The Fundamentals of Quality Improvement
advertisement
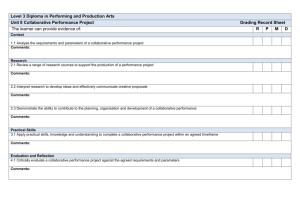
Quality Improvement Principles, Methods and Tools Marlene “Marni” Mason MCPP Healthcare Consulting Marni Mason BSN, MBA Thirty+ years in healthcare as clinician, manager and consultant Primary & specialty care clinic nurse and nursing director – 15 years Consultant in healthcare performance measurement and improvement – 18 years Public health performance management – since 2000 Surveyor for NCQA (10 years) and Senior Examiner for state Baldrige Quality Award (late 1990s) Consultant for PHAB Standards Development (20082009) 2 Learning Objectives In today’s learning session, the participants will develop a better understanding of: Principles of Quality Improvement Selected Quality Improvement Methods Selected Quality Planning Tools Learn about Rapid Cycle Improvement (RCI) And Start development of QI team AIM statement 3 Collaborative with a Capital “C” Systems are perfectly designed to produce the results they achieve 4 IHI’s* Breakthrough Series Also known as the Collaborative Method It is an improvement method that relies on spread and adaptation of existing knowledge to multiple settings to accomplish a common aim Methodology to accomplish organizational system change *Institute for Healthcare Improvement www.ihi.org 5 The Advantage of a Learning Collaborative for Improvement Learning collaborative: a group of multidisciplinary teams from multiple organizations which come together over the course of a year in structured meetings and phone contacts to accomplish specific learning objectives. National experience demonstrates significant boost in pace and level of achievement of outcomes by sharing lessons learned. 6 Collaborative Process (IHI) Participants Select Topic Planning Group Prework Identify Change Concepts P A P D A S LS 1 P D A S LS 2 D S LS 3 Outcomes Congress Supports E-mail Visits Web-site Phone Assessments Senior Leader Reports 7 Characteristics of a Collaborative Team approach Performance measures Teams from multiple organizations One for all, all for one Promotes a culture of change Standardizes practice Sustainable change 8 MLC-3 Collaborative Targets In Illinois, participation in the MLC-3 Learning Collaborative is focused on improvement in two target areas for MLC-3: Community Health Improvement Plans Chronic Disease Prevention-Obesity/Physical Activity (reduce preventable risk factors that predispose to chronic disease) 9 MLC-3 Collaborative Approach All sites receive training in: Quality Improvement Methods & Tools Data Analysis Tools Rapid Cycle Improvement Method Site-based teams develop implementation plan for improvement Series of web-based phone sessions with coaching from consultant 10 Principles of Quality Improvement “Quality is never an accident; it is always the result of high intention, sincere effort, intelligent direction and skillful execution; it represents the wise choice of many alternatives.” William Foster (many variations attributed to others) 11 Performance Management Source: Turning Point Performance Management Collaborative, 2003. 12 The Quality Environment Do you have an organization-wide commitment to assessing and continuously improving quality over time? Are your system decisions based on data? Do you know if your agency is achieving its goals? Do you use data to decide on improvement initiatives and to know if the improvements are successful? 13 Change vs. Improvement W. Edwards Deming stated “Of all changes I’ve observed, about 5% were improvements, the rest, at best, were illusions of progress.” We must become masters of improvement We must learn how to improve rapidly We must learn to discern the difference between improvement and illusions of progress 14 Principles of Quality Management 1. 2. 3. 4. 5. 6. 