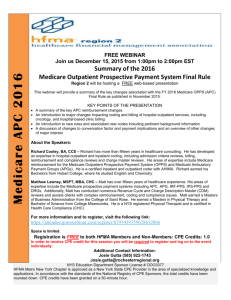
Overview of Ambulatory Payment Classifications (APCs)
advertisement
Ambulatory Payment Classifications APCs Definition • APC stands for Ambulatory Payment Classifications • System for reimbursing acute care facilities for outpatient services (e.g., Outpatient Prospective Payment System or OPPS) –Developed because of success of DRGs History of APCs • OBRA – 1986 – CMS directed to develop OPPS – 3M won bid 1988 • APGs developed by 1990 but not implemented • BBA – 1997 – CMS to implement PPS by 1999 • BBRA - 1999 • APCs implemented 2000 What are APCs?? • Outpatient Payment Groups – Groups of codes with a fixed payment amount • Based on HCPCS codes – Both Level 1 and Level 2 used • Codes in the same APC must have – Comparable clinical aspects – Comparable resource consumption Why Another Payment System? There was a rapid growth in outpatient services and ambulatory care expenditures and payments. Some of the reasons were: 1. Cost efficiency incentives in the inpatient PPS (DRGs) 2. Medicare’s 1982 decision to qualify and recognize facility payment of ASCs (Ambulatory Surgical Centers) 3. Some private insurer incentives to hospitals to treat their beneficiaries in the outpatient setting 4. The decline in inpatient revenue due to DRGs 5. Advancements in medical technology (i.e. anesthetics and laparoscopes) Purpose of APCs • • • • Cost control Efficiency Facilitate payment Address beneficiary coinsurance issues Key Aspects of APCs • Packaging – Services like laboratory (still paid on a fee schedule basis), most supplies, anesthesia, intraocular lenses, and observation care are included in the APC payment • Drugs, pharmaceuticals, and biologicals usually not bundled • Discounting – Multiple procedures provided during the same patient encounter are provided at lower cost than they would be if provided at separate encounters • Applies to services with status indicator T Key Aspects of APCs • Fixed payment rate – Hospitals and payers know in advance how much they will be paid for certain services • Three Year Transition Period – Transitional corridors allowed for a three-year period that limited the payment reductions to hospital under OPPS How Are APC Groups Created • HCPCS codes are grouped together because they have – Similar clinical aspects • Pacemakers can’t be grouped with bronchoscopies even if resource usage is similar – Comparable resource consumption • Clinically similar codes are grouped by the cost to perform the service – Two Times Rule Two Times Rule Requirement • HCPCS codes grouped into APCs based on comparable resource utilization • Median costs determined for each HCPCS code – Average cost for each HCPCS code within a specific APC • Codes are not similar if the resource costs of the highest HCPCS is more than 2 times the cost of the lowest – Exceptions example, low use codes Status Indicators • Letters assigned to each HCPCS code to indicate its payment status • Examples – “C” status indicator • Inpatient only list – “A” status indicator • Other (non-APC payment system) – “G” and “H” status indicators • Payment by pass-through – “T” status indicator • Payment under APCs and subject to multiple procedure discount Types of Services Under APCs • Service with status indicators K, S, T, V, X – Outpatient evaluation and management (status V) – Outpatient surgery (status S or T) – Outpatient ancillary services • Radiology services (status S and X) • Pathology and laboratory services (status X) • Medical testing and evaluations and injections and infusions performed in the outpatient facility (status K, S, T and X) – Certain drugs and biological (status K) • Other services and supplies are either not paid separately, not covered, or paid via other methods More About Status Indicators • Significant procedures with status (T) are paid at a reduced rate when performed with other procedures during the same visit • Significant procedures with status (S) are not discounted when multiple procedures are performed – When an S procedure is performed with other procedures, the S still receives full reimbursement • Services with a status (N) are bundle into other APCs and are considered incidental – A cardiac catheterization code drives the APC payment • Ventriculography, coronary angiography, and S&I codes are all bundled into APC for a heart catheterization Exceptions to Fixed Payment Rates • Outliers • Pass-through items • New technology Outliers • Outlier Payments mandated by BBRA-1999 • Outlier threshold – Multiply the total costs for services eligible for APC payment by an outpatient cost to charge ratio – Costs must exceed 2.5 times more than the APC payment • Less than 2.5 times more is considered standard fluctuation in cost of care – Outlier payment is 75% of the amount that the cost exceeded the payment • Originally computed per claim; now computed per service Transitional Pass-Through Payments • Additional temporary payments – 2 to 3 years • Allows evaluation of cost data for APCs • Specific drugs, devices and