NURS 246 Health Alterations lll
advertisement
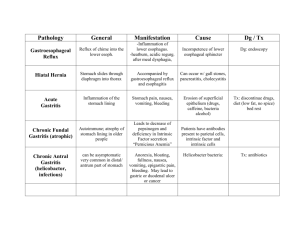
N 246 Health Alterations lll Fall, 2010 Alterations in the GI System Sandra Buckley, RN,MS A & P of GI system 30 ft. long from mouth to anus. Consists of mouth, esophagus, stomach, small intestine, large intestine, rectum, anus. Associated organs: liver, pancreas, gallbladder. Organs covered by peritoneum (parietal:lines abdominal cavity, visceral:covers organs), two folds of peritoneum are mesentery (contains blood vessels and lymph glands) and omentum (contains fat and lymph nodes) Physiology Innervated by parasympathetic, sympathetic and intrinsic nervous system. Parasympathetic:excitatory (increased peristalsis). Sympathetic: inhibitory (decreased peristalsis). Intrinsic (enteric): coordination of motor and secretory functions-two nerve layers that lie between mucosa, contribute to motor and secretory activities. Circulation of GI system Receives approximately 25-30% of cardiac output. Major source from which blood can be diverted during exercise or stress. Venous blood draining the GI tract organs empties into portal vein, which then perfuses liver. Upper GI- blood from splanchnic artery, small intestine-blood from branches of hepatic and superior mesenteric arteries.Large intestine-superior and inferior mesenteric arteries. Arteries of stomach, liver, spleen Function/physiology of GI Each part of system performs different activities. Ingestion and propulsion of food: mouth, pharynx, esophagus. Digestion and absorption: mouth, stomach, small intestine. Elimination: large intestine Ingestion Intake of food, impacted by: appetite-desire to eat, center located in hypothalmus, factors affecting; (increasing appetite) hypoglycemia, empty stomach, decrease in body temperature, sight, smell, taste of food. (decreasing appetite) stomach distention, illness (fever),hyperglycemia, nausea, vomiting, drugs, input from higher brain centers. Hormone Ghrelin; released from stomach mucosa to stimulate appetite. Hormone Leptin; released and involved in appetite suppression Factors affecting GI tract Emotions: stress, anxiety, happiness. May be manifested by anorexia, epigastric and abdominal pain, diarrhea, constipation, gas, decreased satiety and increased consumption (above caloric need). Physical factors: diet, alcohol, caffeine, cigarette smoking, drugs, fatigue, organic diseases, metabolic factors. Swallowing (deglutition) Involve mouth pharynx and esophagus Mouth-lips and oral (buccal) cavity, roof of cavity is soft palate, contains teeth used in chewing (mastication) and tongue. Taste receptors; sides and tip of tongue (important for speech and pushing food to back of throat). 3 sets of salivary glands: parotid, submixillary, sublingual-produces saliva (contains salivary enzyme amylase) Swallowing video http://www.youtube.com/watch?v=Z7x KYNz9AS0 http://www.youtube.com/watch?v=uxH UUgLeNzk Pharynx Musculomembranous tube; nasopharynx, orophrynx ( when food or water present, stimulates swallowing reflex), laryngeal pharynx Secretes mucus, aids in swallowing Epiglottis: lid of fibrocartilage that closes over the larynx during swallowing. pharynx Esophagus Hollow, muscular tube ~ 10 inches long. When swallowing: upper esophageal sphincter (cricopharyngeal muscle) relaxes and a peristaltic wave moves the bolus into the esophagus. Muscular layers contract (peristalsis) and propel food to stomach. Lower esophageal sphincter (LES)- at distal end of esophagus, remains contracted except during swallowing, belching or vomiting. Important barrier that prevents reflux. Dyspepsia Refers to host of upper abdominal or epigastric symptoms such as pain, discomfort, fullness, heartburn, regurgitation or “indigestion”. Etiology: drug intolerance, GI tract dysfunction, pancreatic or biliary tract disease. Dyspepsia Functional or nonulcer dyspepcia-most common cause of chronic dyspepsia. 