7. Know your stakeholders and what they need Focus on processes Use data for making decisions Understand variation in processes Use teamwork to improve work Make quality improvement continuous Demonstrate leadership commitment 15 1. Know Your Stakeholders Identify stakeholders and their needs Set goals based on stakeholder needs Monitor performance and satisfaction to target performance improvement opportunities Improve or redesign how work is done 16 Sector Maps for Planning – Example of Public Sector Health & Human Services •Center for Disease Control & Prev. •Center-Medicaid &Medicare Srvcs •Fed. Drug •Administration Dept. of Social & Human Services Office of the Insurance Commissioner Governor / Legislature Employment Security Department Department of Health •Community & Family Health •Women, Infants & Children •Licensing Boards Tribal Government Health Care Authority School Boards •Public Schools (K-12) •Private Schools (K-12) Local Health Jurisdictions Rural & Community Health Centers Local Government Public Library System Indian Health Service State Board of Health Bullets refer to examples of organizations and are not a comprehensive listing. 17 Example of Private Sector Consulting Foundations Professional Organizations Purchasers Hospitals Home Health Care Funding Foundations Pharmaceutical Companies •Rob’t Wood Johnson Health Plans Providers Business and worksite programs SNF and Nursing Homes Insurance Brokers Primary/Specialty Medical Groups Ancillary Service Practitioners and Groups Media Bullets refer to examples of organizations and are not a comprehensive listing. 18 Example of CommunityBased Sector Service Organizations •Thousands of community-based agencies: specific partners will be identified in each community Communities of Color Organizations United Way Senior Centers Faith-based Community Organizations Community Centers Youth Associations •YMCA / YWCA •Boys & Girls Club •Boy & Girl Scouts of America •Campfire Girls and Boys American Association of Retired Persons Community Health Alliances Youth Sports Associations Churches, Temples & Mosques •Little League •Pop Warner •Soccer, etc Community Health Centers •Federally Qualified Health Centers •Migrant Health Centers Community-based Daycare Sites •All ages •Birth to 3 childcare Bullets refer to examples of organizations and is not a comprehensive listing. 19 Example of Academic/Research Sector State Universities Tribal Colleges Community Colleges Private Universities Allied Health Professional Schools & Training Nursing Schools Private Research Centers\ Pharmacy Schools Bullets refer to examples of organizations and is not a comprehensive listing. 20 Example of Target Populations CONDITION Diagnosed Public: Private: Community: Academic: Age Racial/ethnic Communities Socio-economic/low literacy General Population Center for Medicaid & Medicare Services (CMS) DOH -- CDRRP/DPCP Public Hospital Districts Tribal Associations Veteran’s Admin. Dept. of Defense Medicaid Qualis Health Health plans Media Inland NW Business Coal. Alternative health providers Home health Student health centers DOH-Chronic Disease Risk Reduction (CDRRP) DOH- Diabetes Prevention & Control Program (DPCP) Tribal Assns. Indian Health Services DOH-Chronic Disease Risk Reduction (CDRRP) DOH- Diabetes Prevention & Control Program (DPCP) Dept. of Veterans Affairs Maternal Support Services Community Health Plans of WA – (CHPW) Association of Black Health Care Professionals Association of American Indian Physicians “Move It” program Amer. Diabetes Assoc. Juvenile Diabetes Research Foundation (JDRF) Senior centers Service organizations Community Aging Service Providers WSU Extension Focused research programs, e.g. SEARCH for Diabetes in Youth Communities of color organizations Amer. Diabetes Assoc. (ADA) CHOICE Health Commu. Health Centers (CHCs) WSU Extension Focused research programs, e.g. SEARCH for Diabetes in Youth Molina health plan Community Health Plans of WA (CHPW) Disease management vendors Critical access hospitals Home Health Washington Health Foundation CHOICE Health Commu. Health Centers (CHCs) Centers for Disease Control & Prevention (CDC) Office of Insurance Governor/Legislature Dept. of Corrections Public Employees Benefit Board Local Health Jurisdictions Professional orgs Pharmaceutical. Co Medical Supply Co. Purchasers Disease mgt Hospitals Critical access hospitals Primary/specialty groups WA StateUniv. Extension Commu. Health Centers Amer. Diabetes Assoc. (ADA) Nutrition & Cultures Disease Management Education Centers Allied health training UW Med school Bastyr University Nursing Schools Private Universities Pharmacology Schools Community Colleges Tribal Colleges 21 2. Focus on Processes 85% of poor quality is a result of poor work processes, not of staff doing a bad job Processes often “go wrong” at the point of the “handoff” Attend to improving the overall process, not just one part—some of the most complex