Traumatic Brain Injury and Psychogenic Nonepileptic Seizures
advertisement
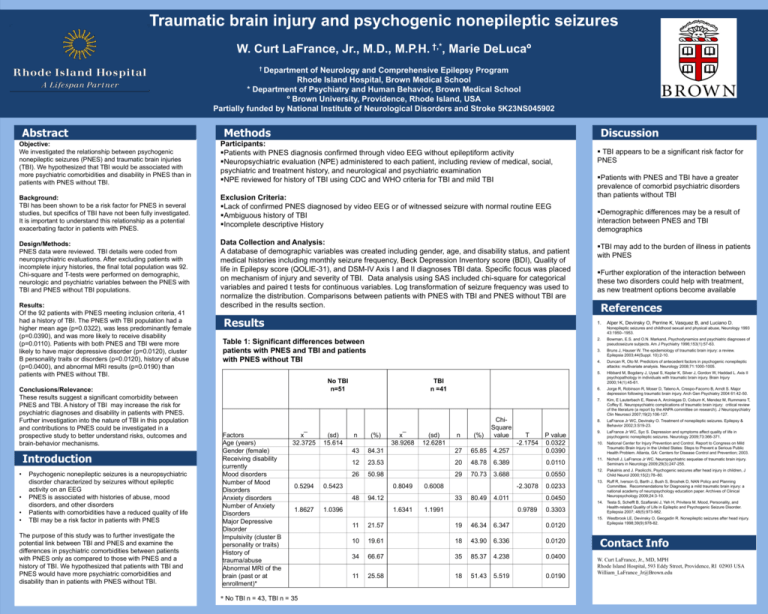
Traumatic brain injury and psychogenic nonepileptic seizures W. Curt LaFrance, Jr., M.D., M.P.H. †,*, Marie DeLucaº † Department of Neurology and Comprehensive Epilepsy Program Rhode Island Hospital, Brown Medical School * Department of Psychiatry and Human Behavior, Brown Medical School º Brown University, Providence, Rhode Island, USA Partially funded by National Institute of Neurological Disorders and Stroke 5K23NS045902 Abstract Methods Discussion Objective: We investigated the relationship between psychogenic nonepileptic seizures (PNES) and traumatic brain injuries (TBI). We hypothesized that TBI would be associated with more psychiatric comorbidities and disability in PNES than in patients with PNES without TBI. Participants: Patients with PNES diagnosis confirmed through video EEG without epileptiform activity Neuropsychiatric evaluation (NPE) administered to each patient, including review of medical, social, psychiatric and treatment history, and neurological and psychiatric examination NPE reviewed for history of TBI using CDC and WHO criteria for TBI and mild TBI Background: TBI has been shown to be a risk factor for PNES in several studies, but specifics of TBI have not been fully investigated. It is important to understand this relationship as a potential exacerbating factor in patients with PNES. Exclusion Criteria: Lack of confirmed PNES diagnosed by video EEG or of witnessed seizure with normal routine EEG Ambiguous history of TBI Incomplete descriptive History Design/Methods: PNES data were reviewed. TBI details were coded from neuropsychiatric evaluations. After excluding patients with incomplete injury histories, the final total population was 92. Chi-square and T-tests were performed on demographic, neurologic and psychiatric variables between the PNES with TBI and PNES without TBI populations. Data Collection and Analysis: A database of demographic variables was created including gender, age, and disability status, and patient medical histories including monthly seizure frequency, Beck Depression Inventory score (BDI), Quality of life in Epilepsy score (QOLIE-31), and DSM-IV Axis I and II diagnoses TBI data. Specific focus was placed on mechanism of injury and severity of TBI. Data analysis using SAS included chi-square for categorical variables and paired t tests for continuous variables. Log transformation of seizure frequency was used to normalize the distribution. Comparisons between patients with PNES with TBI and PNES without TBI are described in the results section. Results: Of the 92 patients with PNES meeting inclusion criteria, 41 had a history of TBI. The PNES with TBI population had a higher mean age (p=0.0322), was less predominantly female (p=0.0390), and was more likely to receive disability (p=0.0110). Patients with both PNES and TBI were more likely to have major depressive disorder (p=0.0120), cluster B personality traits or disorders (p=0.0120), history of abuse (p=0.0400), and abnormal MRI results (p=0.0190) than patients with PNES without TBI. Conclusions/Relevance: These results suggest a significant comorbidity between PNES and TBI. A history of TBI may increase the risk for psychiatric diagnoses and disability in patients with PNES. Further investigation into the nature of TBI in this population and contributions to PNES could be investigated in a prospective study to better understand risks, outcomes and brain-behavior mechanisms. Introduction • • • • Psychogenic nonepileptic seizures is a neuropsychiatric disorder characterized by seizures without epileptic activity on an EEG PNES is associated with histories of abuse, mood disorders, and other disorders Patients with comorbidities have a reduced quality of life TBI may be a risk factor in patients with PNES The purpose of this study was to further investigate the potential link between TBI and PNES and examine the differences in