Health Innovations
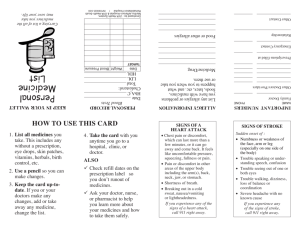
advertisement
FREE ESSENTIAL GENERIC MEDICINES SCHEME IN RAJASTHAN “MUKHYAMANTRI NISHULK DAVA YOJANA” Introduction The availability and affordability of good quality healthcare in times of need is one of the most crucial necessities of public wellbeing in any country. A major component of ensuring that such a system of healthcare exists is the degree of people's accessibility to medicines- affordable and good quality medicines- for both prevention and cure. In India, in spite of the remarkable success of its pharmaceutical industry, the provision of affordable medicines to people remains a daunting task. Several research studies show that expenditure on medicines in India accounts for about 50 to 80 per cent of the total cost of treatment. At least three-fourths of the total out-of-pocket expenditure in the country is spent on buying essential drugs and medicines many of which are highly overpriced. The cost of medicines is so high that it often leads to rural indebtedness and a shift to below poverty line. As a result, almost about 65 percent of India's population lacks regular access to medicines. Some alarming facts As per WHO 65% of the Indian population lacks regular access to essential medicines. The expenditure on health is the second most common cause for rural indebtedness Expenditure on health is responsible for 2% shift from APL to BPL every year. Over 23% of the sick don’t seek treatment because they are not having enough money to spend. Expenditure on drug constitute about 50-80% of the health care cost. Over 40% of hospitalized patients have to borrow money or sell their assets to get them treated. A study by World Bank shows that as a result of single hospitalization 24% of people fall below poverty line in India. Ironically enough, India is referred to as the pharmacy of the world; known for the production of generic medicines. India is not only the third largest producer of generics by volume but also one of the least expensive drug producers. Government health programs in over a dozen countries like Brazil, Ecuador and Thailand, source generics from India. Generic medicines are therapeutically equivalent but cheaper alternatives of usually costlier branded medicines. Every medicine has a salt name that indicates the chemical composition and a brand name to reflect the manufacturer. Brand names are costlier because of the artificial monopoly which they enjoy by evading market competition and huge marketing promotion and advertising costs. If a doctor prescribes the salt name, then the pharmacist can offer the patient a choice between the expensive branded and cheaper generic medicine which are both of equal potency. Need for the innovation Till very recently, medical practitioners due to lack of awareness as well as due to incentives offered by the pharmaceutical industry were in the habit to prescribing the drugs by brand names. Often they were not aware of the cost difference between different brands. This has led an increase in cost of treatment and unnecessary prescription of non-essential, irrational, luxury and wasteful drugs. In addition, geographical access to medicine is a serious concern in the state. The residents in rural areas needed to travel long distances to visit a health facility or to buy essential drugs. In spite of such efforts, access to cost effective, appropriate medicines and their rational use continued to be a challenge in Rajasthan. There remained large gaps in the processes of medicine procurement, quality checking, distribution and pricing. Till very recently, the State Purchase Organization (SPO) under Medical and Health Directorate of Rajasthan was responsible for the procurement and distribution of medicines to government medical facilities across the state. Under the organization, there were constant irregularities in the supply and packaging of essential medicines and other surgical equipments. The SPO had a limited contract of supplying only 45 types of essential medicines; hospitals were responsible for procuring all other medicines independently. Due to lengthy tender processes, more time, effort and money was spent. Under the SPO, there was no maintenance provision in contracts and there was a lack of an inbuilt facility for logistics and distribution. The quality control and inventory management system was also very weak with very limited use of information technology. Along with these shortcomings there were problems of inadequate, unkempt storage and deficit in transportation facilities. The Innovation - Mukhyamantri Nishulk Dava Yojana (MNDY) A step towards making treatment affordable for the entire population of the state through “Provision of Commonly used Essential Medicines” free of cost. Recognizing the need to address these crucial roadblocks on the way to providing affordable, good quality and timely healthcare to people, the Government of Rajasthan (GOR) announced the “Mukhyamantri Nishulk Dava Yojana”(MNDY) for providing commonly used essential generic medicines free of cost to all patients visiting government health facilities (Budget announcement 2011-12). "Mukhyamantri Nishulk Dava Yojana" was launched on Mahatma Gandhi's Jayanti i.e 2nd October, 2011 by Shri Ashok Gehlot, Hon’ble Chief Minister of Rajasthan. The scheme is a novel venture of the State Government for increasing the accessibility to essential medicines and thereby improving health of state's population. , Universal in Nature The benefits under the aegis of MNDY have been extended to the entire 7 Crore population of the state (irrespective of BPL and other categories being benefitted under Mukhyamantri Jeevan Raksha Kosh). The aim is to provide free medicines to all so that no patient is deprived of treatment on account of lack of medicines. No BPL Card, ration card, not even any Id proof is required for availing benefit of free medicine scheme. The only qualifying criterion is that one has to be a human being; he may not be a citizen of the state, so that there is no barrier to access of essential medicines. Number of medicines steadily increasing Under the scheme currently about 400 commonly used essential medicines (which can treat approximately 90% illnesses) are being made available to all patients visiting OPD and IPD at all government healthcare institutions viz-Medical College and associated group of hospitals, District Hospitals, Sub-divisional hospitals, Satellite Hospitals, Community and Primary Health Centres, Subcentres and Dispensaries; however as per announcement of Hon’ble Chief Minister the number of drugs is to be increased to 600, accordingly the EDL has been revised incorporating specialty medicines; tendering for these is under process and the same will be made available in next 2-3 months. According to WHO a limited number of essential drugs are able to cater to the healthcare needs of the majority of the population. The scheme is being implemented at 28 Medical College attached hospitals, 56 DH/SDH/Satellite Hospital 428 CHC’s, 1844 PHCs, 12701 Sub-centre & others, estimated total at 15000 hospitals. Distribution of drugs to patients is ensured through approximately 16053 free Drug Distribution Centers (DDC) established across all healthcare institutions of the state. The Mukhyamantri Nishulk Dava Yojana was launched to address accessibility and affordability issues related to essential medicines; looking to the ambitious nature of the scheme a structured framework was put in place to holistically cover all aspects of implementation in time bound manner. The framework comprises of hard and soft components as reflected by the table below - COMPONENTS OF FREE MEDICINES SCHEME (HARD COMPONENT) (SOFT COMPONENT) (B) TO CHANGE PRESCRIPTION BEHAVIOUR OF DOCTORS (1)Establishment of an autonomous centralized (1)Sensitization and orientation about rational use of procurement agency drugs (RUD) (2)Identification of drugs for free essential drug list (2)Write prescription on self carbonated prescription slips (EDL) (3) Procurement of all essential and life saving drugs (3) Diagnosis must be written through a two-bid transparent e-tendering process (4) Drug Warehouse at every district (4)Write Generic / Salt names (5) Empanelled laboratories for quality testing (5)Use out of Essential Drug List (6) System for transportation of drugs (6)Follow Standard Treatment Guidelines (7) System for storage and drug distribution of drugs in (7)Constitution of Drug and Therapeutics Committee all hospitals (8) e-Aushadhi Software for Inventory management (8)Prescription Audit. (9) Transparent and prompt payment system (9) Report on Adverse Drug Reactions(ADRs) (10) Sufficient funds. (10) Patient counselling (A)TO MAKE DRUGS AVAILABLE IN GOVT. HOSPITALS ADVANTAGE OF ECONOMIES OF SCALE Being a central procurement agency RMSC has the benefit of the “Economies of Scale” wherein procurement of medicines at lowest rates can be ensured due to the bulk central purchase orders. This results in additional, easy and early purchases of medicines, equipments and instruments. Due to bulk purchase, easy and short tender procedures, the State government has saved on time and money. The table below reflects the cost of some commonly used medicines –tender price of RMSC and that of equivalent market brands. COST COMPARISION Disease/ use Name of Drug Pack Size Pain killer Diclofenac Sodium Tablets IP 50 mg 10 Tab strip Cholesterol lowering Atorvastatin Tablets IP 10mg 10 Tab Blister Heart disease Clopidogrel Tablets IP 75 mg Diabetes Glimepiride Tablets IP 2 mg Equivalent Popular Brand Voveran (Novartis) MRP RMSC Tender Price Rs. 31.73 Rs 1.24 Atrova (Zydus) Rs. 103.74 Rs 2.98 14 Tab Strip Plavix (Sanofi) Rs. 1615.88 Rs.8.54 