processes are the result of creating a “work around” 22 Focus on Processes Advice from NCQA, JCAHO and others— measure processes that are High-risk High-volume Problem-prone And Can be tracked and reported as summary or aggregate statistics 23 Develop Process Flow Charts High level flow charts [6-12 steps] initially Identify customer-supplier relationships More detailed flow charts as project unfolds [client flow, information flow, materials flow, decision making flow] Use for process redesign Use for adapting or adopting best practices 24 We inspect restaurants So that # of inspections Conditions in the restaurant don’t create unsafe food So that # of critical violations Public is sold food that is safe to eat The Logic of Public Health % of critical violations corrected within 24 hours So that There are fewer incidents of foodborne illness rate of foodborne illness 25 Logic Models (Many Shapes/Sizes) Connect what we do every day to why we do it Show logical links between activities and goals Link our process objectives to our outcome objectives As long as the format is legible, logical, and it works for you, it’s probably fine Boxes and arrows are not required New computer software is not required 26 Logic Model: Any Public Health Program Inputs Resources Money Staff Outputs Short Term Outcomes Intermediate Outcomes Long Term Outcomes Activities Program Development Program Planning Materials Development, Distribution Informed, Targeted Program Appropriate, Targeted Materials Reduced Morbidity Improved knowledge, beliefs, attitudes Improved Behaviors Reduced Mortality Improved Quality of Life 27 28 3. Use Data to Make Decisions Use performance assessment data to target improvement Use data analysis tools to develop information Analyze data to identify root cause Use data to monitor performance outcomes 29 Use Data to Make Decisions Conceptual Tools Affinity Diagram Brainstorming Process Flow Chart Interrelational Diagraph Matrix Diagram Tree Diagram Cause and Effect Diagram Numerical Tools Check Sheet Bar Chart Histogram Pareto Chart Control Chart Run Chart [See Goal/QPC PH Memory Joggers] 30 Use Data to Make Decisions Brainstorming for root causes—theory generation relies on divergent thinking, no idea is a bad one… What can go wrong in the process we are studying? Problems in hand-offs between steps Problems in execution within steps Look at machines, materials, methods, measurements, and people 31 Cause-effect or Fishbone Diagram Exercise: Constructing a Fishbone Diagram Organizes and displays theories Encourages divergent thinking Demonstrates the complexity of the problem Encourages scientific analysis (rule-out) Turn to page 23 in the PH Memory Jogger. 32 4. Understand Variation Sources of variation include: machines, materials, methods, measurements, people, environment Common cause variation occurs if the process is stable—variation in data points will be random and obey a mathematical law—it is said to be in statistical control, with a large number of small sources of variation Reacting to random variation in a process that is stable/in statistical control, it is called tampering and leads to further complexity, increasing variation and mistakes 33 Understand Variation Special cause variation arises because of specific circumstances which are not part of the process all the time and may or may not ever recur—if the recurrence is periodic, clues to the root cause may emerge Variation can be shown in control charts with mean and standard deviation Control charts are pictures of trend data with an extra feature—the range of variation built into the system 34 Understand Variation A sentinel event is a special cause variation requiring root cause analysis Examine specific incident(s) of special cause variation and make changes to a single element only after very careful analysis Need to investigate special cause variation before making any conclusions about performance level Failure to distinguish between common and special cause variation can be hazardous to organizational performance! 