Integrating Prevention, Control and Therapy for Viral Hepatitis: The
advertisement
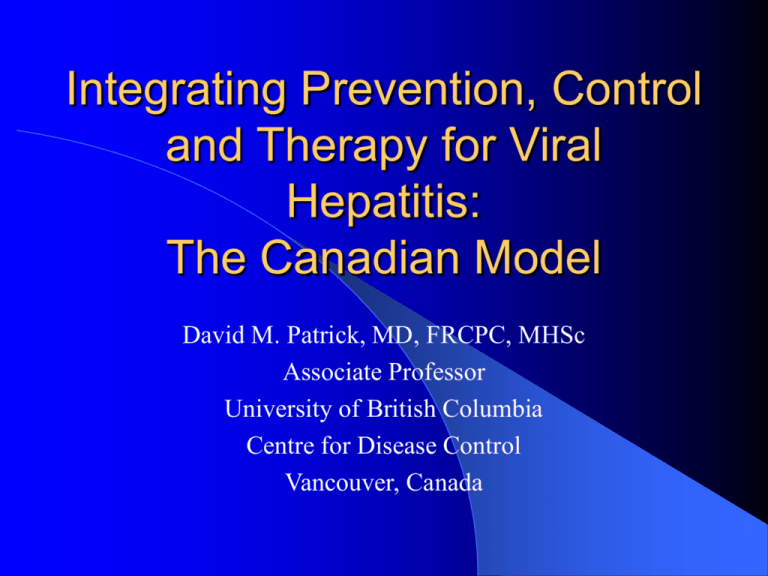
Integrating Prevention, Control and Therapy for Viral Hepatitis: The Canadian Model David M. Patrick, MD, FRCPC, MHSc Associate Professor University of British Columbia Centre for Disease Control Vancouver, Canada Rationale for Integration R = ßcD ß is the risk of transmission per contact c is the number of contacts per unit time D is the duration of infectiousness •Acting on any one variable may not be enough. •Ignoring the infected is not defensible. Control Strategies Contact Rate - c – Health Promotion safer sex substance use – Blood safety – Regulation of food and water sources – Occupational Health practices – Travel Clinics – Macro-economics Transmission Risk-ß – Immunization – Isolation methods Barrier Methods – gloves / condoms Precautions around Parenteral Exposures – Hygiene Control Strategies - D Treat and cure the infection – Screening – Diagnosis – Contact Tracing Non-curative treatment which eliminates infectiousness Model for an Integrated Hepatitis Approach Consistent screening/ testing supplemented by epidemiological studies Link test results to clinical follow-up and management records Integrated prevention and care management Measure outcomes Improvements in Process Prevention & and Care Research Updated & evaluated guidelines for prevention and management Information on drivers of incidence. Modification of prevention programming National Level Organizations Health Canada Canadian Viral Hepatitis Network Canadian Liver Foundation National Level Links: Canada Health Protection Branch Blood Regulation Organ Regulation Health Promotion and Programs Branch Hep Compensation Dept Canadian Blood System BLOOD SAFETY Blood-Borne Pathogens includes CABBI Winnipeg Labs Hepatitis CJD and Genetics Cancer Bureau Cancer and Blood HIV Bureau Retrovirus Surveillance National Laboratory Winnipeg: •Reference centre for Public Health •Development of new diagnostic tests for hepatitis •In collaboration with Medical Devices therapeutics for lot releases for new hepatitis kits •Quality Assurance and Quality Control for evaluation of panels in hospital laboratories and blood system •Centre of Excellence for new viral hepatitis & BBP Community Acquired Blood-Borne Infections Section Mandate: Surveillance, risk assessment, prevention and control of viral hepatitis and emerging blood-borne pathogens Activities: - - Surveillance Targeted research Knowledge synthesis, analysis and policy development Recommendations on prevention and control Surveillance for Viral Hepatitis and Emerging Blood-Borne Pathogens in Canada Enhanced surveillance – is a sentinel health region surveillance system for acute hepatitis B and acute hepatitis C – consists of 6 municipalities, approximately 16% of Canada’s population – provides data on incidence of acute hepatitis B and hepatitis C and transmission patterns Acute Hepatitis B Incidence 2000 7 Per 100,000 pys 6 5 4 3 2 1 0 <15 yrs 15-29 yrs 30-39 yrs 40-59 yrs Male Female *Data from 4 sites, 11% of Canadian population Total 60+ yrs Total Acute Hepatitis C Incidence – 2000* 8 Per 100,000 pys 7 6 5 4 3 2 1 0 <15 yrs 15-29 yrs 30-39 yrs Male 40-59 yrs Female Total *Data from 4 sites, 11% of Canadian population 60+ yrs Total Enhanced Surveillance Risk Factor Information Substance use most important risk factor for hepatitis C, significant for hepatitis B Risky sexual behaviour important risk factor for hepatitis B, especially among gay and bisexual men Significant proportion of cases have no known risk factor Percent of case Ethnicity of Hepatitis B and C 100.00% 90.00% 80.00% 70.00% 60.00% 50.00% 40.00% 30.00% 20.00% 10.00% 0.00% Aboriginal Afroamerican Asian Hep B *Vancouver cases April 1, 2000-March 31, 2001 Caucasian Hep C Other Unknown Surveillance for Viral Hepatitis and Emerging Blood-Borne Pathogens in Canada Hospital Surveillance Centres and the