10 Tab Strip Amaryl (Aventis) Rs. 117.40 Rs.1.95 A. TO MAKE DRUGS AVAILABLE IN GOVT. HOSPITALS 1. Establishment of an autonomous centralized procurement agency Rajasthan Medical Services Corporation (RMSC) The genesis of establishment of Rajasthan Medical Services Corporation Limited (RMSCL) lies in two important announcements of Hon’ble Chief Minister of Rajasthan in the budget speech for the year 2011-12, which were: Point No. 47: Establishment of Rajasthan Medical Services Corporation as a central procurement agency which would be responsible for procurement of generic medicines, surgical and diagnostic equipments for all healthcare institutions of the State. Point No. 48: Commonly used essential medicines will be made available to all patients visiting Government healthcare institutions with effect from 2nd October, 2011. Also patients of Thalassemia and Haemophilia will be provided free treatment with effect from this date. , The RMSC is responsible for the procurement and distribution of generic drugs and medicines, surgical and diagnostic equipments to government medical institutions in the state of Rajasthan. Additionally RMSC has also strengthened the process of quality control over drugs; ensured availability of drugs at all times and promotes the rational use of drugs with special emphasis on the use of generic medicines. In pursuance of the above mentioned first budget announcement, the Sate Cabinet approved the establishment of RMSCL vide its Order No. 49 / 2011 dated 04 April, 2011 and RMSCL came to existence in May, 2011 as State Public Sector Enterprise in the form of a company wholly owned by the State Government, registered under the Indian Companies Act, 1956. Constitution of Board of Directors A Board of Directors has been constituted to decide upon all administrative and policy issues. The Corporation is headed by Principal Secretary, Medical and Health Department, who is ex-officio Chairman of the Board of Directors of the Corporation. Other members are senior officers from NRHM, RMSC, DM&HS and Finance Department. Technical Advisory Committee A Technical Advisory Committee (TAC) has been to provide guidance and supervision for various technical issues regarding procurement of medicines and other items. The committee finalizes the drugs to be included in the EDL, and its updation from time to time, guidance on tender conditions to better the procurement processes, advice on specifications. The other members of the committee who assist MD, RMSC on all technical aspects are from DM&HS, Medical colleges, Finance Deptt. GoR, Pharmacology Deptt. of medical colleges and other nominated and special invitees. RMSC CELLS For each of its diverse functions, the Corporation has been organized into different cells. These cells have their specific roles to play in the efficient functioning of RMSC as also implementation of the scheme 1. Procurement cell - for finalization of tenders of medicines, surgical and suture items 2. Supplies cell – for placement of purchase orders and maintenance of supply chain in the state 3. Logistics Cell – ensures proper storage, temperature maintenance and dispensing 4. Quality Control cell – testing of drugs at empanelled labs 5. Finance Cell - ensures payments 6. I.T cell – for maintenance and smooth deployment of “e-Aushadhi” software 7. Equipment Procurement Cell – for finalization of tenders of equipments and machines Three Tier System for supply of Free Generic Medicines RMSC State Head quarters -JAIPUR Supply Cell Logistic Cell Finance Cell Procurement Cell Quality Control Cell IT Cell Districts Drug Warehouses – 34 Officer in-charge – DDW Pharmacist 1(Warehouse Storage Manager) Pharmacist 2(Hospital Supply Manager) Data Entry Operator 1 & 2 Helpers (need based) Security (need based) Drug Distribution Centres – 16053 Pharmacist Data Entry Operator 2. Identification of drugs for free Essential Drug List (EDL) The Technical Advisory Committee at RMSC comprising of senior doctors from medical colleges, inservice/retired pharmacology experts, RUHS representative, RMSC officers from Procurement, Logistic and Quality section, subject experts, Finance Dept. representative arrived at the final Essential Medicines List (RMSC Procurement List 2012) after detailed discussions and deliberations. EML was developed based upon WHO and National List of Essential Medicines using explicit, previously agreed criteria, based on efficacy, safety, quality, cost and cost-effectiveness. The document has been compiled taking into consideration the generic name of medicine, levels of care, the RMSC procurement rate and also the comparative prices of some popular market brands. It also gives information on the surgical and suture items being procured by RMSC and the free medicines being provided under various National Health Programs. The document has been disseminated to all doctors and para-medics across the state. Recently the list was revised to include more number of specialty drugs after recommendations from the premier healthcare institutions of the state and seeking necessary approval by the TAC. The RSEML 2013 now has total 607 medicines, 73 surgical and 77 suture items i.e in total 757 items. The most important feature of the RMSC procurement list is its focus on the procurement of only generic medicines. (Annexed) 3. Procurement of all essential and life saving drugs through a two-bid transparent e -tendering process Drug procurement is done through an e-tendering process according to a strict written protocol. Tendering is done once a year for most products, based on last year’s consumption although this has been difficult due to the lack of consumption data in the relatively short time that RMSC has operated. The bidding process follows two processes – technical evaluation first, followed by financial evaluation for only those suppliers that pass the technical evaluation. Technical evaluation is done by a committee of 8-10 people that include staff from the procurement unit of RMSC and drug control department with staff deputed from the Drug Regulatory Authority. The Purchase Committee consists of 8 people, including Executive Directors from each unit in RMSC, the Drug Controller and the Chief Accounts Officer. Criteria to pass technical evaluation cover both supplier and supply criteria and include: Supplier must be a manufacturer or importer, Supplier average annual turnover of more than 20 crore for last 3 years. Production of the product by the supplier for more than 3 years, Supplier not blacklisted by any Medical Services Corporation or other State/central government procurement agency in India, GMP certificate for the product, Agreement to supply products with the specified shelf-life and labeling and packaging, which should include the RMSC logo and words “not for sale”, Agreement to supply general products within 45 days and imported or injectable products within 60 days. The entire tendering system is based on a two bid system: 1. technical and 2. financial bid Once the bids are submitted on-line by a specified date, the technical evaluation committee opens the technical part of all bids, undertakes a technical evaluation and presents the results to the Purchase Committee who decides which suppliers and products have passed the technical evaluation. Results of those suppliers and their products that pass and fail are then placed on the web and a few days given for failing suppliers to appeal. The technical evaluation committee will reassess their bids, re-discuss with the Purchase Committee and respond on the web. Once the list of suppliers and products that have passed the technical evaluation is finalized, the Purchase Committee gives permission to open the financial bids of only those suppliers and products that pass the technical evaluation. Two out of three members of the technical evaluation committee (that have the concerned authority) can open the financial bid online. The products that qualify with the lowest price (L1) are chosen, provided that their prices are equivalent to or lower that those found in the market survey. For a product where the quoted price is higher than that of the market survey, the supplier is invited to negotiate with the purchase committee. However, if he cannot equal the price, a retendering for that product is initiated. Other suppliers that match the lowest (L1) price or are the second (L2) and third (L3) lowest process are also identified as they may be approached for purchase should the first L1 supplier fail to supply all products on time. If any item is not approved by the Purchase Committee for any reason, the tenders are invited again and the process begins anew. In the earlier procurement system under the SPO, a purchase preference of about 100 per cent was given to public sector pharmaceutical companies and 80 per cent to state small scale industries if they matched the L-1 rate. This has been altered with the new procurement policy with purchase preference being restricted to 25 per cent out of which state pharmaceutical companies receive 10 per cent preference and state small scale industries receive 15 per cent preference if they matched the L-1 rate. The drugs, medicines, surgical & suture items are procured based on the need and consumption pattern of the items by the Government Healthcare Institutions. Procurement orders are normally placed to meet out 4 months need and 2 months pipeline stock which are likely to be in transit and under quarantine. Though the procurement is centralized and purchase orders are issued from RMSC headquarters but the suppliers are required to supply the items directly in the District Drugs Warehouses (DDW) of each of the districts as per orders. Drug availability at various