NUTRITION Nursing Implications
advertisement
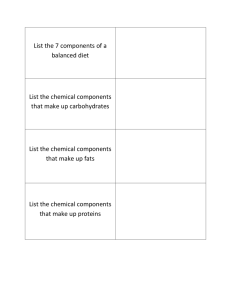
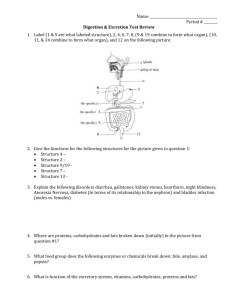
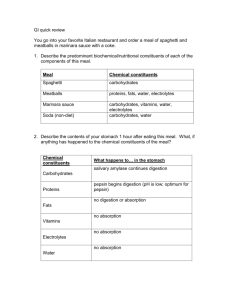
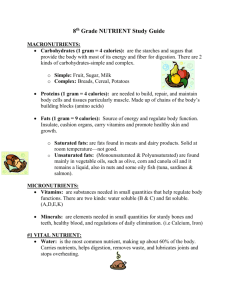
NUTRITION Nursing Implications 1 Nutrition • All of the processes involved in consuming and utilizing food for energy, maintenance, and growth. Physiology of Nutrition Five processes are involved in the body’s use of nutrients: – – – – – Ingestion. Digestion. Absorption. Metabolism. Excretion. Ingestion • The taking of food into the digestive tract, generally through the mouth. Digestion • The mechanical and chemical processes that convert nutrients into a physically absorbable state. Digestion includes: – Mastication (chewing). – Deglutition (swallowing). – Peristalsis (coordinated, rhythmic, serial contractions of the smooth muscles of the GI tract). Absorption • The process by which the end products of digestion pass through the small and large intestines into the blood or lymph systems. Metabolism – The body’s conversion of nutrients into energy. – Basal metabolism is the amount of energy needed to maintain essential physiologic functions when a person is at complete rest, both physically and mentally. Excretion – The process of eliminating or removing waste products from the body. The Six Essential Nutrients • • • • • • Water Carbohydrates Fats Proteins Vitamins Minerals Water • The Most Important Nutrient. • Daily requirements: 1,000mL of water to process 1,000kcal eaten. Functions of Water • Solvent (dissolves substances to form solutions). • Transporter (carries nutrients, wastes, etc. throughout the body). • Regulator of body temperature. • Lubricant (aids in providing smooth movement for joints). • Component of all cells. • Hydrolysis (breaks apart substances, especially in metabolism). Classification & Sources of Water • Liquids consumed (water, coffee, juice, tea, milk, soft drinks). • Foods consumed (especially fruits and vegetables). • Metabolism (produces water when oxidization occurs). Water: Digestion, Absorption and Storage • Water is not digested. It is absorbed and used by the body as we drink it. It cannot be stored by the body. The body loses water in four ways: – – – – Urine. Feces. Perspiration. Respiration. Water: Signs of Deficiency • Abnormal water losses include profuse sweating, vomiting, diarrhea, hemorrhage, wound drainage (burns), fever, and edema. • A deficiency of water is called dehydration. Prolonged dehydration results in death. Carbohydrates • The chief source of energy for the body. Made up of carbon, hydrogen, and oxygen. They are the major source of food for all people. • Daily requirements: 50% to 60 of an individual’s kcal intake per day. Functions of Carbohydrates Carbohydrates are... • The primary source of energy for the body. • Spares proteins from being used for energy, thus allowing them to perform their primary function of building and repairing body tissues. • Needed to oxidize fats completely and for synthesis of fatty acids and amino acids. Carbohydrates: Classification and Sources • Carbohydrates may be simple or complex. • Simple are single or double sugars. • Complex are composed of many single sugars joined together (starch, dietary fiber, glycogen). Carbohydrates: Digestion, Absorption and Storage • Digestion of cooked starches begins in the mouth. • Little digestion occurs in the stomach. • Carbohydrate digestion completed in the small intestine. • Carbohydrates are used completely, leaving no waste for the kidneys to excrete. Carbohydrates: Signs of Deficiency • Mild deficiency can result in weight loss and fatigue. • Serious deficiency can result in ketosis. Fats • The most concentrated source of energy in the diet. An essential nutrient, but too much can be a health