35 Variation Exercise Joiner Associates – Hunter Conference exercise Attributed to Brian Joiner’s 9 year-old son 36 5. Use Teamwork QI efforts need buy-in from all stakeholders Creative ideas are needed Division of labor is needed Process often crosses functions Solution generally affects many 37 Use Teamwork Teams should develop a clear charge and support resources Teams should adopt working agreements (cell phone etiquette to decision procedures) Teams should assign roles of facilitators and recorders Team process has predictable stages that are useful to keep in mind: Forming, Storming, Norming, Performing 38 Example of Alignment Wheel Public Health and Partners Aligned with the 10 Essential Services ES 10: Research Goal Statement ES 9: Evaluate ES 1: M onitor Health Status Pharm. Co., N.I.H. ES 2: Diagnose LHJs and Investigate CDC FQHC, Qualis , Health U.W., V.A DSHS / MAA WADE ES 8: Assure a U.W. Competent Workforce Pharm W.S.U . Goal Statement Health Plans ES 7: Link People to Needed Services LHJs Health Care DM Ed Center PH Program DSHS / MAA OIC, Legislature, Govern ES 6: Enforce Laws and Regulations Goal Statement HH S ADA , WADEES 3: Inform, Educate Pharm.and Empower Assoc Qualis FQHC Faith-based, Goal Schools, Educ. Assoc. Statement Profession (AARP etc), ES 4: M obilize al Assoc., Community OIC, Partnerships Feds, ES 5: Develop Policies and Plans 39 6. Make QI Continuous QI is a system-wide approach to assessing and continuously improving quality of the processes and services over time See inter-relationships, not parts Understand the flow of work, not the one-time snapshot Detail the work processes Determine cause and effect relationships Identify points of highest leverage Improve and innovate, not just change for change’s sake 40 PDCA/PDSA Cycle definition The Plan Do Check/Study Act Cycle is a trialand-learning method to discover what is an effective and efficient way to design or change a process The “check” part of the cycle may require some clarification; after all, we are used to planning, doing/acting. It compels the team to learn from the data collected, its effects on other parts of the system, and under different conditions, such as different communities 41 Act • What changes are to be made? The PDSA Cycle for Learning and Improvement • Next cycle? Study • Complete the analysis of the data • Compare data to predictions • Summarize what was learned Plan • Objective • Questions and predictions (why) • Plan to carry out the cycle (who, what, where, when) • Plan for data collection Do • Carry out the plan • Document problems and unexpected observations • Begin analysis of the data 42 Ongoing PDSA Cycles PLAN PLAN PLAN Target Improvements Accreditation Accreditation ACT Areas for Improvement DO Evaluate CHECK Report/Recommend Self-Assessment or Accreditation DO ACT Improvement work Recommend Improvement ACT DO Areas for Improvement Evaluate CHECK CHECK Study Improvement Results Report/Recommend Performance Improvement Cycle Self-Assessment or Accreditation 43 Make QI Continuous Use assessment to identify areas for improvement Charge QI team and provide support Provide QI training Use tools to understand root causes Use data for baseline and analysis Design process improvement to address root causes Train…train…train… staff on the newly designed process improvement 44 Adopt or Adapt Model Practices Use data to identify need for improvement Identify exemplary practices in: other local departments, Michigan state programs and other states, CDC and other national organizations, www.naccho.org/topics/modelpractices other industries Describe your process (Logic Model) Study the exemplary practice process Adopt or adapt as appropriate 45 7. Demonstrate Leadership Commitment Build a QI culture Connect the organization’s strategic plan to performance improvement Know and use quality principles Encourage all staff to use quality improvement in daily work Reward improvements Assure adequate QI infrastructure for quality assessment and improvement activities 46 What questions do you have? 47 Rapid Cycle Improvement (RCI) and PDSA Cycles 48 Why do we need a systematic model for improvement? “All improvements require change but not all change will result in improvement. A primary aim of the science of improvement is to increase the chance that a change will actually result in sustained improvement from the viewpoint of those affected by the change.” --The Improvement Guide, 1996 49 Rapid Cycle Improvement Model for Improvement The idea behind rapid cycle improvement is to first try a change idea on a small scale to see how it works, and then modify it and try it again until it works very well for staff and