2/3’s of patients have no obvious organic or biochemical cause for symptoms that can be evidenced by endoscopy. Clinical findings: weight loss, vomiting, dysphagia, melena, anemia. GERD Gastroesophageal reflux disease (GERD),not a disease but a syndrome that results in reflux of gastric secretions into esophagus. Predisposing conditions: LES (incompetent lower esophgeal sphincter), hiatal hernia, decreased gastric emptying. Results in: - irritation – pyrosis (heartburn), -inflammation - esophagitis, hoarseness, -difficulty swallowing – dysphagia. Gerd-diagnosis Upper GI x-ray with barium swallow Esophageal endoscopy Esophageal manometry Ph monitoring Barium swallow Outlines the esophagus Contrast is ingested Gastrografin (water soluble contrast), and barium Nursing care: educate and support pt.; signed consent, allergy status to meds or contrast, need to drink contrast, assume various positions on table, NPO 8-12 hours before procedure, avoid smoking 12 after midnight. After procedure; take measures to prevent contrast media impaction (fluids, laxatives), stool may be white 72 hours post-test. PT. education Lifestyle changes Dietary changes- alcohol, spices, chocolate, broccoli, salmon, caffeine, smoking, mint, fat. Medications-antacids(tums, maalox), H2 blockers (tegamet, pepsid), protein pump inhibitors (nexium, Protonix), prokinetic meds (metaclpromide) Other esophageal disorders Barrett’s esophagus-precancerous lesion, requires annual tissue biopsy. Esophagitis-due to chemical irritation (dust, lye, temperature, ETOH abuse). Achalasia-cardiospasm of lower portion of esophagus muscle. Causes obstruction and accumulation of food and fluid. Esohageal disorders Esophageal cancer-rate is high in Asia, low in U.S., but higher incidence in African-Americans and men. Prognosis poor. Clinical manifestations-similar to GERD. Esophageal strictures-caused by chronic GERD or ingestion of caustic liquids. Intervention-endoscopic dilation. Esophageal varices Dilated tortuous veins in lower portion of esophagus. Complication of liver cirrhosis. Bleeding varices most life-threatening complication of cirrhosis. Factors producing irritation: Alcohol, poorly masticated food,acid regurgitation, increased abdominal pressure (nausea, vomiting, straining, coughing). stomach Function is to store food, mix food with gastric secretions, and empty contents into small intestine. Absorbs only small amount of water, alcohol, electrolytes and certain drugs. Average length of time food in stomach:3-4 hours Chief cells secret pepsinogen (antecedent of pepsinthe main enzyme of gastric juice which converts proteins into peptones) Parietal cells secrete hydrochloric acid, water and intrinsic factor (increases absorption of vitamin B complex) stomach Gastritis Results from breakdown in normal gastric mucosal barrier. May be acute or chronic. Type A-associated with autoimmune disorder, Type B-associated with H. Pylori. Clinical manifestations similar to GERD, often self-limiting. Gastritis (continued) Severe cases may require NPO, IV fluids, NG for lavage. When atrophy of cells occur, may result in loss of intrinsic factor/decreased RBC’s/anemia. Tx- education,lifestyle modification, assessment of severity,medication, surgical interventions (gastrectomy,vagotomy or pyloroplasty). Medications- antacids,Zantac, Tagamet, prilosec, prevacid Pernicious anemia Intrinsic factor produced by cells in gastric mucosa Binds with ingested B12 (degraded by HCL) to form complex that travels to small intestine for absorption. B12 deficiency: anemia Atrophic gastritis: common condition in older people, damages cells of stomach, without healthy cells, production of HCL and intrinsic factor is diminished. Vitamin B12 deficiency caused by atrophic gastritis and a lack of intrinsic factor is know as pernicious anemia. Hiatal Hernia Herniation (bulging upwards) of a portion of stomach through diaphragmatic opening. Acid from stomach spills into unprotected esophagus – irritation of mucus lining. “choking feeling”, lump in throat, food stoppage and regurgitation More common in older adults and women. Hiatal Hernia Diagnositic studies: barium swallow, endoscopy. Collaborative care: administration of medications (antacids, antisecretory agents), avoidance of lifting and straining, elimination of alcohol and smoking, HOB elevation Surgical Therapy (hiatal hernia) Objective to reduce reflux by enhancing integrity of LES. Procedures: valvuloplasties: also called fundoplication, involves wrapping of fundus of stomach around lower portion of esophagus. Can be preformed laproscopically. Prevents reflux in 90% of patients. Nursing management Postop care: prevention of respiratory complications, IV therapy, wound