level. Level of care Tertiary Institutes Suture items Drug Items Surgicals Medical College Hospitals 410 70 72 District / Sub-dist / Satellite Hospitals 375 60 62 CHCs 150-225 50 50 PHCs/Dispensaries 75-150 25 25 Sub Centers 20-30 0 0 Secondary Primary CHALLENGES IN SUPPLY CHAIN Proper annual demand generation Proper and timely indent generation Cold chain maintenance (in summer temp rises to 51 c) Population- 6.8 million population - longer waiting times Geographical spread of the state 342,239 Sq. Km. Approach - PHC upto 150 km from HQ High patient load in tertiary care centre. Choice –medicines like cough syp, analgesic oint. Epidemics of swine flu-malaria-dengue-chickengunia-scrub typhus etc Supply should be un-interrupted • No scarcity of Pharmaceutical manufacturers • Need for Supplementary methods of procurement • Alternate supplier for each drug 4. Drug Warehouse (DDW) at every district Before the inception of RMSC the District Drug Warehouses were functioning as stores for CM&HO, receiving all supplies from Central and State level. However with the establishment of RMSC and implementation of MNDY the DDWs were strengthened and staffed by RMSC. Earlier the DDWs were under the administrative control of DM&HS but subsequent to constitution of RMSC the DDWs (like in other states) were formally transferred to RMSC for all future purposes. Currently there are 34 DDWs, one for each of the 33 districts and one additional DDW has been established at Jaipur to cater to the demand of the district (as the SMS Hospital is the premier institution and caters to a huge load of patients not only from within the state but also from neighbouring states). Manpower deployment: Human resources for health are identified as one of the core building blocks of a health system. They are the healthcare industry’s most important asset and key to success of any intervention; hence the DDWs were strengthened appropriately for efficient transactions and operations at the drug warehouse as follows – Officer in-charge – DDW (earlier DPC, RHSDP a MO/SMO from the M&H Deptt.) Pharmacist 1(Warehouse Storage Manager) Pharmacist 2 (Hospital Supply Manager) Informatics assistant (2) Helpers(need based) Security man(need based) The OI/c is the nodal officer for implementation of MNDY and assists CMHO in effective functioning of DDW. The entire responsibility of drug warehouse management (Infrastructure strengthening, receiving medicines, their upkeep and supply chain) & monitoring is carried out by him together with his assistant staff within the respective district. Infrastructure strengthening of DDWs The drug warehouses were suitably strengthened for effective management and optimal functioning as follows – (a)For Inventory Management Heavy Duty Racking System 8’ feet Heavy Duty Racking System 14’ feet, Hydraulic Hand pallet trucks Pallets Side Racks (b) For Computerization Desktop Computer Core i3 Based Desktop Computer Core 2 Duo 24 pin 136 Column Printer Laser Printer Bar Code Reader Bar code Printer (c) For Cold Storage Cold place(2O-80 C)- Walk-in-Coolers constructed at all DDWs, ILRs Cool place(80 - 280 C) - Air Conditioners in Rooms Normal temperature (d) Others 1 KVA Inverter cum UPS with 4 hr backup Steel Cupboard Office Table Chairs Fire extinguishers As per norms each DDW was developed to have the following: Seating space for staff with office infrastructure Adequate facilities for storage of medicines Quarantine area for storing of medicines waiting for quality check approval Walk-in-Cooler Area for “Not of Standard Quality Drugs”(NOSQ) Space for loading and unloading of supplies 5. Empanelled laboratories for quality testing As far as the quality of drugs is concerned it is primarily the responsibility of the concerned manufacturers and it is regulated by the Drugs Regulatory Departments of Central & States Government under the provisions of Drugs & Cosmetics Act & Rules there under. As per drug laws drug manufacturers can release the drugs for sale or distribution only when the drugs are found conforming to all quality parameters. Drugs regulatory officials enforce & monitor compliance to these provisions and based on this quality assurance system, drugs are made available to the patients everywhere. However the RMSC has evolved more foolproof mechanism of additional multiple checks on quality of drugs at every stage of procurement process including pre-release retesting of all the batches of drugs through empanelled labs. I. Checks at procurement level- Selection of quality compliant suppliers: Strict parameters for selection of reputed supplier companies Provisions laid down to carry out their factory audit on random basis from time to time II. III. Checks at supply level-Acceptance of drugs with QC passed COA: It is mandatory on the part of drug manufacturer to check quality of all active pharmaceutical ingredients as well as all inert excipients used in manufacture of drug formulation. Carry out in process quality control checks and finished product analysis and the every batch of a drug is released only when it is found conforming to specified quality standards Mandatory on the part of supplier to send QC passed test report of each batch supplied along with the invoices, without which goods shall not be accepted in warehouses. Checks at release level:-Pre-release quality assurance by retesting of all batches of drugs in Govt. approved empanelled labs: IV. The stocks of drugs received at warehouses of corporations are first quarantined and samples of each batch no. drug are drawn and sent to QC Cell of RMSC headquarters The QC Cell gets them retested through empanelled labs of the corporation. Batch release instructions are uploaded on e-Aushadhi software after getting QC passed test reports from empanelled lab allowing their shifting from quarantined area to distribution area and release thereof to DDCs & healthcare institutions for distribution to the patients. The drugs which failthe quality testing at empanelled labs are required to be kept in the area demarcated as “NOSQ” i.e NOT OF STANDARD QUALITY Ongoing checks-Further quality checks during storage & on receipt of quality complaints: The RMSC QC Cell enquires all quality complaints which are received The QC Cell also keeps continuous vigil on quality of drugs and may carry out retesting of batches on random basis as and when required. The DDWs & DDCs incharge also check the batches physically in their possession from time to time and any changes or defects noticed visually are reported immediately to QC Cell. Procedure for Receipt of stock & drawl of samples from District Drug Warehouses for the purpose of retesting: 1. The drugs supplied by the supplier against Purchase Order issued from RMSC headquarter is accompanied with supplier’s invoice and QC passed test reports of all the batches. The stock of medicines received is tallied from invoice & entered by the warehouse in-charge in Register as well as in e-Aushadhi software. The supplier also mails one copy of invoice & QC passed test reports of all the batches to headquarter QC cell for the purpose of sampling planning. 2. Stock of medicines is kept in QUARANTINE AREA of warehouse. 3. Drugs supplied by the suppliers are subjected to quality test by the empanelled laboratories as per policy. 4. Samples of each batch of supply are drawn from each warehouse within 05 working days from date of receipt in the specified quantity of the item required for testing by the team of warehouse in-charge, pharmacist and other members who may be notified as per sampling plan. The item wise sample quantity to be drawn is provided by QC cell from head office to all DDW’s. 5. The samples drawn in warehouses are duly packed preferably in cartons and outer side of pack is duly signed by members of the sampling team at DDWs and sent along with requisition slip to the Head Office of RMSC through the courier / cargo to reach at the earliest at Jaipur. Samples are sent only after making all necessary entries in the software system. 6. If any particular batch of a product is received again in QC Cell after a gap of 30 days from earlier receipt, then the sample may again be drawn from received stock and sent for testing to empanelled lab, if it thinks appropriate. 7. In order to ensure the quality of the drugs during the storage in warehouses, samples may be drawn for retesting as and when required. 8. In case of any specific complaint or any suspicion about the quality, it is immediately to be reported to RMSC headquarters. The inspection team of RMSC may be constituted and / or an officer going for inspection of the warehouse may also take samples and hand over to the quality control cell in the head office for testing. The outcome of the report will have to be reported to the Managing Director immediately. 