customers. Then, and only then, does a change become a permanent improvement. What are we trying to ac c omplish? How will we know that a c hange is an improvement? Ac t Study Plan Do 50 Testing a Change: Why Test? Low Confidence in success -Smaller Scale Tests -More of them prior to implementation High Minor Level of risk Major 51 Modified from Jane Taylor PhD Testing a Change: Why Test? Minimize risks of potential failure and of potential adverse or unanticipated side effects Predict how much improvement can be expected from the change Learn how to adapt the change to conditions in the local environment Evaluate costs and side-effects of the change Minimize resistance to implementation 52 Rapid Cycle Improvement Mod el for Im p rovem ent What are we trying to ac c om plish? How will we know that a c hange is an im provem ent? Ac t Stud y Pla n Do 53 What Are We Trying to Accomplish? The first question is meant to establish an aim for improvement that focuses group effort. Aims should be as concise as possible – sometimes it takes a few trials of testing an aim before it becomes truly focused Focus on what matters to the organization, staff and patients Use numerical goals wherever possible Guidance and resources (e.g. tools to be used, methods and systems to be changed) 54 How Will We Know That a Change is an Improvement? Measures and definitions are necessary to answer this question. Data is needed to evaluate and understand the impact of changes designed to meet an aim. When shared aims and data are used, learning is further enhanced because it can be shared. In this way, superior performance and best practices are more quickly identified and disseminated through benchmarking. 55 What Change Can We Make that Will Result in an Improvement? This step is also known as “How will we get there?” Formulate change concepts that may improve the process outcomes This is the who, what, when, and how of doing the actual test It compels the team to learn from the data collected, its effects on other parts of the system, and under different conditions 56 Consolidation of Relevant Knowledge and Experience Develop a set of change concepts Definition of Change Concepts - Ideas for interventions and actions for improvement with a greater likelihood of working based on evidence, quantitatively documented experience, and/or internal data. 57 Some Sources for Improvement Interventions and Actions Published literature in scientific journals Documented (with data) experience from other public health agencies Internal qualitative analysis of work processes Internal quantitative analysis of work processes Use qualitative analysis tools (e.g. fishbone diagrams, root cause concepts) to identify barriers e.g. Pareto analysis National experts (e.g. IHI, NACCHO, PHF, ASQ, Goal/QPC, MLC states and many others) 58 Sequential Building of Knowledge Includes a Wide Range of Conditions in the Sequence of Tests A P S D Breakthrough Results A P S D A P S D Theories, hunches, & best practices A S P D Spread Implement Test new conditions Test a wider group Test on a small scale 59 Sequential Testing….when do you move to implementation? After each PDSA… Implement as is Abandon it Increase in scope e.g. more clients, more programs Modify it and test again Test under different conditions 60 Testing Done in Multiple Change Areas in Parallel A P A P RCI Team #4 Or 4th Change S D A P S D Change RCI Team #1 Or 1st Change A P S D S D S D S D S D A P S D S D A P S D S D A P A P S D A P A P 3rd A P A P A P RCI Team #2 or 2nd Change S D S D A P RCI Team #3 or A P A P A P S D A P S D A P A P S D S D Aims: Productivity Quality Coordination Access S D S D 61 Testing a Change Testing – Trying and adapting existing knowledge on small scale. Learning what works in your system Testing is not permanent Often we have more failures than successes Test on a small scale over a short period of time Have experts comment on feasibility Anticipate a sequence of tests on one change idea 62 Testing a Change: Tips Move from ideas to action quickly Decrease the scope of the test Test of oneness One stakeholder, one program, one day As you are designing the test, ask ‘What design would enable us to do this test now, tomorrow or next week 63 Implementing a Change Implementation – Making this change a part of the day-to-day operation of the system Implement a change ONLY if it will