care, education. If NG present- maintain patency of tube, dangerous to attempt to replace tube if dislodged due to possibility of perforation of surgical repair. Upper GI Ulcers Peptic ulcers- erosion of GI mucosa mostly in Antrum an duodenum Caused by the digestive action of HCL acid & pepsin. Acute (superficial) Chronic (deep, longer healing) Gastric or duodenal ( by location), but different in etiology and incidence. Physiology of Peptic ulcer disease Mucosal defense system may be impaired by: H. pylori, inadequate blood flow, smoking ,NSAIDs Compare gastric vs duodenal Gastric - superficial, in antrum/body of stomach Common in women and unskilled workers, low socio-eco. Burning, gas pressure left epigastric, to back, high abdominal. Pain 1-2 hrs after food intake. Increased w/ smoking, drugs and alcohol use N/V, weight. loss Duodenal-high end of duodenum. Common in men, associated with psychic stress, 80% of all ulcers Burning, gnawing, midepigastric, to back, high abdominal,pain 2-4 hrs after meals, episodic, middle of night. Pain relief with antacids and food intake, N/V. Increased with alcohol, Stress ulcers Erosive gastritis caused by: Transient GI ischemia (low blood supply) with shock, severe injury, burns, surgery. Low blood supply results in imbalance of acid and mucus barrier- causing erosion. Prevention: prophylactic meds: antacid, Famotidine (Pepcid) Complications of chronic ulcer disease. Hemorrhage, more common with duodenal ulcers Perforation, most lethal complication, associated with peritonitis. Gastric outlet obstruction-scaring and atony of pylorus. Systemic Acid Blockers Histamine 2 Take any time of day (x2), no food restrictions Zantac, Tagamet (oldest, not for elderly/drug interactions), pepcid (IV, PO) Proton Pump inhibitors Take in AM before meal (30 min.) Usually 1xday Prilosec, Prevacid, Protonex, Aciphex Prilosec not indicated for those on coumadin Surgical interventions ulcer disease 20% of ulcer pt’s require surgery, but rarely performed now, usually resolved with medications. Procedures: gastrectomy (billroth I or II) vagotomy (cut vagus nerve to decrease gastic acid secretion) Pyloroplasty(pyloric dilatation) Nursing interventions of Post-op care If NG present, maintain patency, nares care, I&O, comfort, educational and emotional support. Surgical wound monitoring Observe signs of bowel status: bowel sounds present? r/o obstruction or bleeding) Pain control (monitor, position change) Post op teaching: diet, lifestyle risks and changes Dumping Syndrome Results from reduced gastric capacity after resection of most of the stomach and pyloric sphincter. Symptoms occur 15-30 min. after a meal, feelings of weakness, sweating, palpitations, dizziness Due to large bolus of hypertonic fluid entering intestine and fluid drawn into bowel, causes distention of bowel. Advise patient to lie down. Postprandial hypoglycemia Varian of dumping syndrome Bolus of concentrated carbohydrate results in hyperglycemia and excessive amounts of insulin, occurs 2 hrs after meals. Treatment-sugared fluids or candy to relieve hypoglycemia. Then, limit amount of sugar consumed with meal and eat small, frequent meals. Nutritional therapy related to surgical intervention Eliminate drinking fluids with meals Dry foods with low carbohydrate content (avoid high sugar diet) Small meals Rest after meals Heliocobacter pylori bacterium Promotes peptic ulcer formation Acquired in childhood and common in adults Gram-negative bacillus cultured in 1982 Prevalence of H. Pylori infection in duodenal ulcer patients as high as 95-100%. Treatment: triple Therapy (amoxicillin, Biaxin,Prilosec) H. Pylori and autoimmune response http://www.wnyc.org/shows/radiolab/e pisodes/2009/09/25/segments/133980 c. Diff http://www.nytimes.com/2010/07/13/s cience/13micro.html?