9. In case of any serious adverse reactions reported in the government healthcare institutions during administration of any drug the warehouse in-charges are required to act immediately and inform by phone & email to the Head Office and take all measures to stop further distribution with immediate effect and retrieve & recall all the stocks of such drugs supplied. Matter in such cases will also be reported to Drugs Control Department for needful action beside investigations at RMSC level. Treating doctors will fill form as prescribed by CDSCO for taking up the matter with DCGI & concerned state Drugs Controller for needful action at their end also. Process adopted for secret Coding of samples: Out of the samples received in the Head office from all the warehouses, the quantity of common batch of each item are mixed and from each batch two portions are made from pooled quantity out of which one is sent for testing and another kept as control sample till its expiry unless required for any other verification. Rest of the quantity of the batch is kept in secured area. If sample passes the quality control test, the remaining quantity lying in the QC Cell of RMSC is issued to DDW / DDC for distribution within one month and if sample fails the quantity is utilized for further confirmatory testing. From the sampled drug, the particulars like manufacturers name, manufacturing licence number and any other distinct marks of the supplier company, if any, are concealed either by using black indelible ink or by fixing non-removable stickers and thereafter each unit pack of drug is assigned secret code number which is of alpha-numerical digits only. All relevant entries are made in computer and sample meant for testing is sent to one of the empanelled laboratories for analysis as per plan. Written memorandum with request to test samples as per specified timeline accompanies the samples and it contains code number and details of drugs without particulars of the supplier which have been concealed during coding. However samples to the Govt. Labs viz. CRI, NIB, DTL etc. and also such samples coding of which affect products integrity & quality are sent in original packing & without coding. The selection of empanelled laboratories for test & analysis of specific drug is done on rotation basis keeping in view the backlog of the pending samples. Samples secretly coded are sent through messenger and outside the city they are sent through courier or messenger to ensure that it reaches the labs, at the earliest. QC Cell at headquarter sends the samples to empanelled labs at the earliest, possibly within 3 working days from date of receipt from DDWs to get early reports. 6. System for Transportation of Drugs from DDW to Institutions ,, For smooth management of supply chain in the district, transportation guidelines have been issued from the state level. Transportation of medicines from District Drug Warehouse to institutions may be done by two means as below A. Transportation by vehicle owned by medical institutions B. Transportation through hired vehicle (i) For Transportation purpose necessary budget has been allocated to respective CM&HOs/PMOs. (ii) If budgetary amount is inadequate, additional demand may be sent to Director PH by CM&HOs/PMOs (iii) CMHO may either hire vehicle for whole of the district or transferred to Deputy CMHO /BCMO in order to ensure smooth transportation. fund may be Procedure of medicine supply from DDW Preparation of route chart - Route map is prepared based on geography of the district for smooth supply (Day/Date wise institutions for supply) and circulated to all institutions by CMHO in consultation to respective DPCs. Indent from Institutions - Concerned pharmacist of all institutions of the particular area of the district comes to DDW with indent form dully signed by MOIC /PMO/ Superintendent of Medical Colleges on pre decided date / Day. Verification of Indent & Time Schedule - O I/C DDW verifies the time schedule of the institution. Passbook system & Issue Voucher – Medicines are collected by pharmacist of DDW and voucher is generated. The total amount of the medicines demanded by the institution is mentioned in the passbook of the concerned institution. The supply is packed as per indent. Voucher is also provided to the Pharmacist / Store keeper of respective institution. Pooled transport/ Hired vehicle – If required a common vehicle is hired, , by CMHO for the purpose of supply of medicines on rent (Drug Distribution Van) It loads all the goods of the all institutions of the particular district and supplies them to respective institutions and get receipt from the storekeeper of the particular institution. Delivery Schedule Logbook - A pre-designed logbook is provided to the driver. This log book may be filled at the starting point (at DDW) and signed by OIC DDW. The OIC DDW enters the date, time, reading of milometer (starting kms), names of institutions of the day where supply is to be delivered. After reaching the first point of delivery, concerned storekeeper / In-charge of the institution receives the delivery and mentions the date, arrival time, total kms (distance from the DDW) and signs logbook. Logbook Maintenance & verification - Similar process of delivery is followed. Recording in Logbook is done at each institution for the day. The distance is entered in the Logbook from the last institution. Payment At the end of the month total kms are to be calculated and payment done by CMHO as per MoU/Rate Contract. For which budget has been provided to CMHOs by DMHS. 7. System for storage (Sub-stores) and distribution of drugs (DDCs) in hospitals Sub-stores at Hospitals The existing central stores at the healthcare institutions are vital links of supply chain management system, therefore a need to strengthen them was felt to facilitate efficient implementation of MNDY; thus the central stores were renamed as Sub-Store and suitably strengthened through provision of funds for civil works (need based), minor repairs, racks, fridge, etc. The funds at institution level were provided as under – Strengthening Sub-stores at HC Institutions Strengthening of Sub-stores at MC Hospitals PHC - @ Rs.25, 000 CHC - @ Rs. 50,000 DH/SDH/SH - @ Rs. 2.00 lacs SMS M C Hospitals - @ Rs. 20.00 lacs Other M C Hospitals - @ Rs. 10.00 lacs Attached Group of Hospitals - @ Rs. 5.00 lacs For smooth functioning the medical officer in-charges have been directed to obtain medicines as per requirement from the drug warehouses, store them as per issued guidelines at sub-stores and make them available at drug distribution centres (DDCs) established in the institution. The e-Aushadhi software is also deployed at the sub-stores and captures all inventory management data. Drug distribution centers (DDCs) in Govt. hospitals , The Drug Distribution Centers have been established based on OPD and IPD load of each institution, a total of 16053 DDCs have been created across the state. All DDCs operate during OPD hours and for IPD/Emergency/Casualty patients 24X7 availability of medicines is ensured by the medical officer incharges through identified DDCs. The onus of making medicines available to all OPD and IPD patients lies with the MOI/c, PMO and Medical Superintendent of the respective institutions. An amount of Rs. 2.25 lacs was sanctioned for creation of every new DDC (civil works, furnishings, fridge, computer etc.) and was made available to the respective institutions through the parent department of M&H and Medical education. Each DDC is managed by pharmacist who is responsible for smooth transaction of medicines, ensuring continuity of medicines by replenishment from Sub-store and proper storage of medicines as per issued guidelines. The data entry operator at the DDC captures the transactions in e-Aushadhi and issues voucher to all patients. At the DDC records for all prescriptions are being maintained as RMSC has provisioned for duplicate prescription slips. The pharmacist at the DDC takes the signatures of the recipient, issues the medicines and returns the original prescription slip, while retaining the duplicate slip (for a period of six months). These duplicate slips are provided to the medical officer incharge, 1% of these are subjected to “Prescription Audit” by the Drug & Therapeutic Committees constituted at the institutional level. Fair price medicine shops & BPL counters. Apart from the DDCs generic medicines are also given to BPL counters. Since not all medicines are available at the DDCs, patients may be required to pay low cost at fair price shops to obtain particular medicines which are not part of essential medicine list. Therefore under the current system patients can obtain generic medicines from both free of cost centers and fair priced shops. These include: , Lifeline Store – at low cost BPL Counters –free of cost FLOW CHART FOR DRUG DISTRIBUTION UNDER MNDY RMSC SUPPLIER SUPPLIER SUPPLIER Purchase Orders 34 DISTRICT DRUG WAREHOUSES 16053 DRUG DISTRIBUTION CENTERS Medical College Hospitals District Hospitals/Sub-divisional Hospitals/Satellite Hospitals Community Health Centers Primary Health Centers All patients visiting OPD & in IPD Sub-Centers 8. e-Aushadhi Software for Inventory management Record Keeping: of all medicines received from the suppliers and issued thereof to the institutions is done online through e-Aushadhi software a web based application, developed and maintained by Centre for Development of Advanced Computing (CDAC). All transactions, inventory management are meticulously handled through this software. Initially the record keeping at DDCs was being done manually, however in October 2011 all Sub-stores and DDCs were computerized and manpower was trained to efficiently handle the software. e-Aushadhi is a web based application which deals with inventory management of stock of various drugs, sutures and surgical items at DDWs. The application has been developed by the Centre for Development of Advanced Computing (CDAC), the software is being continually upgraded in house by the I.T cell of RMSC as per requirement of DDWs for managing the inventory effectively. The e- Aushadhi software utilizes a propriety software Oracle for the back end and Java for the front end. Key features of "e-Aushadhi" Drug inventory desk: Store, maintain, update, search & display information related to drugs. Drug Issuance desk: Indent generation and issuance of drugs to hospitals/institutions Quality control desk: Tracking quality check progress Sample register desk for recording the receipt of sample, return of sample and disposing of sample Condemnation register desk Drug locator and transfer of drugs: helps to locate drugs in various warehouses and facilitate transfer of drugs between drug warehouses whenever needed. Ability to prepare comprehensive reports The software also enables maintaining a record of lost drugs, returned drugs, any miscellaneous consumption and conducting periodic physical stock verification by cross checking it with the data on the software. The access to e-Aushadhi has been given to the following stakeholders: Supplier to check the delivery and status of his/her products Principal Health Secretary(M&H) &Medical Education Director Public Health OSD, Medical Education CMHO and Principal Medical Officer (PMO) for monitoring To all 34DDW in-charges for inventory management and transfer of drugs to and fro. To all the heads of the various cells at RMSC for monitoring Training for the use of the software has been given by CDAC to all concerned staff using for operating the software. At state headquarters the operations are handled by a core team of CDAC deputed at RMSC and along with RMSC staff. The software is deployed at all DDWs, Sub-stores and DDCs upto PHC level across the state (except a few PHCs where connectivity issues are being addressed).As of now te software is deployed at all hospitals(medical college, district, sub-divisional and satellite hospitals), CHCs & 1250 PHCs i.e total 3200 online drug units. 