lead to improvement Involves more people and conditions: you will run into more resistance and factors which require “design tweaks” 64 What Can We Do Now… … by Next Week, …by Tuesday, …by Tomorrow …that we can learn from without harming clients or burdening staff? Modified from Jane Taylor PhD 65 Rapid Cycle Improvement–Example 66 What are We Trying to Accomplish? Increase accurate and complete reporting of CD to 80% or more of all reports by 10/07, and more than 95% by 2/08 with clear definition of complete reports. We do this in order to provide valid data for planning and program improvement 67 How Will We Know When We Get There?: Measurements Increase (trended) in percent of accurately completed CD reports Decrease in staff time to input incomplete information Trend in overall measures in right direction (direction of goodness indicated by arrow) Other CD reporting measures Other process measures 68 What Changes Can We Make? Data analysis of reasons for incomplete reports. Identify reasons with definitions Assure that database can capture each reason Initiate data collection process Train staff and providers in definition and reporting process Address lack of knowledge of providers Create plan to identify high volume providers and target for extra training 69 RCI Team Planning Tool PROJECT: REDUCE PERCENT OF STAFF CANCELLATIONS (10-3-06) Aim: Reduce staff cancellations of patient appointments to 5% or less by Dec 2006 and less than 2% by March 2007 with clear definitions of types of appointments considered staff cancellations.We do this in order to provide high quality, accessible services to our clients. Measures 1. Trend of staff cancellations in right direction. 2. Assess actual increase in productivity (measured by hours of direct service) that occur as a result of reducing the percent of 3. Trend in overall measures in right direction (e.g. hospitalizations, staff and patient satisfaction) Cycle Number 1 Change Tested Person(s) Responsible 1a Data on staff cancellations to determine reasons (Pareto analysis Identify reasons for staff cancellations Beth T., Margaret 1b Establish definitions of staff cancellations Bernie & Med Prov 1c Train staff and providers in definitions Donna, Beth T. 1d Pilot test in all provider practices for 7 weeks Beth, Margaret 10/9- 11/24 WEEK. (1 = Sept 5) 1 2 3 4 (9/4) 5 (10/2) 6 7 8 9 10 11 (11/6) 12 13 (11/28) 70 Data Analysis- Pareto Chart Non-Reporting Facilities by School Type 100 100.0% 90 90.0% 80 80.0% 70 70.0% 60 60.0% 50 50.0% 40 40.0% 30 30.0% 20 20.0% 10 10.0% 0 0.0% CHILDCARE/PRESCHOOL Total PUBLIC Total PRIVATE Total CHARTER Total 71 8 7 5 4 4 4 3 3 3 3 2 2 1 1 1 1 1 G IS D 8 AT 10 C LI O H ER TO B N EE C H E R BE N TL E FE Y N TO N DA VI S O LA KE N W V IL E LE ST W L IN O O D D EN H E LA IG HT K E FE S N TO M T N M O R R IS B EN D LE FL U SH IN G O G O D R IC KE H A RS L M EY O N TR O SE G E NE S EE G C FL AR R A IN N M EN D B T LA -A IN N SW SW C AR OR TH TZ C R EE K Data Analysis- Pareto Chart 70 Non-Reporting Schools By District 100.0% 62 60 90.0% 80.0% 50 70.0% 40 60.0% 50.0% 30 40.0% 20 30.0% 11 20.0% 10.0% 0 0 0 0.0% 72 Results – Error Rate 73 Results – Time Study 74 Steps to Set Up a Rapid Cycle Improvement Establish a multi-disciplinary RCI team Identify a positive opinion leader Align leadership and administrative support Consolidation of relevant knowledge and experience (national) for multiple changes Development of an overall aim statement (using the three questions at a high level) Decide where to start and develop a strategy for a series of rapid cycles. 75 Guidance on Following the Steps It is important not to try to write the perfect AIM statement and develop the most thorough rapid cycle strategy at the start. It is more important to start small, rapid tests of change through PDSA cycles as soon as possible. The AIM statement and strategy evolve continually as you learn from testing. The major objective is to build organizational learning from small tests of change. 76 Key Lessons from RCI The rapid improvement work must be seen as The Work and not a separate project Implementation and holding the gains requires integration into daily work and meetings Start work with those interested in change Communicate what is happening persistently Provide support to providers and staff who take on this new work 77 What questions do you have? 78