_r=2&ref=science Upper GI hemorrhage management Upper GI hemorrhage is defined as loss of more than 1500ml. Of blood, or 25% of blood volume. ~200,000 hospital admissions year for UGI bleed Mortality rate 6-10% Increased incidence of UGI bleed in older adults, women r/t use of NSAIDs Drug induced: aspirin, NSAIDs, corticosteroids (get history!) GI Hemorrhage-upper GI Self-limiting in 85% of patients. Originates from a number or sources: -Peptic ulcer disease-accounts for ½ of major upper GI bleeds. -Portal hypertension-results in bleeding Varices (most often esophageal), accounts for 10-20% of hemorrhages. Upper GI hemorrhage Mallory-weiss tear-laceration of gastroesophgeal junction, 5-10% of GI hemorrhages, ~1/2 of patients report history of heavy alcohol use or retching. Vascular anomalies Gastric neoplasm's Erosive gastritis, usually superficial and attributable to NSAID, aspirin, corticosteroids, alcohol or stress. Erosive esophagitis-due to chronic GERD GI Hemorrhage Obvious – hematemesis frank blood, bright red or coffee- ground, ( dark mahogany, grainy digested blood), Melena- black, tarry stools Hematochezia-stools containing bright red blood. Occult – not visible to the naked eye. Presence of very small amount of blood in mucus, gastric secretions or stool, detected by guaiac test. Esophageal varices bleeding/hemorrhage control Stabilize pt. and mange airway. IV started (may include blood products). Diagnosis determination Endoscopic exam, lavage Esophageal varices management Main goal is avoidance of bleeding and hemorrhage. Management of bleeding-medications (vasopressin, nitroglycerin, b adrenergic blockers), balloon tamponade, sclerotherapy, ligation of varices, shunt therapy Causes: GI BLEED In stomach & duodenum: erosion of bld. Vessels in the lining due to: peptic ulcer, stress ulcer, hemorrhagic gastritis, cancer, GI polyps, medications Systemic disease: interfere with blood clotting. blood dyscrasias leukemia Nursing interventions Stabilization, (don’t forget emesis basin!, universal precautions) evaluation, vs q 15 min.,evaluate for signs of shock, lab values, ABGs, U/A, guiac stool, IV fluid replacement Assessment of hemodynamic status, hematocrit, NG tube placement, pharmacologic intervention, use of O2 blood replacement, endoscopy. Cancer of stomach 7th leading cause of cancer mortality in US. Worldwide, 2nd most common form of cancer, Japan and Costa Rica have highest rates More common in men Signs and symptoms Manifestations may exhibited by: pain, anemia, ulcer disease, indigestion. Detection difficult due to vagueness of symptoms. Diagnostic tests: analysis of blood, stool and gastric secretions(histology), CEA test (carcinoembryonic antigen), upper GI series, endoscopy. Surgery-gastrectomy as radiation and chemotherapy not proven to be successful as primary intervention. Nausea and Vomiting Feeling of discomfort with desire to vomit (forceful ejection of food and secretions-emesis) Related to slowing of gastric motility and emptying, or if GI tract becomes irritated, excited or distended. Nausea is subjective usually accompanied by anorexia (lack of appetite) May result in dehydration, electrolyte imbalances, decreased plasma volume, metabolic alkalosis, weight loss, threat of aspiration (elderly, unconscious or conditions that impair gag reflex) N&V Most common manifestation of GI diseases Protective mechanism Fecal odor or bile (d. green) indicate lower GI obstruction Collaborative care Emotional support Nutritional therapy-IV fluids, electrolyte replacement, glucose, advance to clear liquids-full liquids. NG tube to suction (decompression) Dietary consult Nursing diagnosis: imbalanced nutrition: less than body requirements. Gerontologic considerations Increased risk of cardiac or renal insufficiency, fluid/electrolyte imbalances, increased susceptibility to CNS side effects of antiemetic meds. Caution with fluid replacement (monitor fluid status: edema, BP, resp. status) Alteration in LOC (increased risk for aspiration) Medications/antiemetics Easier to prevent than treat! Give prophylactically. Most cause sedation Prokinetic-Reglan (aka metoclopromide, dopamine and serotonin receptor blocker, increases upper GI motility) Serotonin Receptor agonists-Zofran, Kytril, Anzemet,( used for Chemo and induction of anesthesia) Dopamine antagonists-Phenothiazines-Phenergan, compazine, thorazine. Butyrophenones-Haldol Diarrhea Not a disease but a symptom May be acute (infection, can be selflimiting) or chronic (2-4wks) May result in explosive watery diarrhea, tenesmus, cramping, abdominal pain. Perianal skin irritation Symptoms continue until the irritant or causative agent is excreted. Potential Consequences of diarrhea Debilitating, life threatening Dehydration Electrolyte imbalances Malabsorption and malnutrition Major cause