Canadian Viral Hepatitis Network Sentinel Regions Surveillance: – less effective in assessing the burden of disease – difficult to follow up the natural history Applications of Hospital Based Surveillance: – Blood-borne pathogens and chronic diseases – evaluation of medical practices as well as interventions – education, counseling and other public health functions Integrated Approach Clinical Data Laboratory Data • prevalence Required Knowledge • natural history (Scrambled Data) Vital Statistics Population Health/ Policy Requirements Billing Data • intervention effectiveness • economic burden Canadian Viral Hepatitis Network • representation from provinces/territories, non-government organizations, Statistics Canada, CIHI, academics/clinicians and the Centre for Infectious Disease Prevention & Control Population & Public Health Working Groups Infectious Diseases Expert Advisory Groups • input on issues and priorities to Steering Committee/Working Groups Technical Working Group Secretariat Support • data & data management expertise • statistical expertise • provided by Health Canada Canadian Liver Foundation Established 1969 supports research public information and education – living with liver disease programs – help-line – pamphlets – awareness programs #S #S #S Annualized Rate of HCV by Service Area/Centre (per 100,000 population) & V & V & V British Columbia < 100 100 - 200 > 200 Rural and Semi-Urban Community Reporting HCV #S Below BC Mean #S Above BC Mean #S #S #S #S #S N #S #S #S #S S # #S BC Health Authorities Interior NORTHERN E W Fraser S Vancouver Coastal #S #S#S Nisga'a #S #S Sources: Vancouver Island Hepatitis C data are from Epidemiology Services, BC Hepatitis Services and Laboratory Services divisions of the BC Centre for Disease Control. #S #S Northern Population figures are from the Statistical Profile of Canadian Communities, Census 1996, Statistics Canada. #S #S Nisga'a #S # S #S Note: The Nisga'a Health Council will remain an independent health authority. Geographic data are from BC STATS, BC Ministry of Finance and Corporate Relations. #S #S #S #S #S #S #S #S & V Prince George #S #S #S Explantion of Spider Diagram Analysis: #S #S On this map, all rural, semi-urban and urban communities with populations less than 25,000 are assigned to the closest "service centre". A service centre is defined as an urban community with a population of 25,000 and greater, and has clinical services to provide HCV treatment. #S #S #S #S The annualized HCV rate reported on this map represents the cumulative rate of HCV of all communities within the service area. The mean annual HCV rate from 1992-2000 is 106.4 cases per 100,000 population for BC. #S #S #S #S #S #S #S INTERIOR #S #S West Vancouver FRASER North Vancouver COASTAL #S #S Port Coquitlam #S &V V &V & V &&V & V &&V V & &V V & V & V & V & V #S Maple Ridge Mission # # #S #S S # #S S #S #S #S #S S # #S #S #S #S S Delta # #S # # #S #S #S #S Vancouver # # #S #S #S #S # & V Richmond #S Chilliwack # #S #S Duncan #S #S ##S S # Nanaimo VANCOUVER ISLAND #S #S #S Burnaby & V #S # S Surrey #S Abbotsford ##S#S S #S 20 ##S S #S 0 20 Kilometers & V Southwest BC Inset Map #S #S Victoria #S #S #S #S COASTAL #S & V & V #S #S#S #S Campbell River VANCOUVER #S #S #S #S ISLAND #S #S #S #S #S # S #S & V & V & V #S #S #S # S FRASER #S #S #S #S #S#S #S #S#S # S #S #S#S#S#S#S #S S ##S#S #S #S#S #S #S #S && V &V V &V && V &V & V & V V &V &V &V && V V & V & V #S #S #S #S #S #S #S #S #S #S #S #S #S #S #S #S #S #S #S #S #S ##S #S S #S #S #S #S #S#S # S #S # S #S #S #S Vernon #S #S #S #S #S Kamloops #S #S #S #S # S #S VANCOUVER #S New Westminster #S #S #S Langley #S #S #S #S #S #S Coquitlam #S #S #S ##S S #S #S VANCOUVER #S #S Kelowna #S #S #S #S #S ##S #S S #S #S # #S S #S #S #S #S #S #S Penticton #S #S #S #S #S #S ##S S #S #S #S#S #S#S #S # S #S 200 0 Kilometers See Southwest BC Inset Map 200 Goals of BC Hepatitis Services •Optimal Surveillance •Evidence-based