Sterilization
advertisement

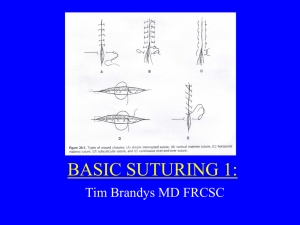
Sterilization By: Dr. Yasser El Basatiny Prof. of Laparoscopic Surgery Antisepsis • Definitions: Antisepsis = against putrefaction To eliminate or reduce the germs • Antisepsis: use of antimicrobial chemicals on human tissue • Disinfection: use of antimicrobial chemicals on inanimate objects Historical background • In 18th and 19th century , serious infections among hospitalized patients, morbidity and mortality was very high nearly all trauma and surgical wound got infected and suppuration • Hand wash and clothing change policy reduced maternal mortality from 11.4% in 1846 to 1.3% in 1848 • Pasteur’s discovered bacterium and it’s role in wound infection. • Lister published 1st antiseptic principle in 1867 • Kocher reported 2.3% infection rate in clean wound by 1899. Aseptic technique • • • • • • • Hygienic hand wash Preoperative preparation of patient’s skin Gloving Sterile draping Isolation precaution Autoclaving of instruments Proper waste disposal Principles of sterilization Operating room: • Minimum size is 5x5 meter • Appropriate ventilation, changing room air 20 to 25 times per hour. • Passing inflow air through “high efficiency particulate air” HEPA filter • All doors of OR. should be closed • Air pressure should be positive The primary source of perioperative infection is the patient and the secondary source are the OR team A CFD simulation of a Cleansuite installation in an operating room shows laminar air flowing from diffusers in the ceiling, down and away from the patient, and out vents near the floor Patient as a source of infection Wounds: • • • • Clean wounds Clean contaminated Contaminated Dirty Intrinsic resistance to contamination • Age, obesity, diabetes, cirrhosis, uremia and immunodeficiency. Methods of sterilization • Iodophors (Betadine) broad spectrum antimicrobial against fungi, viruses, gram positive and gram negative. Operative team • Scrub the hands and arms with antiseptic solution like iodophors and chlorhexidine • Face mask over the mouth and nose, head cover and shoe covers • Disposable sterile gloves • Sterile gown: impermeability to moisture. • Sterile drapes impermeable to bacteria Methods of sterilization • Steam heat (Autoclave) • Chemical solution: used for instruments tolerate moisture but not heat. 2% glutaraldehyde • Dry heat: for items can tolerate heat and not penetrated well by steam • Gas sterilization: for delicate instruments Autoclave sterilizer Surgical technique Gentle handling of tissues, careful hemostasis and appropriate irrigation. • Incisions: along normal skin line, adequate exposure, same incision in reoperation • Atraumatic handling: minimize necrosis of skin margin • Dissection: least amount of trauma in dissecting in natural tissue planes • Debridement: the most important single factor in management of contaminated wounds Surgical technique • Hemostasis: to minimize blood loss and prevent hematoma formation • Wound closure: primary closure for clean wounds, delayed primary closure should be considered on or after 4th day in contaminated wound • Suturing: simple interrupted sutures, mattress suture, subcuticular suture Surgical technique • Dressing: protect the wound from mechanical trauma and bacterial invasion, sterile dressing applied before removal of drapes, moist dressing speed up epithelization 10 folds, infected wounds needs dressing that absorb exudates. • Immobilization: it reduce lymphatic flow and minimizing the spread of wound flora, more resistance to bacterial growth, elevation reduces interstitial edema. • Suture removal: proper timing for suture removal • Prophylactic antibiotics: before skin incision Operative equipments Electrocautery: • High frequency alternating current • For hemostasis and incise tissue • Unipolar, rapid dehydration of the cell and the blood vessels within the tissue coagulate • Bipolar, more precise and confines the damage to the tissue between the tips of forceps Operative equipments Argon beam coagulator (ABC): • For parenchymatous