of death throughout world (especially in children) In 2009 diarrhea was estimated to have caused 1.1 million deaths in people aged 5 and over and 1.5 million deaths in children under the age of 5 (wikipedia) diagnosis History: travel, food ingestion (diet, food allergies, lactose intolerance) medications, surgery, family exposure, etc. (see previous chart) Lab: WBC, anemia, iron and folate deficiencies, elevated liver enzymes, electrolyte disturbances. Stool: blood, mucus, WBC’s, paracites (O&P), culture, fat content Collaborative care Based on cause and aimed at replacement of fluid and electrolytes, decrease in number, volume and frequency of stool. Physical assessment: vs, weight, skin breakdown, abdominal inspection Oral replacement-water, solutions containing glucose and electrolytes (mild) Parenteral- fluids, electrolytes, vitamins, nutrition (severe) Antibiotics, antidiarrheals Nursing implementation Infection control Pt support-emotional, fatigue, embarrassment, pain Hydration status, I&O, fluid replacement Normal nutritional intake medications Antibiotics-specific to organism, but may cause inreased diarrhea by altering normal GI flora (lactobacillus) May be susceptible to Clostridium difficile infection ( treated with Vancomycin, Flagyl) Healthcare workers use vigilance regarding transmission (isolation, hand friction, gloves) Diarrhea etiology (general classifications) Diarrhea-infectious Lower GI hemorrhage Hematochezia usually present Bleeding from small intestine or colon Etiology: diverticulosis, most common cause of lower GI bleed, ~40%. Present in patients who are >50 with hematochezia Vascular ectasis-common in patients over 70yrs old. Lower GI hemorrhage Neoplasms Inflammatory bowel disease-ulcerative colitis, often have diarrhea with varying amounts of hematochezia. Symptoms: abdominal pain, urgency and tenesmus. -Tenesmus-spasmodic contraction of anal sphincter with pain or persistent desire to empty bowel or bladder. -Anorectal disease-hemorrhoids, fissures. Inflammatory Bowel disease Crohn’s disease Most often seen in ileum, jejunum and colon. Abscesses or fistulas may develop Nonbloody diarrhea and abdominal pain. Not cured by surgery Tx to rest bowel Ulcerative colitis Multiple abscess develop Bloody diarrhea and abdominal pain Tenesmus Cure with colectomy Tx to rest bowel Diverticulosis and diverticulitis Multiple outpouching of mucosa in colon. Diverticulosis-multiple, noninflammed diverticula, pt. often w/o symptoms Diverticulitis-inflammation of diverticula in sigmoid colon, due to retention of stool and bacteria in diverticulum Associated with lack of dietary fiber. Pt. should not have BE or colonoscopy due to possibility of perforation or peritonitis. Ulcerative colitis Inflammation and ulceration of colon and rectum, multiple abscesses may develop Higher incidence in women, age 15-25, chronic disorder Symptoms: bloody diarrhea and abdominal pain. Treatment-rest bowel, medications, diet, surgery Crohn’s disease Inflammation of segments of GI tract, most often ileum, jejunum and colon, chronic disorder Abscesses and fistulas may develop Symptoms: diarrhea, fatigue, abdominal pain, weight loss, fever. Treatment-drug therapy, nutritional therapy, surgery does not cure disease. Cancer of colon and rectum 2nd most common cause of cancer death in US. Diet is most important environmental factor associated with colorectal cancer. Symptoms: rectal bleeding, changes in bowel habits, abdominal discomfort, occult bleeding. Steady blood loss as it grows and ulcerates Diagnostic studies Digital rectal exam Sigmoidoscopy, barium enema, CT scan, lab tests (anemia). Treatment-surgery, extent determined by location and extent of cancer, radiation , chemotherapy. GI Inflammation & Infection Acute abdomen – sudden onset abd. pain requiring prompt decision making. Varied causes: trauma, ischemic bowel, ulcers, PID, pancreatitis, GB, ruptured gut, uterus, ovarian cysts, peritonitis, perforations, bowel obstruction. Acute Abdomen dx and tx Exploratory laparotomy – “open, look & see”. Diagnostic as well as a surgical procedure. Use to surgically remove (GB, appendix) or surgically repair (ruptured abdominal aortic aneurysm) Trauma - abdominal Blunt trauma – motor vehicle accident Penetration injuries – gunshot, stab wounds Both results in