonography patient has not aborted (no decisive HCG change for 10d) 6% complete abortion prior to misoprostol If not completed abortion administer misoprostol 400 mcg PO in two 200 mcg tablets (800 PV, done but not licensed in any country) (Observe for 4 hours about 50% will abort) 84% abort within the next 24 hours Monitor patient for home administration Pain medication for cramping and medication for GI symptoms Mifepristone + Misoprostol Return in 7-10 days to confirm abortion by sonography Vaginal bleeding lasts for 17 +/-11 days and tapers off rapidly after initial expulsion, tell patients to expect 9-20 days of bleeding 8-9% of women have bleeding >30 days Pathologic confirmation: decide about tissue disposal if patient should bring the tissue with her Medical Abortion Overview “Expected” side effects “Expected” bleeding “Expected” cramping Medication requirements Hospitalization rates “Expected” Side Effects GI: Nausea, Vomiting, Diarrhea Mild temperature elevation (PD effect) Cramping Headache, dizziness Bleeding “Expected” Bleeding Bleeding-moderate to heavy Some clots-small to large Onset average 2-4 hours after misoprostol Heaviest bleeding may last 1-4 hours as pregnancy is expelled Contact us if 2 maxipads/hour for 2 hours: call (pads should be ‘dripping wet’) “Expected” Cramping Cramps are light to heavy Pain usually managed with ibuprofen 600-800 mg/4-6 hours Prescription for acetaminophen with codeine may be given on day 1 or day 3 Night cramping usually worse before expulsion Ultrasonography Ultrasonography Diagnosis of Complete Abortion Any abortion without suction curettage must have a confirmatory examination before the patient’s treatment course is complete Ultrasound disappearance of the gestational sac this usually mandates a transvaginal ultrasound Negative pregnancy test (<50 mIU/ml in urine) 90% drop in b-HCG Management of Complications Pain: May assess on an Likart scale Temperature: returns to normal 3-4 hours after misoprostol Failure to bleed: Do not treat EP with this regimen Heavy or prolonged bleeding: stops 1-2 hrs after passing pregnancy Rest, heating pads, NSAID or non-ASA Plenty of non-alcoholic beverages Clinician should call back 30-60 minutes to assess the patient’s condition Completion may take up to 3-4 weeks Return visits are the only way to assure completion 80-85% will abort within two weeks with Mtx-Misoprostol and 9597% within two weeks with RU486-Misoprostol Complication Rates Surgical abortion: 9/100,000 overall with mortality <1/100,000 Most surgical complications result from instrumentation in the uterus and from second trimester procedures Medical abortion: complications are more difficult to assess: bleeding is expected, it can be heavy, hemorrhage is a complication US Trial 1/859 Tx adverse event rate of 0.17% Specific AEs From Medical Abortions of first 80,000 5 EP, one of which was fatal 13 transfusions (one was EP case) 117 had curettages, nearly all were non-emergent 10 received antibiotics for presumed infection 6 had allergic reactions 50 women had ongoing pregnancies, of which all but two terminated surgically Conclusions Conclusions Contraception is good primary prevention of disease Perceptions of safety and convenience Provider Education Reducing mythology Increasing knowledge of noncontraceptive benefits Many methods available but cost and access seem to still limit their use and increase risk of unplanned pregnancy Most women will use many methods Abortion should be safe, legal and rare “We have not inherited the earth from our grandparents, we have borrowed it from our grandchildren.” ---attributed to Ancient Chinese