hazard. • Daily requirements: should not exceed 25% to 30% of an individual’s caloric intake per day. Functions of Fats • Provides concentrated source of energy. • Assists in absorption of fat-soluble vitamins. • Is a major component of cell membranes and myellin sheaths. • Improves flavor of foods and delay’s stomach’s emptying time. • Protects and hold organs in place. • Insulates body, thus assisting in temperature maintenance. Classification of Fats • Triglycerides (true fats). • Phospholipids (lipoids, composed of glycerol, fatty acids, and phosphorus). • Cholesterol. Sources of Fats • Animal (lard, butter, milk, cream, egg yolks, and fat in meat, poultry, and fish). • Plant (oils from corn, safflower, peanut, palm, etc., as well as nuts and avocado). Digestion, Absorption and Storage of Fats • No chemical breakdown of fats occurs in the mouth and very little in the stomach. • Digestion occurs in small intestine. • Fats not immediately needed by the body are stored as adipose tissue. Fats: Signs of Deficiency and Excess • Deficiency occurs when fats provide less than 10% of daily kcal requirement. • Gross deficiency may result in eczema, retarded growth, and weight loss. • Excess fat consumption can lead to overweight and heart disease. Proteins • The only nutrient that can build, repair, and maintain body tissues. • Daily requirements: determined by size, age, gender, and physical and emotional conditions. • Daily protein requirement for average adults is 0.8g for each kilogram of weight. Functions of Proteins • To provide amino acids necessary for synthesis of body proteins, used to build, repair, and maintain body tissues. • To assist in regulating fluid balance. • Used to build antibodies. • Plasma proteins help control water balance between the circulatory system and surrounding tissues. • In event of insufficient stores of carbohydrates and fats, protein can be converted into glucose and used for energy. Classification & Sources of Proteins • Complete proteins contain all 9 essential amino acids. (All animal fats, except for gelatin, are complete. Only plant fat that is complete is soybeans). • Incomplete proteins have one or more essential amino acids missing (plant proteins). Digestion, Absorption and Storage of Protein • Digestion begins in the stomach. • Most digestion takes place in the small intestine. • Amino acids not used to build proteins are converted to glucose, glycogen, or fat and are stored. Signs of Deficiency and Excess of Protein • • • • Muscle wasting. Edema (swelling). Lethargy and depression. Excess can result in heart disease, colon cancer, osteoporosis. Vitamins • Essential organic compounds that regulate body processes and are required for metabolism of fats, proteins, and carbohydrates. • Needed in very small amounts. BODY WEIGHT/BODY MASS • Ideal body weight • Body mass index • Percent body fat 32 FACTORS AFFECTING NUTRITION • • • • • • • • Development Gender Ethnicity & culture Beliefs about food Personal preferences Religious practices Lifestyle Medications & therapy – table 45-1 33 FACTORS AFFECTING NUTRITION • • • • Health Alcohol abuse Advertising Psychologic factors 34 NUTRITION THRU THE LIFE CYCLE – Young & Middle Adult • Lay foundation for lifetime nutrition pattern in young adulthood • Nutrient requirements change very little • Females need to maintain/increase intake of Vit. C , Vit D, & calcium; & maintain intake of iron • Basal metabolism decreases 2-3%/decade after age 25 • Obesity, HTN , & DM may begin to form 35 NUTRITION THRU THE LIFE CYCLE – Older Adults • • • • Physiologic, psychosocial, economic changes Need fewer calories Nutrient requirements basically the same Variety & nutrient dense foods; water 36 Factors Affecting Nutrition: Ethnicity & Culture • Native American – – – – – Starches: corn, rice Fruits: berries Veggies: rhubarb, mushrooms, roots Meats: game, seafood, nuts Milk: little used • High incidence of lactose intolerance • Encourage broiled, poached, steamed meats 37 Factors Affecting Nutrition: Ethnicity & Culture • U.S. Southern – Starches: cornbread, biscuits, potatoes – Fruits: melons, peaches, bananas – Veggies: collards, okra, tomatoes, cabbage – Meat: pork, chicken, fish – Milk: milk, ice cream • Many foods fried, cooked with lard 38 Factors Affecting Nutrition: Ethnicity & Culture • Mexican – Starches: tortillas, corn products – Fruits: few – Veggies: chili peppers, tomatoes, onions – Meat: beef, poultry, eggs, pinto beans – Milk: cheese; rarely drink milk 39 Factors Affecting Nutrition: Beliefs & Preferences • Individual likes & dislikes • Beliefs about foods • Fad diets 40 Factors Affecting Nutrition: Religious Practices • Christianity – – – – Catholics Eastern Orthodox Mormons Seventh Day Adventists • Islam – No pork or alcohol; daylight fasting during Ramadan 41 Factors Affecting Nutrition: Lifestyle • Economic & social status • Work/activities 42 Factors Affecting Nutrition: Medications, Therapy, & Health • Therapies – Chemo, radiation • Health – GI disorders, viruses, oral ulcers 43 Factors Affecting Nutrition: Alcohol, Advertising, & Psych • Alcohol – Can depress appetite – Abuse can lead to malnutrition (esp Vit B) • Advertising – May influence food choices • Psych – Overeat vs. don’t eat when stressed, depressed 44 DIETARY GUIDELINES • • • • • • • • Eat a variety of foods Maintain or improve your weight Be physically active every day Eat diet low in trans fat, saturated fat, & cholesterol Eat plenty of vegetables, fruits, & grains Use sugars in moderation Use salt & sodium in moderation If you drink alcohol, do so in moderation 45 Food Guide Pyramid Fats, oils & sweets Use sparingly Milk, Yogurt & Cheese Meat, poultry, fish, dry beans, eggs & nuts 2-3 servings Vegetables & Fruits (2-5 servings) Bread, cereal, rice & pasta (6-11 servings) FOOD GUIDE PYRAMID • • • • • • • • • Healthy Eating Pyramid Daily exercise & weight control Whole grains at most meals Vegetables in abundance Fruits 2-3 times/day Nuts, legumes 1-3 times/day Fish, poultry, eggs 0-2 times/day Dairy or calcium supplement 1-2 times/day White rice, white bread, potatoes, pasta, sweets, red meat, butter sparingly • MVI for most • Alcohol in moderation 47 ALTERED NUTRITION • Malnutrition – lack of necessary or appropriate food substances – Overnutrition – caloric intake in excess of daily energy requirements • Overweight – BMI 26-30 • Obese – BMI > 30 • Morbid obesity – interferes with mobility or breathing 48 ALTERED NUTRITION • Malnutrition – Undernutrition – intake of nutrients insufficient to meet daily energy requirements as a result of inadequate food intake or improper digestion & absorption of food • Dysphagia – difficulty swallowing • Anorexia – loss of appetite • Protein-calorie malnutrition 49 The Nursing Process: Assessment Two types of data: • Subjective. • Objective. Subjective Data • • • • 24-Hour Recall. Food-Frequency Questionnaire. Food Record. Diet History. Objective Data • Body Mass Index. • Skinfold Measurement. • Other Measurements (e.g. Abdominal-Girth, Mid-Upper-Arm). • Laboratory Tests. RISK FACTORS FOR NUTRITIONAL PROBLEMS • Diet history – – – – – – – – Chewing or swallowing difficulties Inadequate food intake Restricted or fad diets No intake for 10 or more days Inadequate food budget Inadequate food preparation facilities Physical disabilities Living & eating alone 53 RISK FACTORS FOR NUTRITIONAL PROBLEMS • Medical history – – – – – – – – – – Unintentional wt loss or gain of 10% within 6 months F/E imbalance Oral or GI surgery Dental problems GI problems Chronic illness Alcohol or substance