internal organ damage.. Trauma: signs and symptoms See: contusions, abrasions, hematoma, bruising, Cullen’s sign, Turner’s sign. hematuria, hematemesis Feel: hard, distended abdomen guarding, splinting. Hear: absent or decreased bowel sounds. Peritonitis Local or generalized inflammation. Primary causes: infections from blood, cirrhosis w/ ascitis, genital tract organisms. Secondary: ruptured appendix, blunt or penetrating abdominal trauma, pancreatitis, ruptured diverticulitis, peritoneal dialysis. S/S: abd. pain, rebound tenderness, spasm Pancreatitis Mild edema to severe necrosis of the pancreas. More common in middle-aged men. Common causes: alcoholism, GB disease Less common causes: trauma, viral, duodenal ulcer, pancreatic cysts, CF, drugs (sulfas, thiazides steroids, NSAIDs) Pancreatitis Auto digestion of pancreas due to reflux of bile acids into pancreatic duct. as in post GI surgery, post ERCP - ERCP - Endoscopic retrograde cholangio-pancreatography Pancreatitis: manifestations Abdominal pain – LUQ to mid epigastric, radiate to back. Deep, piercing, steady pain. GI: pain aggravated by food, nausea not relieved by vomiting, distended abd (ileus) absent bowel sounds. CV/resp . <BP, >HR, >RR, fever, crackles Skin: jaundiced, flushed, Pancreatitis: Dx & treatment DX: elevated serum amylase, lipase ERCP reveals gallstones xrays of abd. Ultrasound TX: NPO then high CHO, lo fat, hi protein Relieve pain and spasm Meperidine, nitro, papaverine Cholecystitis/Cholelithiasis Cholecystitis commonly due to bile stones Also caused by bacteria (e. coli, streptococci, salmonella) from vascular or lymphatic route or chemical in bile. Cholelithiasis bile supersaturated with cholesterol causing precipitation – stones. Stones may migrate to cystic or CBD ducts resulting in obstruction. S/S indigestion, pain, fever, jaundice, N/V Fluid Elect. Imbalances from GI fluid loss (daily amts) Salivary glands Stomach Small intestines Pancrease Liver, GB 1000 to 1500 ml Enzyme- Amylase (ptyalin) 2500 ml Pep’gen,hcl Gastric juice Lipase,I fac 3000 ml Amyl,lipase peptidases 700 ml panc Tryp’gen, reatic juice Amyl, lipase 1000 ml Bile bile Initiates CHO digest Protein, fat Cobalamin CHO, fat protein Protein, fat CHO Fat emulsion Fluid losses from GI Vomiting Gastric/intestinal suctioning Diarrhea Ileostomy Prolonged use of laxatives enemas Parenteral fluid/elect replacement Provide adequate fluid replacement. Dietary consult. Calorie count. Monitor labs: elect., glucose, albumin levels. Monitor tube placement– gastric residual output (grass green color), acid level, amount Monitor temps, WBC, infection control ”wick” via NG tube, frequent oral care, nasal care. I & O- IV fluids, PEG/tube feeds, BM, ostomy drainage. IV fluids, electrolytes, parenteral feedings: Crystalloids- dextrose, Ringer’s lactate Colloids – albumin Bld products- packed RBC, leucocyte poor blood, Fresh Frozen Plasma Electrolytes- Kcl, Nacl PPN - peripheral parenteral nutrition TPN – total parenteral nutrition Influencing factors GI Environment: lifestyle, travel Growth and development: childhood illness , eating habits anorexia nervosa, bulimia Diversity: home remedies, intolerances, obesity, eating disorders, dietary preferences Sexuality: practices, slimming diets, exercise Coping - stress response result in ulcer formation or aggravation c. Influencing factors Aging: Loss of appetite due: problems with gums, teeth, loss sense of taste, smell, less saliva Delayed esoph. emptying, incompetent LES, < gastric motility,< emptying ,< HCL, I factor < ability of liver to metabolize med/hormones Constipation: name 7 causes Pediatric Differences GI system immature at birth Gastric capacity – newborn – 10-20ml 1 wk.- 30-90, 1 mo.- 90-150, 1yr.