50000 series - Coding Certification Tips
advertisement
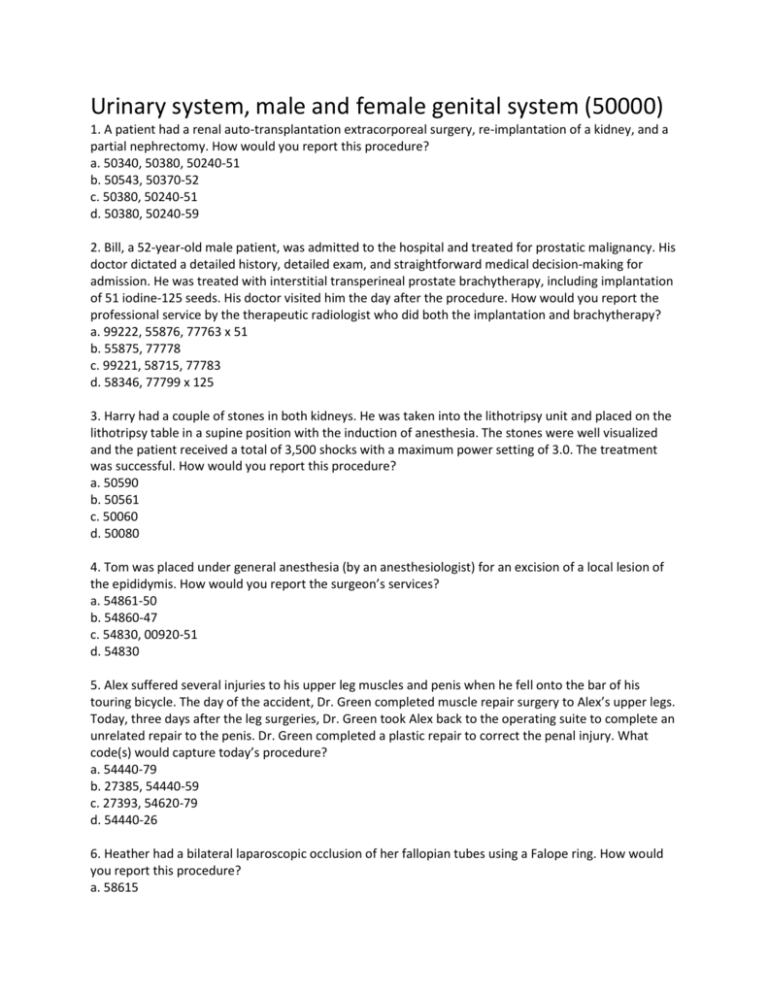
Urinary system, male and female genital system (50000) 1. A patient had a renal auto-transplantation extracorporeal surgery, re-implantation of a kidney, and a partial nephrectomy. How would you report this procedure? a. 50340, 50380, 50240-51 b. 50543, 50370-52 c. 50380, 50240-51 d. 50380, 50240-59 2. Bill, a 52-year-old male patient, was admitted to the hospital and treated for prostatic malignancy. His doctor dictated a detailed history, detailed exam, and straightforward medical decision-making for admission. He was treated with interstitial transperineal prostate brachytherapy, including implantation of 51 iodine-125 seeds. His doctor visited him the day after the procedure. How would you report the professional service by the therapeutic radiologist who did both the implantation and brachytherapy? a. 99222, 55876, 77763 x 51 b. 55875, 77778 c. 99221, 58715, 77783 d. 58346, 77799 x 125 3. Harry had a couple of stones in both kidneys. He was taken into the lithotripsy unit and placed on the lithotripsy table in a supine position with the induction of anesthesia. The stones were well visualized and the patient received a total of 3,500 shocks with a maximum power setting of 3.0. The treatment was successful. How would you report this procedure? a. 50590 b. 50561 c. 50060 d. 50080 4. Tom was placed under general anesthesia (by an anesthesiologist) for an excision of a local lesion of the epididymis. How would you report the surgeon’s services? a. 54861-50 b. 54860-47 c. 54830, 00920-51 d. 54830 5. Alex suffered several injuries to his upper leg muscles and penis when he fell onto the bar of his touring bicycle. The day of the accident, Dr. Green completed muscle repair surgery to Alex’s upper legs. Today, three days after the leg surgeries, Dr. Green took Alex back to the operating suite to complete an unrelated repair to the penis. Dr. Green completed a plastic repair to correct the penal injury. What code(s) would capture today’s procedure? a. 54440-79 b. 27385, 54440-59 c. 27393, 54620-79 d. 54440-26 6. Heather had a bilateral laparoscopic occlusion of her fallopian tubes using a Falope ring. How would you report this procedure? a. 58615 b. 58671 c. 58671-50 d. 58679-50 7. A 65-year-old male patient has an indwelling nephroureteral double-J stent tube replaced to treat a ureteral obstruction caused by a stricture from postoperative scarring. His stent tube is exchanged every two months to prevent occlusion in the stent, UTI, and loss of kidney function. Dr. Mott did this procedure via a transurethral approach under conscious sedation and provided the radiological supervision and interpretation. How would you report this procedure? a. 50605, 50382 b. 50385, 52283, 99143 c. 50385 d. 0084T 8. Dr. Blue provided interpretation and results for a needle electromyography for