biologicals – Chemotherapy drugs and adjuvant and supportive drugs used with them – Immunosuppresive drugs – Orphan drugs (by FDA definition) – Radiopharmaceuticals – New medical devices, drugs, and biologic agents • Not paid as a hospital outpatient service as of 12/31/96 • And cost of the items is significant – Coinsurance may be less than 20% New Technology APCs • Specific APC groups created for new treatment technologies – Services that do not fit into any other APC • Temporary payments during assessment periods Outpatient Evaluation and Management Codes • Describe use of space in facilities • Describe use of supplies in facilities • Describe involvement of hospital employees in E/M services • Can’t Be Used If… – Patient admitted within 48 hours – Patient taken to surgery – Patient receives other global service • Example: Dialysis Codes with Status V • Only codes used in outpatient settings – Outpatient clinic • • • • • Office or Other Outpatient Service (99201 – 99215) Office or Other Outpatient Consults (99241 – 99245) Confirmatory Consults (99271 – 99275) HCPCS exams (G0101, G0175, G0245, G0246, G0264) Ophthalmology codes for appropriate exams (92002 – 92014) – Patients in observation status • Hospital Observation Services (99217 – 99220 and 99234 – 99236) – Emergency Room • Emergency Department Services (99281 – 299285) APCs for E/M • Codes for E/M visits route to 6 APC groups – APC 0600 Low-level clinic visits • 92012, 99201, 99202, 99211, 99212, 99241, 99242, 99271, 99272, 99431, G0101, G0245, G0246, G0264 – APC 0601 Mid-level clinic visits • 92002, 99203, 99213, 99243, 99273 – APC 0602 High-level clinic visits • 92004, 92014, 99204, 99205, 99214, 99215, 99244, 99245, 99274, 99275, G0175 – APC 0610 Low-level emergency visits • 99281, 99282 – APC 0611 Mid-level emergency visits • 99283 – APC 0612 High-level emergency visits • 99284, 99285 CMS on Level of E/M Service • Hospitals identify and follow a method for choosing the level of service – "As long as the services furnished are documented and medically necessary and the facility is following its own system, which reasonably relates the intensity of hospital resources to the different levels of HCPCS codes, CMS will assume that it is in compliance with these reporting requirements." • There should not be a high degree of correlation between the code reported by the physician and that reported by facility. Choosing the Level of Service • Systems for choosing the level of E/M are developed by each facility – Facilities must follow their own systems – Facility codes would not often match providers • “New" and "established" pertain to whether the patient already has a medical record • Use 99281 for screening services in the ER when no treatment is furnished CMS on Documentation • Facilities that use documentation to determine the level of E/M have little problem supporting the codes. – If physicians, nurses, or clerical staff assign codes without reference to documentation, routine periodic audits should be performed to ensure that documentation supports the level of service • This includes facilities that crosswalk to link their acuity levels to E/M codes. – Documentation is the final arbiter of the level of service – Inappropriate assignment of E/M codes is viewed as a compliance issue Observation Care • Originally packaged item – Bundled into ER and Surgery APCs • Separate payment now allowed for 3 diagnostic categories: – Chest pain – Asthma – Congestive heart failure • May use admitting diagnosis • Patient must be in observation for at least 8 hours and no more than 48 hours Critical Care • Critical care is classified as a "significant procedure" (APC 0620) under the OPPS. – Hospitals use code 99291 to report outpatient critical care services • Used in place of a code for a medical visit or emergency department service. • Use CPT definition of "critical care" and coding guidelines – Exceptions • Facilities only paid for one period time with code 99291 • Services usually bundled into Critical Care codes may be billed separately when furnished on the same day Other Coding Difference • Surgery package includes all anesthesia but does not include pre- and postoperative global visits – Bill with separate E/M when provided in facilitybased clinic • Do not use global maternity codes – Use “Delivery Only” codes and code for prenatal and postnatal care with E/M codes if provided in facility-based clinic • Do not use “global” codes (i.e., with interpretation and report) for services like EKGs – Use the “tracing only” codes Inpatient Only List • Status Indicator “C” • Services that must be performed inpatient due to – Invasive nature of procedure – Need for at least 24-hours of recovery or monitoring time before the patient can be safely discharged – Performance in the inpatient setting because of underlying condition of patient • Codes removed from list due to reevaluation and technology changes • 2003 allowed payment for Inpatient Only services in outpatient for emergencies ASC List • ASC is Ambulatory Surgery