9. Transparent and prompt payment system A transparent and prompt payment system has been put in place at RMSC to ensure timely payments to suppliers and all stakeholders. The following procedure is followed Payment either through CBS (Core banking solution, anywhere banking), or/ and NEFT (National Electronic Transfer) up to 1.00 Lac or and through RTGS (Real Time Gross Settlement) if more than 1.00 Lac. e- Processing of suppliers payment through e- Aushadhi Software. Physical Cheques are not issued to any suppliers. Centralized payment to all stakeholders viz suppliers, DDWs staffers/ various service providers. TDS and other statutory dues etc through e-payment only. 10. Sufficient Funds At the time of commencement of the scheme budget allocation was made for provision of free medicines at all healthcare institutions of the state based on levels of care. The state government has provisioned for sufficient funds for the implementation of the scheme in the annual budget for 2011-12 and 2012-13. Total Budget allocated for year 2011-12: Rs.200.00 Crores (which includes Rs. 5.00 Crores Equity contribution and Rs. 5.00 Crores loan) Expenditure upto March 2012: Rs.190.00 Crores Total Budget allocated for year 2012-13: Rs. 341.1953 Crores Expenditure upto March 2013: Rs.261.60 Crores Budget allocation for F.Y. 2012-13 Medical Education Department S. No Type of Health Institution 1 SMS Medical College &attached group of hospitals 2 Other Govt. Medical Colleges &attached group of hospitals 3 Govt. Dental College Medical & Health Department – S. No Type of Health Institution 1 Sub-Centers 2 PHC 3 Urban PHC & City Dispensaries 4 CHC 5 6 SH & SDH DH No. of Health Institutions 11487 1517 37+198 30 bedded -285 50 bedded – 70 75 bedded –17 100 bedded – 4 18 50 bedded – 3 100 bedded – 3 150 bedded – 10 200-225 bedded - 5 300-350 bedded -12 400 bedded -1 Proposed Budget (Rs.) 45.00 Crore 15.00 Crore 75. 00 lacs Proposed Budget (Rs.) 10,000 1.25 lacs 3.00 lacs 7.50 lacs 15.00 lacs 22.50 lacs 30.00 lacs 22.50 lacs 15.00 lacs 30.00 lacs 45.00 lacs 60.00 lacs 90.00 lacs 120.00 lacs Besides this an additional budget of 10% was kept in reserve to address need based demand in times of exigencies (after consumption of allocated budget) and after approval by authorities at appropriate level. During F.Y. 2012-13 Rs. 341.1953 Crores was transferred under the State Plan for procurement of drugs/surgical/sutures. Further during F.Y. 2012-13 drugs/surgical/sutures worth Rs. 261.60 Crores have been purchased and worth Rs. 216.00 Crores have been distributed to the medical institutions. Passbook System: was created to maintain record of medicines issued to a particular facility against the allocated budget. Two copies of the passbook are maintained – one at the DDW and the second by the respective institution. The authorized person from the healthcare facility collects the medicines in accordance with the pre-decided calendar days and entries of the budget against the issued medicines are registered in the passbooks. RMSC provides medicines upto 90% of the budget allocated to each of the institutions and additional 10% budget is allocated to meet emergencies like epidemics, communicable diseases, disasters or when there is stock-out of essential medicines. The MOI/cs are able to procure medicines through local purchase at competitive rates. B. TO CHANGE PRESCRIPTION BEHAVIOUR OF DOCTORS AS per WHO it is not only increasing access but also implementing rational use of drugs that makes the access truly holistic. Not only the EML has been implemented well in the state, but there has been education and supervision to ensure that all doctors prescribe EML drugs by generic name. Various orders have been issued by the Principal Secretary of Medical & Health via the RMSC to all facilities requesting that: Essential drugs be prescribed, Use of non-essential drugs be justified by the concerned doctor, Drugs be prescribed by generic name, Carbon copy prescriptions be used, one copy for the patient and one for the facility, Prescription audit be done by the DTCs to ensure appropriate use of medicines, STGs to be followed by doctors, Diagnosis be written on all prescriptions which should be signed by the doctor Patients be counseled, Drug and Therapeutic Committees be established in all large hospitals, Dispensing be monitored. In addition, there has been extensive education of the public through IEC interventions such that patients now know that they are entitled to receive free medicines from the health facilities. The RMSC has a monitoring an evaluation unit, which operates a help-line. Patients are free to call this number if they do not get medicines from the facilities. 1. Sensitization and orientation about rational use of drugs (RUD) Pursuant to launch of MNDY an initial resistance to change in the prescribing pattern was felt on behalf of the doctor community deployed at public health institutions; therfore seminars,confrences and review meetings were held regularly at state, zonal and district level to sensitize the doctors towards rational use of drugs. All 33 districts have been covered by a core team of RMSC. Workshops organised were attended by all government/ private doctors of the district, as also NGOs working on health issues.The impact is being observed in the visible change in prescriptio practices of the doctors at all public healthcare institutio sof the state. The sessions focussed on topics of rational use of drugs, factors underlying irrational use of drugs, how the industry benefits from brands and promotion of non-essential drugs, RMSC – EML, prescription by genric name, “False” Evidence-based medical practice, Promotion of Hazardous, Banned and Bannable Drugs, Me too drugs, lack of objective drug information and the the ultimate solution: statutory price control for all essential drugs.The aim of the workshops was with a take home message To make treatment accessible and affordable To serve the ailing mankind To Save Lives 2. Write prescription on self carbonated prescription slips 3. Diagnosis must be written 4. Write Generic / Salt names In the past too, the state government had issued circulars and orders to address the much neglected aspects of rational use of drugs; however the same were reinforced and reiterated for better compliance with the launch of Mukhyamantri Nishulk Dava Yojana. Self carbonated prescription slips have been made available by RMSC at all govt. health care institutions and circular to prescribe on these slips has been issued with an objective that the duplicate yellow slips are to be retained by the pharmacists deployed at the DDCs after issuing medicines to the patients and obtaining their signature/thumb impression. He /she also mentions the quantity of medicines issued against each item and affixes the seal of “Not available” if a particular medicine/s are not available at the DDC. The retained prescription slips (1% of total OPD and IPD slips) are then audited by the Drug and Therapeutic Committees constituted at each of the medical college hospital and district hospitals of the state. The circular also clearly states that all doctors have to essentially write the provisional/ final diagnosis for the patient’s condition and prescribe medicines by generic /salt name only. The circular also conveys that routinely medicines are to be prescribed for 3 days but can be extended upto 7 days in special cases; however for chronic cases medicines may be prescribed for upto 1 month. Studies undertaken by various agencies like PHFI, WHO, Prayas, TISS students and HCM RIPA trainees reveal that prescription practices are considerably in allegiance with the issued circulars, however scope for improvement exists. 