abuse Neurologic or cognitive impairment Catabolic or hypermetabolic condition Adolescent pregnancy or closely spaced pregnancy 54 RISK FACTORS FOR NUTRITIONAL PROBLEMS • Medication history – – – – – – – – – – Aspirin Antacid Antidepressants Antihypertensives Anti-inflammatory agents Antineoplastic agents Digitalis Laxatives Diuretics Potassium chloride 55 PHYSICAL EXAM • • • • • • • • • • • General appearance & vitality Weight Skin Nails Hair Eyes Lips, tongue, gums, teeth Heart Abdomen Musculoskeletal Neurologic 56 ANTHROPOMETRIC MEASUREMENTS • Height & weight • Skinfold measurements – tricep most common site 57 LABORATORY DATA • • • • • • Albumin & pre-albumin Transferrin Hgb BUN 24 hour urine Total lymphocyte count 58 DIAGNOSING • Altered nutrition: more than body requirements • Altered nutrition: less than body requirements • Altered nutrition: risk for more than body requirements • Fluid volume excess, fluid volume deficit, & risk for fluid volume deficit • Activity intolerance • Constipation • Risk for Impaired Skin Integrity 59 PLANNING • Client will: – Maintain I&O balance – Consume proper amounts of foods from variety of food groups – Comply with diet therapy – Tolerate tube feedings – Not have any complications assoc with malnutrition 60 IMPLEMENTING - Teaching • Use established nutritional standards • Use visualization of serving sizes to help ID accurate serving sizes • Incorporate culturally based intake patterns or restrictions • Include client & family • Collaborate with dietician 61 IMPLEMENTING Special Diets • NPO – nothing by mouth • Clear liquid diet – water, tea, coffee, clear broths, gingerale, plain gelatin • Full liquid diet – clears; milk; cooked cereals, pudding, ice cream, cream soup; • Soft diet – easily chewed & digested • Dysphagia – thickened liquids • Diet as tolerated 62 IMPLEMENTING Stimulating Appetite • Relieve illness symptoms that depress appetite prior to mealtime • Provide familiar food that person likes served at proper temp. • Select small portions • Avoid unpleasant or uncomfortable treatments or activity immediately before/after meals • Provide tidy, clean environment • Encourage or provide oral hygiene before mealtime • Reduce psychologic stress 63 IMPLEMENTING Assisting with Meals • • • • • • • Help client feed self when possible Assist client to sit on side of bed or chair if possible Check tray for client’s name, type of diet, & completeness “which order would you like to eat?” Spread napkin, cut foods, shell egg, etc. Do not rush client; allow ample time Offer fluids every 3 or 4 mouthfuls of food if client unable to communicate • Use adaptive feeding aids as needed • For blind person, identify placement of food as you would describe time on a clock 64 IMPLEMENTING Special Supplements • Oral – Provide calories & nutrients – Can be liquid or powdered – Specific types • Tube Feeds – When condition prevents food intake – Impairment in upper GI tract, otherwise fx GI tract – Increased metabolic needs that oral intake can’t meet • Parenteral Nutrition – IV nutrients (TPN, PPN) 65 EVALUATING Enteral Feeds • • • • Daily wt I&O Labs Monitor for complications 66 IMPLEMENTING Home Care Teaching • • • • • • • Preparation of formula Proper storage of formula Administration of feeding Mgmt of enteral or parenteral access device Daily monitoring needs S/S of complications to report Who to contact with questions/problems 67 EVALUATING • If outcomes not achieved, – Was cause of problem correctly identified? – Was family included in teaching plan? Are they supportive? – Is client experiencing symptoms that cause loss of appetite? – Were outcomes unrealistic for this person? – Were client’s food preferences considered? – Is anything interfering with digestion or absorption of nutrients? 68 TERIMAKASIH