Center – Free-standing outpatient surgery center not associated with a hospital • ASC list includes procedures that require ORs but not admission for procedure or recovery – Procedures not on ASC list are “out-ofscope” • Procedures that might be performed in outpatient but might require emergent admission Factors in APC Payment Calculation • • • • Relative weight Conversion factor Wage adjustment factor Copayment Annual updates affect – APC groups, payment adjustments, conversion factor, and payment weights Other Outpatient Facility Payment Systems • Fee schedule • Outlier and pass-through payment • Composite rate methodology UB-92 and APCs • Importance of coding in APC system • UB-92 – Codes – Dates of Service – Service units – Bill Type – Revenue Codes Annual Updates and Changes • Required by law and may change – – – – APC groupings Payment adjustments Conversion factor Payment weights • Changes to APCs may result from – – – – Changes in technology Changes in CPT codes Codes removed from Inpatient Only List New procedures or services • CMS publishes Proposed Rule for comments – Final Rule is issued after comment period and any adjustments 2001 Changes • Revisions to APCs due to new or deleted HCPCS codes • Procedures removed from Inpatient Only list • APCs reconfigured for some devices removed from pass-through list • New APCs for Radiology using contrast 2002 Changes • Outlier threshold and payment percentage changed • Outlier payment computed per service rather than per claim • Observation care payment allowed for three diagnoses • Packaging changes • New guidelines for pass-through payments • Exceptions to the 2-times rule 2003 Changes • Exceptions to the Inpatient Only list were made for these services performed in emergencies • Observation care payment based on admitting diagnosis • Pass-through payments were updated • Codes developed for trial billing 2004 Changes • Outlier payments revised again • Payments for new technology readdressed • Nuclear medicine payment system revised • Standard system for choosing level of E/M services were not implemented but CMS acknowledged need E/M Standard • CMS received industry criticism for lack of a standard E/M level methodology for all providers. – CMS recognized that a national standard is needed. • 2002 OPPS proposed rule, CMS deferred comment on establishing a standard. – Several organizations submitted their version of E/M criteria. • Most hospitals have developed what is called a "point system" for selecting E/M levels – A decision on a standard methodology still has not been made Legislative Changes • Several changes have affected APCs since implementation • Benefits Improvement and Protection Act (BIPA) – Took effect in December 2000 – Changes to APCs • Accelerate reductions in beneficiary copayment amounts • Set up categories of devices for pass-through payment Outpatient Code Editor • Analyzes hospital outpatient claims for coding edits using CCI • Validates ICD-9 and HCPCS codes • Assigns APCs • Identifies errors • Indicates actions needed National Correct Coding Initiative • The NCCI is a set of billing edits developed by HCFA to identify coding patterns resulting in overpayment to the providers • More than 107,000 Correct Coding Initiative edits are incorporated into the outpatient code editor for OPPS – Edits determine what procedures and services cannot be billed at the same time when they are furnished for the same patient on the same day Assignment of Codes and APCs • Appropriate procedure and diagnosis codes are extracted from the medical record – Encoding software helps with bundling issues and assignment of APCs • Codes may also be assigned in specific departments – Related charges are added by the Chargemaster Charge Description Master (CMD) • A computerized master price list of everything the facility can prove to patients – Includes supplies, diagnostic tests, pharmaceuticals, procedures, and other room time – Hundreds of thousands of items are included in chargemaster to link services provided in a hospital and the generation of claim forms • Chargemaster is maintained by the Chargemaster Coordinator including – Annual updates (e.g., code changes) – Updates specific to the CDM – Monthly audits to determine whether bills follow billing regulations CDM Continued • Some claims are generated almost entirely from the Chargemaster – Chemotherapy – Interventional radiology – Radiation therapy • Some services that previously were chargemaster driven require coding to be performed by the HIM department under APCs Significant Abbreviations • • APC – Ambulatory Payment Classification • • APG – Ambulatory Patient Group • • ASC – Ambulatory Surgery Center • • BBA – Balanced Budget Act • BBRA • – Balanced Budget Refinement Act • CDM • – Charge Description Master CMS – Center for Medicare and Medicaid Services DME – Durable Medical Equipment DRG – Diagnosis Related Group HCPCS – Healthcare Common Procedure Coding System OBRA – Omnibus Budget Reconciliation Act OPPS – Outpatient Prospective Payment System