organs, unipolar coagulation non touch technique. Less depth of penetration 2-3 mm Surgical lasers: • Argon Laser, ophtalmogic tratment and vascular anastomosis. • CO2 Laser, to cut tissue • Nd:YAG Laser, flexible quartz fiber can be used for paranasal sinus and tracheobronchial tree • Er:YAG Laser, very strongly absorbed by the water of tissue can vaporize cartilage, fibrous tissue and bone Harmonic scalpel • Use of ultrasonic power for cutting and coagulation Sutures and needles Needles • • • • Open French eye needle Swaged on needle (eye less) Straight or curved Cross section: can be round triangular or flattened • Needle point: cutting, tapered or blunt Sutures and needles Absorbable sutures • Absorption and disappearance of the suture from the tissue implantation site • Catgut: made from the intestine of cattle or sheep, absorption of plain catgut is about 10 days. Chromic catgut (treated by chromium salt) its absorption is delayed up to 20 days. • Polyglycolic acid (Dexon): absorbable braided, synthetic suture, higher tensile strenght, reabsorption by hydrolysis at 60 to 90 days. • Polyglyconate ( Maxon): synththetic monofilament. • Polyglactic acid (Vicryl): braided synthetic suture, very high tensile stenght, absorbed in 60 days • Polydioxanone (PDS): monofilament absorbable Sutures and needles Non absorbable sutures • Silk: protein filament from the silkworm larva, dyed, treated by polybutilate and braided. Good tensile strength • polyester (Dacron): superior strength and durability • Nylon: synthetic polyamide polymer, monofilament and multifilament. • Polyprolene (Prolene): monofilament, minimal tissue reaction • Stainless Steel: low carbon iron alloy, monofilament or multifilament. Used for bone suturing Sutures and needles Staplers • TA Instruments: linear everting double line, length 30, 55, 90 mm. staple size 3.5 and 4.8 mm. 3.2 mm for vessel closure. • GIA Instruments: two double rows of staples and divide the tissues in between. • EEA Instruments: end to end or end to side circular staplers • Skin staples: speed of skin closure and efficacy. Drains Historical aspects • Dates back to Hippocrates • Metal tubes, glass tubes, bone, gauze and combination of gauze and rubber • Tapered lead and bronze tubes to drain abdominal cavity by Celsus in 1st century • Penrose drain 1890, cigarette drain 1897 • Air vent suction by Heaton 1889 Principles of wound drainage • To drain cavity or soft tissue to prevent collection of serum or blood • It is not a substitute for hemostasis or meticulous technique • Either passive or active, prophylactic or therapeutic. • It should be soft, nonirritating, firm, smooth and resistant to decomposition. Types of drains Penrose drain (obsolete) • Efficient but there is significant risk of secondary infection. • Soft, flexible latex rubber wick • To drain purulent material, blood or serum from body cavity • Brought out through a separate stab at dependant area • Anchored to the skin with a non absorbable suture Types of drains Closed suction drain • Lower infection rate, might clog and cease function • Firm multi-holed catheters made of polyvinyl chloride or silicone. • Effective to drain soft tissue under large skin flaps Types of drains Sump drain • Large and bulky • Double or triple lumen allow irrigation and aspiration • Rely on continuous flow of air from outside predisposes to secondary infection. • Less likely tissue occlusion • For high volume enteric fistula Types of drains Closed suction Penrose drain • Combination of closed suction drain and Penrose drain which uses capillary action • Low secondary infection, effective in abdominal cavity • Ideal drainage system Percutaneous catheters • Inserted by radiologists CT or US guided to drain accessible localized collection Minimal invasive surgery • • • • Laparoscopic surgery Thoracoscopic surgery NOTS “natural orifice transluminal surgery Single port laparoscopic surgery Minimal invasive surgery • To reduce tissue injury, fast post operative recovery, short hospital stay • Pneumo-peritonium to create room to work Thank you