5. Prescription out of Essential Drug List (EDL) The primary purpose of Essential Drug List is to promote rational use of medicines considering the four important aspects i.e. efficacy, safety, suitability and cost effectiveness. Furthermore it promotes prescription by generic names. As per WHO, Essential drugs are those that satisfy the priority healthcare needs of majority of the population. The RMSC - EML 2012 has been framed by Technical Advisory Committee (TAC) of RMSC after several rounds of wide consultations with experts of different disciplines from different districts of the state (medical college faculty and district hospitals) and taking into account the WHO Essential Drug List, National List of Essential Medicines, RSEML 2005, Tamil Nadu EDL. The EML is a dynamic document and feedback from all stakeholders is welcome which will helps in its revision at regular basis. To address the issues of changing disease prevalence, treatment modalities, and introduction of newer medicines and identification of unacceptable risk-benefit profile as well as therapeutic profile of some medicines the EML 2012 was recently updated and RSEML 2013 (will soon be printed and disseminated) now has total 607 medicines, 73 surgical and 77 suture items i.e in total 757 items. The medicines included in the list are most commonly used essential and life saving drugs. Circulars have been issued to prescribe by generic name from within the EML as far as possible and only when the condition of the patients requires medication of salts other than those of EML the prescriber may justify his prescription accordingly. Salient features of RSEML 2012: Names of drugs have been given with their strength and pack size mentioned separately against each for convenience. Level of medical care has been indicated against each drug – U – Universal, i.e of se at Primary, Secondary and Tertiary levels of healthcare S – Secondary Healthcare i.e of use in District Hospitals, Sub district Hospitals, Satellite Hospitals & Community Health Centre’s T – Tertiary Healthcare, i.e of use in Medical College Hospitals Purchase price of RMSC has given for most of the drugs. The price at which a drug is issued to a facility is 5% more than the purchase price. It gives an idea about the purchase economics and may be helpful in calculating the budget at a facility. The prevailing retail prices of some equivalent brands commonly available in the market have been given against each drug for comparison with RMSC prices. List of drugs being provided by GoI for various National Health Programs and Janini Shishu Suraksha Yojana have also been included in the list. Level of care Primary care Secondary care Tertiary care Health Institute Approximately No. of drugs permissable Sub-centre 30 PHCs 200 CHCs 300 District Hospitals 400 Medical college hospitals 500 6. Follow Standard Treatment Guidelines Developing and adopting Clinical guidelines - the Standard Treatment Guideline’s Clinical guidelines (standard treatment guidelines, prescribing policies) consist of systematically developed statements to help prescribers make decisions about appropriate treatments for specific clinical conditions. Evidence-based clinical guidelines are critical to promoting rational use of medicines, they provide a benchmark of satisfactory diagnosis and treatment against which comparison of actual treatments can be made and they are a proven way to promote more rational use of medicines. Standard Treatment Guidelines 2006 were developed by DSPRUD for the state under the aegis of World Bank aided Project RHSDP. It was based on different levels of care, prevalent clinical conditions in the state and the skills of available prescribers. As evidence-based treatment recommendations and regular updating helps to ensure credibility and acceptance of the guidelines by practitioners hence same has been revised by DSPRUD with technical inputs from subject specialists at medical college institutions. The second edition STG 2012 has been printed and disseminated to all government doctors and post- graduate students across the state. For compliance of all above, circulars have been issued time to time from the state government and the M&H Deptt. STGs promote rational use of drugs when: developed in a participatory way involving end-users; easy to read; for their easier and better use introduced with an official launch, training and wide dissemination; reinforced by prescription audit and feedback. Evidence-based regular updating and treatment recommendations to ensure credibility and acceptance of the guidelines by practitioners Sufficient resources are available to meet cost of their development and to cover the costs of printing, dissemination and training. Release of Standard Treatment Guidelines 2012 during the National Conference on”Access to Essential Medicines in India” held at Jaipur on 2nd October, 2012 7. Constitution of Drug and Therapeutics Committee A drugs and therapeutics committee (DTC) also called a pharmacy and therapeutics committee is a committee designated to ensure the safe and effective use of medicines in the facility or area under its jurisdiction, As per WHO governments may encourage hospitals to have DTCs by making it an accreditation requirement to various professional societies. DTC members should represent all the major specialties and the administration; they should also be independent and declare any conflict of interest. To be successful, the DTC should be appropriately located in the organizational structure, be representative of the stakeholders, have stakeholders ownership in the decision making process, use behavioural change models to implement decisions, and enthuse itself to break out of the “regulatory” mode to the “therapeutic leadership” role. Governments may encourage all district hospitals to have DTCs by making it an accreditation requirement to various professional societies. CHCs with less number of beds may join and 4-5 CHCs may have a common DTC. Factors critical to success include: clear objectives; a firm mandate; support by the senior hospital management; transparency; wide representation; technical competence; a multidisciplinary approach; and sufficient resources to implement the DTC's decisions. DTCs can help tremendously in curtailing inappropriate drug use; reduce drug expenditures and increase availability and accessibility to essential medicines thus optimizing the value of limited government funds. In compliance of all above circulars Drug and Therapeutic Committees have been constituted a almost all medical college hospitals and district hospitals of the state and are undertaking role as assigned to them; however institutionalization of the committees and performance upto desired levels will take some time and repetitive efforts on part of the system. 8. Prescription Audit One of the major roles that the Drug and Therapeutic Committees have to play is to undertake prescription audit in order to identify prescription errors and undertake corrective action at the institution. The above mentioned circular issued at the level of Principal Secretary (M&H) and Medical Education also clarifies that audit of 1% of total OPD and IPD prescriptions has to be carried out every month and the audited prescriptions can be destroyed after keeping them for six months period. Prescription audit and feedback consists of analyzing prescription appropriateness and then giving feedback; involving peers in audit and feedback (peer review) is particularly effective. Prescription audit is undertaken to see if the treatment of a specific disease is in accordance with guidelines – the percentage of prescribing encounters in accordance with standard treatment guideline).The DTCs have to identify the % of prescriptions not in accordance with the STGs, number of cases where counseling was done and number of case where action has been initiated. The circular issued states that in case of defaulters – Step 1- Counselling by Unit head and DTC members has to be done Step 2 -Written advice to the concerned doctor by Supdt./PMO/CM*HO/MOIc with copy to the department Step 3-Case may be referred to Principal Secretary M&H /Med. Education for disciplinary action Prescription audits are being undertaken by the constituted committees and defaulters being counseled on a regular basis. 9. Report on Adverse Drug Reactions (ADRs) 10. Patient Counselling The scheme has seen one and half years of implementation and during this period number of reforms encompassing rational use of drugs, prescription by generic name, adoption of EML and STGs have been put in place in the state’s health systems. The M&H Deptt has witnessed a positive response from the major stakeholders, though much still needs to be achieved. Doctors and paramedics have been sensitized during the workshops and review meeting to also report on adverse drug reactions and counsel the patients on use of drugs. The new recruited pharmacist (1345 in numbers) were trained by RMSC staff in Sept 2012 and all issues related to medication errors, good dispensing practices, counselling of patients, reporting on adverse reactions were covered; however limiting factors like excess load of patients, availability of equivalent manpower, literacy status of patients, paucity of time and others are the bottlenecks and need to be viewed critically. IMPACT of MNDY Mukhyamantri Nishulk Dava Yojana was launched on Maatma Gandhi’s Jayanti 2nd October, 2011 with the basic aim to increase access to commonly used essential medicines for all people of the state. The entire population of 7 crore is eligible to benefits under the scheme. This ambitious scheme has been lauded not only at the national level but acclaimed recognition at international platforms as well. As a result the Corporation has witnessed visitors from number of states, NGOs as also from the WHO and the World Bank. The impact can be briefly put together as - 1. Increase in access and equity of the underserved and Reached out to the unreached After implementation of scheme, number of outdoor and indoor patients has increased significantly at government hospitals. Since the launch of the scheme the data is as followsTotal number of beneficiaries - 10.68 Cr. patients More than two lacs patients are being benefitted every day. Before 44 Lac patients per month After MNDY 62 Lac patients per month Study by TISS students reflects that the number of patients has increased after the inception of scheme. “On an average about 80-100% increase in the OPD count” is observed. Doctors are of the view that as the access to medicines has been increased under the aegis of the scheme the patients are visiting all levels of healthcare for availing treatment and this has lead to considerable increase in the OPD i.e MNDY has improved utilization of government health facilities. Similar findings were reported by “Rapid Assessment of MNDY” undertaken by IHMR, Jaipur. 