Prevention • Care Management •New, effective, & expensive drugs that improve outcomes are they cost-effective? Population Individual Was a Centre for Excellence the Answer? British Columbia Centre for Disease Control Communicable Disease Control Epidemiology Microbiology Clinical Services Surveillance Public Health Information System Transfusion Transmitted Infection Reporting Laboratory Linkage – testing, PCR and genotyping at the BCCDC – bar-coded labels for specimens link provider, patient and outcome – pilot treatment cohort tracking system Specific Studies – seroprevalence; enhanced surveillance – IDU and MSM cohorts Hepatitis A Prevention Hygiene Food Inspection Travel Advisories Immunization – – – – High Risk (MSM, IDU) Chronic Liver Disease Targeted Blitzes Contacts and Outbreak Control Hepatitis A in Canada and B.C. Rate per 100,000 population 30 25 20 BC Canada 15 10 5 0 92 93 94 95 96 97 98 99 0 1 Reported Hepatitis A Vancouver 19972001 – Risk Factors MSM 30 Vaccination Campaigns 25 SROs 15 10 5 IDUs Unknown Dr. Patricia Daly Contact Travel DTES/IDU MSM Oct-01 Jul-01 Apr-01 Jan-01 Oct-00 Jul-00 Apr-00 Jan-00 Oct-99 Jul-99 Apr-99 Jan-99 Oct-98 Jul-98 Apr-98 Jan-98 Oct-97 Jul-97 Apr-97 0 Jan-97 Cases 20 Immunization for Hepatitis B High Risk since 1980’s Age 11 since 1992 – But routine pre-natal screening and readily available HBIG and birth dose Infants since 2000 Hepatitis B in Canada and B.C. Rate of Acute Disease per 100,000 population 12 10 8 BC Canada 6 4 2 0 92 93 94 95 96 97 98 99 0 1 Hepatitis B Age-group 11-20 Cases of Acute Disease per 100,000 population 25 20 15 BC 10 5 0 92 93 94 95 96 97 98 99 0 Antenatal Seroprevalence of Anti-Hep B core, 1999 Percent Reactive 20% 18% 16% 14% 12% 11.1% 11.9% 10.4% 10.4% 10% 7.4% 8% 6.5% 5.2% 6% 4% 2% 0.0% 0.7% 1.5% 0.0% 0% Age Group 15-16 17-18 19-20 21-22 23-24 25-29 30-34 35-39 40-44 Total 43 41 39 37 35 Total Age 33 31 29 27 25 23 21 19 17 90 80 70 60 50 40 30 20 10 0 15 IU Geometric Mean Titre for anti-HBs by Age Hepatitis C Prevention Blood screening Harm Reduction – street nurses – NEP (no parephenalia stuff) – No safe injection sites but starting Hepatitis C in Canada and B.C. Rate per 100,000 population 250 200 150 BC Canada 100 50 0 92 93 94 95 96 97 98 99 0 1 Vancouver Injection Drug User Cohort 100 HIV 80 HCV 60 40 20 0 Dec 96 May 97 Jun 97 Nov 97 Dec 97 May 98 Jun 98 Nov 98 Dec 98 May 99 Jun 99 Nov 99 HIV 19.4 6.0 2.5 2.5 3.4 2.0 HCV 64.8 27.2 23.4 28.9 20.7 16.7 Chronic Viral Hepatitis Therapy Funding not a huge problem Catering to patient population is Type distribution – Hep C 65% 1; 35% non 1 mostly 2&3 Consumer advocacy is building Specific Efforts for Street Involved including pilot integrated treatment clinics in each region Hepatitis B Therapy Lamivudine still not curative coverage for one year (case by case review thereafter) e ag pos and pre-core mutants Issues of Importance when Developing Education Programs Identified by Provincial Hepatitis Advisory Committee need for consumer & professional education nursing education to support advanced practice include co-infection with HIV & chemical dependency professional & consumer involvement in development of curriculum & materials broad representation on advisory committee Challenges Funding of IT Multiple blood-borne infections in marginalized populations – eg. substance use Historic problems and marginalization for First Nations (Aboriginal Groups) Immigration Trend to reduced spending on social issues Global Context Vaccines are still job one WHO coverage assessments – not operational yet Rapid tests and treatment – We’re not so sure – Cost efficacy – Rx good value but not like vaccine Where next? Better linkage of public health and treatment Health Care Worker Education Nurse practitioners Integrated drug and hepatitis Rx Broader population programs for Hepatitis A immunization? Acknowledgements Mel Krajden, Gail Butt, Warren Hill Tony Giulivi, Leslie Forester Patricia Daly