psychiatric comorbidities between patients with PNES only as compared to those with PNES and a history of TBI. We hypothesized that patients with TBI and PNES would have more psychiatric comorbidities and disability than in patients with PNES without TBI. Results Patients with PNES and TBI have a greater prevalence of comorbid psychiatric disorders than patients without TBI Demographic differences may be a result of interaction between PNES and TBI demographics TBI may add to the burden of illness in patients with PNES Further exploration of the interaction between these two disorders could help with treatment, as new treatment options become available References 1. Alper K, Devinsky O, Perrine K, Vasquez B, and Luciano D. Nonepileptic seizures and childhood sexual and physical abuse, Neurology 1993 43:1950–1953. Table 1: Significant differences between patients with PNES and TBI and patients with PNES without TBI No TBI n=51 Factors Age (years) Gender (female) Receiving disability currently Mood disorders Number of Mood Disorders Anxiety disorders Number of Anxiety Disorders Major Depressive Disorder Impulsivity (cluster B personality or traits) History of trauma/abuse Abnormal MRI of the brain (past or at enrollment)* TBI appears to be a significant risk factor for PNES x¯ 32.3725 (sd) 15.614 TBI n =41 n 43 84.31 27 65.85 4.257 P value 0.0322 0.0390 12 23.53 20 48.78 6.389 0.0110 26 0.5294 * No TBI n = 43, TBI n = 35 x¯ 38.9268 (sd) 12.6281 50.98 0.5423 70.73 T -2.1754 3.688 0.0550 -2.3078 33 1.6341 (%) 0.6008 94.12 1.0396 n 29 0.8049 48 1.8627 (%) ChiSquare value 80.49 4.011 1.1991 0.0233 0.0450 0.9789 2. Bowman, E.S. and O.N. Markand, Psychodynamics and psychiatric diagnoses of pseudoseizure subjects. Am J Psychiatry 1996;153(1):57-63. 3. Bruns J, Hauser W. The epidemiology of traumatic brain injury: a review. Epilepsia 2003;44(Suppl. 10):2-10. 4. Duncan R, Oto M. Predictors of antecedent factors in psychogenic nonepileptic attacks: multivariate analysis. Neurology 2008;71:1000-1005. 5. Hibbard M, Bogdany J, Uysal S, Keplar K, Silver J, Gordon W, Haddad L. Axis II psychopathology in individuals with traumatic brain injury. Brain Injury 2000;14(1):45-61. 6. Jorge R, Robinson R, Moser D, Tateno A, Crespo-Facorro B, Arndt S. Major depression following traumatic brain injury. Arch Gen Psychiatry 2004 61:42-50. 7. Kim, E Lauterbach E, Reeve A, Arciniegas D, Coburn K, Mendez M, Rummans T, Coffey E. Neuropsychiatric complications of traumatic brain injury: critical review of the literature (a report by the ANPA committee on research). J Neuropsychiatry Clin Neurosci 2007;19(2):106-127. 8. LaFrance Jr WC, Devinsky O. Treatment of nonepileptic seizures. Epilepsy & Behavior 2002;3:S19-23. 9. LaFrance Jr WC, Syc S. Depression and symptoms affect quality of life in psychogenic nonepileptic seizures. Neurology 2009;73:366-371. 10. National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention; 2003. 11. Nicholl J, LaFrance Jr WC. Neuropsychiatric sequelae of traumatic brain injury. Seminars in Neurology 2009;29(3):247-255. 12. Pakalnis and J. Paolicchi, Psychogenic seizures after head injury in children, J Child Neurol 2000;15(2):78–80. 13. Ruff R, Iverson G, Barth J, Bush S, Broshek D, NAN Policy and Planning Committee. Recommendations for Diagnosing a mild traumatic brain injury: a national academy of neuropsychology education paper. Archives of Clinical Neuropsychology 2009;24:3-10. 14. Testa S, Schefft B, Szaflarski J, Yeh H, Privitera M. Mood, Personality, and Health-related Quality of Life in Epileptic and Psychogenic Seizure Disorder. Epilepsia 2007; 48(5):973-982. 15. Westbrook LE, Devinsky O, Geogadin R. Nonepileptic seizures after head injury. Epilepsia 1998;39(9):978-82. 0.3303 11 21.57 19 46.34 6.347 0.0120 10 19.61 18 43.90 6.336 0.0120 34 66.67 35 85.37 4.238 0.0400 11 25.58 18 51.43 5.519 0.0190 Contact Info W. Curt LaFrance, Jr., MD, MPH Rhode Island Hospital, 593 Eddy Street, Providence, RI 02903 USA William_LaFrance_Jr@Brown.edu