2. Decrease in out of pocket expenditure There is huge amount of reduction in out of pocket expenditure in the treatment of common man as all costly medicines are being provided free of cost. • Everyday we are giving drugs to more than 2 Lac patients • The average cost per patient is around Rs.15 • Otherwise the cost of drugs purchased from the market use to cost around Rs.300 to 500 • The implementation of the scheme has also resulted in COST CURTAILMENT as reflected by the tables below ( a study was undertaken by OI/C-DDW, Bikaner) - Comparison of costs of generic vs branded drug treatment (in Rs) Disease Generic Drugs Branded drugs OPD treatment of 30 days Depression / Mixed anxiety disorder 45.59 799.00 Schizophrenia 100.77 1093.80 Mania 227.49 1962.30 Hypertension 29.28 435.60 Diabetes mellitus 17.19 481.20 OPD treatment of 3 days Diarrhoea and vomiting 17.73 190.81 ARI 12.39 118.19 Comparison of costs of generic vs branded drug treatment (in Rs) Disease Generic Drugs Branded drugs Indoor medical/non surgical cases (Single episode) Myocardial Infarction 2195.73 9381.78 Enteric fever 426.50 2953.40 Pneumonia 381.09 2102.77 Stroke/ CVA 635.32 3636.29 Diabetic ketoacidosis 502.83 3192.41 Comparison of costs of generic vs branded drug treatment (in Rs) IPD surgical cases Generic Branded Private hospital package Abdominal hysterectomy (spinal anesthesia) 1567.25 8369.15 20000 Traditional cholecystectomy under GA 1977.67 13535.59 17000 Herniorrhaphy under SA 2294.31 10491.82 15000 LSCS under SA 1550.49 8211.53 20000 Traditional appendicectomy under GA 1977.67 13535.59 15000 3. Source of Youth Employment Due to implementation of this scheme several youth have got employment. - 1345 Pharmacist have been recruited permanently under this scheme. - 3600 Computer Operator and Information Assistant have been engaged on Contract. 4. Increase in Numbers of Girl Child treated After implementation of the Scheme there is a substantial increase in number of girl child (upto age of 6 years) coming for treatment to Government Hospitals. This will help improve gender ratio by aiding “Save the girl child” programme. 5. Savings to Government After one year of RMSC it was reflected that centralized procurement has resulted in enormous savings to the state government as follows Amount spent on costly medicines by RMSC- approx. 507 Cr. Market price of these medicines – approx. 3000 Cr Savings of approx. Rs. 2493 Cr. to the State Government which can be spent on developmental works or creation of other community facilities. 6. Other effects 1. Reduction in retail sale of costly medicines- particularly anticancer, immunoglobulin, albumin, factors, sutures, rabies vaccines etc. 2. Reduction in opening of new retail drug shop/ increase in closing of retail drug shops. 3. Reduction of patient load to private hospitals and that too low socioeconomic group the POORER are benefited more. 4. Decreased private drug sales 70% in rural areas 30-50% in districts 15-20% cities 5. Highly Cost Effective Procurement of Drugs, medical devices, Equipments and consumables for Govt Hospitals 6. Implementation of MNDY – a landmark in the History of Rajasthan 7. Prescribing by generic names – a revolution. 0 to 100 % Shift towards generic prescription 8. Abundant suppliers – Enormous competition 9. Stringent Quality Control – won the confidence of Medical practitioners and people. A model against counterfeiting practices. 10. Continuous & adequate supply 11. Some charitable hospitals procure drugs from RMSC and provide free to patients. SCALABILITY AND CHALLENGES FACED The scheme has been launched with a noble cause and hence received acclaim and recognition nationally and worldwide. The sole objective was to address access and affordability to essential medicines and same has been achieved through the scheme’s mandate. The scheme can definitely be scaled up to other states and regions of the country. Officials from WHO and 14 states have also visited the state to study the Rajasthan model and replicate it in their states. The GoI has also taken note of the scheme’s success and plans to implement it across the country as it has been made part of NRHM. Funds for the scheme have already been provisioned under the NRHM so that a holistic healthcare package is available to the entire population. Challenges faced and addressed: Change in attitude of prescribers Logistics management at DDWs – space, equipment, furniture, WIC etc. Placing skilled manpower in place – Pharmacists at DDWs, Sub-stores and DDCs for dispensing and inventory management Efficient Quality Control mechanism at state HQ Dedicated and user friendly IT software for inventory management Computerization upto PHCs (at all DDW, Sub-stores and DDCs) for managing inventory related records Timely payments to suppliers is essential Efficient Supply chain management and effective monitoring of excess and shortage medicines in the field Proper annual demand generation Cold chain maintenance (in summer temp rises to 51 c) Population- 6.8 million population - longer waiting times Supply should be un-interrupted No scarcity of Pharmaceutical manufacturers Need for Supplementary methods of procurement Alternate supplier for each drug CONCLUSION The scheme is a venture for increasing access of the state’s entire population to essential generic medicines and has succeeded considerably in reducing the out of pocket expenditure on medicines The innovation has indeed been rated as one of the exceptional steps towards increasing access to medicines and will go a long way in the medical history of the state as a harbinger towards equity in healthcare. RMSC motto ALL ESSENTIAL MEDICINES AT ALL PUBLIC HEALTH INSTITUTIONS AT ALL TIMES So that No Human Being dies for Want of Medicine FREE DIAGNOSTIC SERVICES IN RAJASTHAN “MUKHYAMANTRI NISHULK JANCH YOJANA” 1. PROBLEM STATEMENT Good quality healthcare is a basic fundamental right of people and should be made available to all. India is a poor country and the onset of any illness in the family is not less than a night mare for a poor family. Out of pocket expenditure on health leads to poverty, misery and loss of invaluable human lives. This is preventable. There are four Essential Components of Health Services Component of health service Provision Hospital infrastructure provided free Consultation by a doctor & nursing care provided free Drugs, Surgical and sutures items provided free Diagnostic Services were paid These Services are available at the token money for registration at OPD for Rs.2/- or Rs.5/and in IPD for Rs. 10/-. Patients had to pay only for tests whereas other components were provided free of cost in government hospitals. If diagnostic services were made available at all hospitals without fees then it will be a step further towards the “Right to Medical Treatment” for the people of Rajasthan. Diagnostic facilities is one of the most important components of the treatment and play a critical role in all disease control and prevention program by providing timely and accurate information for use in patient management. Some diagnostic services are already being provided in govt. hospitals. Patients can undergo these tests by making payment as decided by the RMRS of the institution. For specific categories of patients like BPL these are already free. These constitute a significant number of total tests performed. Scenario prior to launch of MNJY Services available at the token money for registration at OPD for Rs.2/- or Rs.5/- and in IPD for Rs. 10/ Patients pay only for tests whereas other components are provided free of cost 2. PROGRAM DESCRIPTION Vision - To provide quality essential diagnostic services in all the government health care institutions and contribute to fundamental right to health. Mission - To strengthen the existing laboratories and other diagnostic facilities (and to create additional facilities if required) in all the public health institutions so as to provide the essential diagnostic services free of cost to all patients visiting government hospitals. To meet gaps and to provide quality diagnostic services adequately equipped diagnostic facilities are proposed as package at various levels of health care. S.No. Level of care Medical Institutions No. of free tests 1 Tertiary MCH (28) 70 2 Secondary 3 Primary DH/SDH/SH (57) CHC (431) PHC(1610) Dispensaries (198) 56 37 15 Outcome Objectives 1. To strengthen and modernize the existing laboratory facilities at PHCs, CHCs, Sub District Hospitals, Satellite Hospitals and District Hospitals by establishing the modern diagnostic laboratories. New equipments & manpower would be added to the same lab. Additional labs may be required at few district hospitals with very high patient load. 2. To provide X-Ray and ECG services essentially at the CHCs, SDH/SH/DH. 3. To strengthen, upgrade & modernized the Medical College Hospital laboratories so that they work efficiently as referral laboratories for patients referred from primary and secondary level medical institutions. Additional labs may be required to meet out the extra work load. It could also be met out by outsourcing of services. 