- 210-360 Peristalsis greater in newborn – loose BM Digestion occurs in duodenum Enzymes are deficient until 4-6 months Liver function immature. Structural Defects: Cleft lip, cleft palate- difficulty feeding. Esophageal atresia (blind pouch) w/ tracheo-esophageal fistula. Pyloric stenosis- obstructive hypertrophy of the circular muscle around pyloric canal, S/S: projectile vomiting, irritable, hungry. Surgical correction –treatment of choice. Disorders - GI Motility in Child Gastroenteritis –inflammation of the stomach & intestines accompanied by vomiting, cramps and diarrhea Kids in day care, poor housing sanitation Average 5 yr old - 2 episodes/year Cause- viral, bacterial, parasitic. Risk for hypovolemic shock if untreated due to severe dehydration. Health History Health Mgt: Smoking, alcohol,exposure,travel Usual daily food and fluid intake, weight gain/loss, food allergies, intolerances. Measures (cultural) used to treat symptoms, pain, diarrhea, nausea, vomiting, caregiver Elimination pattern: frequency, time of day, consistency Activity/sleep pattern: How exercise affect GI, been awakened by gas, heartburn. Relationships, stress/coping, value/belief patterns. Assessment: syllabus outline Nursing history: main complaint, pain,location duration, aggravation by food or not. Medical hx, family hx, meds, OTC drugs. Physical exam: oral, dental, gum, breath odor Abdomen: skin pigment, scars, striae, masses pulsations, bruits, bowel sounds, peristalsis, distention. Note location, quadrants, region. Inspect, auscultate, percuss first, then palpate. “Listen before you touch.” Common alterations/disorders: chronic or recurring. Diagnostic Tests: prep and care Fiberoptics: EGD, ERCP- examines upper GI. proctosigmoidoscopy colonoscopy- lower GI. Xrays: barium swallow- esophageal study Ultrasounds, CT scans, angiography Lab tests: serum amylase, lipase Stool- clay-colored, guaiac, ova/parasite Gastric analyses- acidity and content Paracentesis- removal ascitic fluid- dx and tx Tube feeding Types: gastrointestinal- short vs longterm gastrostomy-differt insertion than PEG Jejunostomy- do not check residuals. Formulas: depending on alteration. Precautions: aspiration, HOB 30 degrees, stop feeding w/ patient turns, ? residuals Infection: oral care, intubated, how often. Prevent accidental displacement or removal. Surgical Care Vagotomy (reduce acid in peptic ulcer) Billroth I, II (dumping syndrome) Bowel resection (seminar) Fecal diversions colostomy ileostomy Nursing Diagnoses - GI Impaired tissue integrity: chemical irritant Altered elimination: diarrhea, constipation Risk fluid volume deficit r/t vomiting, diarrhea, gastric decompression, hemorrhage Risk for infection/altered protection Risk impaired peristomal skin integrity Nursing Diagnoses: GI Altered comfort: pain r/t tissue damage inflammatory process distention, nausea Knowledge deficit r/t disease and treatment P.C. metabolic alkalosis/acidosis P.C. low potassium, low/high sodium, low magnesium Interventions Position: semi-fowlers, knee support Activity: bedrest, BR privilege, commode Pain mgt: assess and treat regularly. Diet mgt: npo, ice chips, mouth care, liquids Meds: a.c. p.c. crushed, via feeding tubes GI tubes purpose:decompression/feeding salem-sump - for decompression- low suction levine, Keofeed or Dobhoff, intestinal tubes (Miller, Abbot) Outcome Criteria Normovolemic status – vital signs stable NO infection and injury, adequate blood sugar, electrolytes, calories required. Pain decreased. Self-care, ADL, dressings. Verbalize knowledge about cause and rationale for treatment. Discharge planning/teaching Lifestyle modification: diet, activity, weight and stress management, relaxation techniques, OTC drugs. Signs of exacerbation, infection Wound, colostomy care, follow-up Sexuality concerns Support groups and com. resources Legal and ethical issues Withholding Treatment 26 yr old patient in a permanent vegetative state, enteral tube fed, w/ 15th bladder infection. Should antibiotics be w/held? Feeding? Family expressed concern that no heroic measures be used to extend biologic life of their daughter. They have been unwilling to withdraw existing enteral nutrition. Ethical and Legal Principles Treatment maybe withheld if a competent patient, refuses consent, if it is medically futile or if the burden of it’s provision outweighs the benefit. If withholding treatment leads to death, the underlying disease is the cause. Intervention simply prolongs life. Pt in a permanent vegetative state cannot be cured of that brain damage. Any treatable comorbidities related to condition will not lead to recovery from permanent vegetative state. Bibliography Medical-Surgical Nursing, 7th edition, Lewis, Heitkemper, Dirksen, O’brian, Bucher. Atlas of Human Anatomy, 4th edition, Netter Pharmacology, 3rd edition, Kee and Hayes Understanding Nutrition, 11th edition, Whitney.