4. To keep these labs optimally functional so that the required number of quality diagnostic test services are available at all times in all govt. hospitals. BASIC COMPONENTS FOR STRENGTHENING AND MODERNIZATION OF LABORATORIES (1)Infrastructure The renovation of existing infrastructure, need based new space addition, manpower management, equipment repair and additional demand procurement and supply of chemicals, reagents and consumables are the building stones of the scheme. Civil works were carried out for laboratories as follows: Civil Works for Laboratories to be established at health institutions Repairs & renovation of adjusting laboratories. Need based additional civil work/space at DH/MCH. Construction of shelves & cabinets to store reagents Platform, basin, sink and other sanitary fittings Counters for sample collection and report dispatch Equipment installation civil work. Chair, Table, Racks, Almirah etc. Refrigerator, UPS etc. (2)Manpower Presence of right person at the right place with the right skills is one of the major managerial principals. In the health sector the availability of skilled and trained manpower and their optimal utilization along with the available resources is the key to success of any scheme. The scheme entails - Utilization of existing staff after sensitization & training (MOs and LTs) New recruitment (need based) and training. Contractual recruitment through RMRS. Computer operators. Training of other cadres – ANMs, MOs, LTs (3) Equipments & Infrastructure The use of latest technology and quality of diagnostic services depends upon the technical specifications of equipments, instruments and appliances being procured for diagnostic centers. A team of technical committee comprising of experts from Pathology, Bio-Chemistry and Micro Biology examined and prepared the specifications of all the equipments and machines. Equipment Maintenance and Repair Workshops will be set-up at state & zonal level and would ensure the following – Gap analysis and procurement of new equipments. Equipment maintenance and repair. Utilization of existing equipments after one time repair X-Ray Machine Semi Auto Analyzer ECG Machine Three part hematology Analyzer (CBC) Back up of Equipments A provision of backup equipments at all labs has been ensured by concerned MOIC at MCH/DH/SDH/SH. Additional equipments to redress the problems of failure and maintenance shutdown have been readily made available at all laboratories (4) Supply of Reagents and Consumables Reagent and consumables have been procured by the institutions at their level for initial period of three month after which these will be made available by RMSC. LIST OF FREE INVESTIGATIONS (FOR DISTRICT/SUB DISTRICT/SATELLITE HOSPITALS) S. N 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 of Test ClinicalName Pathology Hemoglobin Estimation (Hb) Total Leukocyte Count (TLC) Differential Leukocyte Count (DLC) MP (Slide Method) ESR Bleeding Time (BT) Clotting Time (CT) PBF CBC Blood Group (ABO-RH typing) Total Eosinophilic Count (TEC) Bio Chemistry Blood sugar Blood Urea S. Creatinine S. Bilirubin (T) S. Bilirubin (D) SGOT SGPT S. Alkaline Phosphates S. Total Protein S. Albumin S. Calcium S. CK - NAC S. CK - MB S. LDH S. Amylase S. Uric Acid Microbiology S. CRP VDRL Rapid Test HIV Rapid Test Sputum for AFB Widal SlideTest Dengue (Rapid) Test Malaria by Card Test Rheumatoid Factor (RF) ASLO HBsAg (Rapid) Test Urine Analysis Urine Complete Urine Pregnancy test (UPT) Urine Microscopy Stool Analysis Stool for OVA and cyst Cardiology ECG Radiology X-Ray USG LIST OF FREE INVESTIGATIONS for CHC level. S. N. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 Name of Test Clinical Pathology Hemoglobin Estimation (Hb) Total Leukocyte Count (TLC) Differential Leukocyte Count (DLC) MP (Slide Method) ESR Bleeding Time (BT) Clotting Time (CT) CBC Blood Group (ABO-RH typing) Bio Chemistry Blood sugar Blood Urea S. Creatinine S. Bilirubin (T) S. Bilirubin (D) SGOT SGPT S. Alk. Phos S. Total Protein S. Albumin Micro Biology VDRL Rapid Test HIV Rapid Test Sputum for AFB Widal SlideTest Urine Analysis Urine Sugar/ Albumin Urine Pregnancy test (UPT) Stool Analysis Stool for OVA and cyst Radiology X-Ray Cardiology 28 ECG 31 DESIGNING & SETTING UP OF LABORATORIESD 1. , Infrastructure/Space requirements Location- Existing lab space will be used for free investigation purpose Section/Compartments of Laboratory and size The present laboratory space has been divided through partition by aluminium into sample collection corners and testing equipments, storage of reagents/chemicals and records. Reception Counter with window outlets-one for patients coming for investigations and another for report collection (Aluminium or glass cabin) Waiting space Toilets for urine collection. 2. Man Power at District/Satellite Hospital Laboratory Staff Medical Officer (Pathology/Microbiology) -1 Medical Officer (Radiology) -1 Lab Technician -6 Lab Attendant -3 Computer Operator -2 Helper/Cleaner -2 Radiographer -3 ECG Technician -4 3. Investigation/Diagnostic Equipments 1. Glucometer 2. Sahli’s Hemoglobinometer 3. TLC pipettes Neubauer’s chamber 4. Binocular microscope 5. Disposable ESR Cup 2ml with stands 6. Refrigerator 7. Five part hematologic analyzer 8. Incubator 9. Centrifuge machine 8 tubes 10. Needle & syringe destroyed 11. Fully automatic chemistry analyzer 12. Serological water bath 13. X-ray Machine 14. ECG Machine 15. USG Machine 4. Reagents/Material Required for Investigation 5. Glucostrip 6. Pregnancy Test Card 7. Urine Strips for Albumen and Sugar 8. VDRL rapid kit 9. HBsAg rapid kit 10. Widal Test Kit 32 11. Dengue rapid kit 12. Malariya antigen kit 13. RA Factor Kit 14. ASLO titer kit 15. HIV rapid Kit 16. Prothrombin Test Kit 17. Leishman’s Stain, Buffer for leishman’s Stain 18. Anti-A, Anti-B and Anti-D for Blood Group 19. Trisodium citrate 3.8% 20. Z.N. Kit for AFB 21. Lancet, Disposable gloves , spirit, Cotton roll, Gauze roll, Instrument tray with cover , Disposable Syringes, Tourniquet, Blood Collection tubes (Vaccutainer) 22. Glass Slides, Urine/Sputum container plastic, cover slips, Filter Paper, wBC pipettes, Neubauer’s Chamber, Capillary Glass tubes 23. Phenyl, 2.5% sodium hypochlorite, Biomedical waste bags and bins 24. ECG roll X-ray films.Jelly for sonography, tissue paper 25. Reagents for 3 part hematology analyzer 26. Reagents for semi automatic chemistry analyzer (blood sugar, urea, creatinine, LFT, cholesterol,LDL, Uric Acid, GGT, calcium, amylase, lipase, LDH, CK-NAC, CK-MP) Other important issues have also been addressed - 1. Quality control - quality policy has been developed and its compliance will be ensured by. establishment of Quality Assurance Program Implementation Unit at state level at RMSC, at zonal level at medical colleges and at district hospitals in the districts' 2. Bio-safety - Standard Operating Procedures (SOPs) for healthcare workers will be developed and issued and personal protective gear for bio-safety will be provided to ail laboratory staff. 3. BMW Rules implementation - all healthcare institutions are legally bound to implement BioMedical Waste (Management & Handling) Rules (1998 amendment 2000 &.2043) and it will be the responsibility of medical office in-charge to ensure disposal of laboratory generated bio-waste as per rules and obtain Common Treatment Facility(CTF) connectivity. 4. Provision for back -up equipments - all medical officer in-charges to ensure stand by invertors and generators for emergency times as also additional standby equipments. 5. Patient friendly services - ensure proper waiting space, shed, counter for registration,sample and report collection such that the patients do not have to wait for more than 10 minutes at these counters. Medical college hospitals to ensure availability-v of online report of diagnostic tests. 6. Display Boards - of list of available tests outside the laboratories (on blue background with white letters) and also board indicating time of sample and report collection. 7. Ensure 24x7 lab services -for intensive Care Units (ICU), in patients department (IPD) emergency/casualty and other serious patients at MCH, DH, SDH and SH. 33 3. IMPACT OF THE PROGRAM All patients coming to government healthcare institutions are availing the free diagnostic services at medical college and district hospitals/satellite hospitals and sub-divisional hospitals irrespective of their status of income. A 25% increase in the OPD has been observed .Till date approximately 90 lakh patients have been benefitted at these institutions. The scheme has been launched at CHCs from 1st July, 2013 and will cater to a large population of the state, were the number of investigations being provided free are 28 in numbers; similarly the scheme will take off at PHCs on 15th August, 2013 with 15 tests. Thus all levels of healthcare have been covered in implementing this scheme and the state has become the 1st in the country to provide diagnostic services free to its entire population. However, as the period of implementation is too short the impact can be observed only after a considerable gap of time 4. SCALABILITY AND CHALLENGES FACED The scheme can be scaled up in other states of the country as well, taking learning’s from the state of Rajasthan so that the approach /road map is more defined and bottle necks can e addressed prior to launch of the scheme in any of the states and regions. 5. CONCLUSION The scheme has definitely been able to further reduce the gap of affordability and accessibility to health services in the state; however it will bring results only after a period of implementation of 6 months-one year. Rajasthan Medical Services Corporation Gandhi Block, Swasthya Bhawan, Tilak Marg, C-Scheme, JAIPUR Ph:- 0141-2228066, Fax: 2228065, email: rmsc@nic.in Website : www.rmsc.nic.in 34