anal sphincter function. How would you report this service? a. 51784 b. 51784, 51785-51 c. 55875 d. 51785-26 9. A 48-year-old patient with BPH has his prostate removed via a laser enucleation. During this procedure he also has a vasectomy. What code(s) would report this procedure? a. 52648 b. 52649 c. 52649, 55250-51 d. 52647 10. What code series would you refer to for patients who have had a previous cesarean delivery and now present with the expectation of a vaginal delivery? a. 59400–59141 b. 59618–59622 c. 59610–59614 d. 59610–59622 11. How would you report a bilateral cadaver donor nephrectomy with cold preservation? a. 50300-50 b. 50320-50 c. 50234 d. 50300 12. 45-year-old male is going to donate his kidney to his son. Operating ports where placed in standard position and the scope was inserted. Dissection of the renal artery and vein was performed isolating the kidney. The kidney was suspended only by the renal artery and vein as well as the ureter. A stapler was used to divide the vein just above the aorta and three clips across the ureter, extracting the kidney. This was placed on ice and sent to the recipient room. The correct CPT code is: A. 50543 B. 50547 C. 50300 D. 50320 13. 67-year-old female having urinary incontinence with intrinsic sphincter deficiency is having a cystoscopy performed with a placement of a sling. An incision was made over the mid urethra dissected laterally to urethropelvic ligament. Cystoscopy revealed no penetration of the bladder. The edges of the sling were weaved around the junction of the urethra and brought up to the suprapubic incision. A hemostat was then placed between the sling and the urethra, ensuring no tension. What code should be used for this procedure? A. 57288 B. 57287 C. 52000, 57288 D. 52000, 51992 14. 16-day-year old male baby is in the OR for a repeat circumcision due to redundant foreskin that caused circumferential scarring from the original circumcision. Anesthetic was injected and an incision was made at base of the foreskin. Foreskin was pulled back and the excess foreskin was taken off and the two raw skin surfaces were sutured together to create a circumferential anastomosis. Select the appropriate code for this surgery: A. 54150 B. 54160 C. 54163 D. 54164 15. 5-year-old female has a history of post void dribbling. She was found to have extensive labial adhesions, which have been unresponsive to topical medical management. She is brought to the operating suite in a supine position. Under general anesthesia the labia majora is retracted and the granulating chronic adhesions were incised midline both anteriorly and posteriorly. The adherent granulation tissue was excised on either side. What code should be used for this procedure? A. 58660 B. 58740 C. 57061 D. 56441 16. 5-year-old male with a history of prematurity was found to have penile curvature, congenital hypospadias. He presents for surgical management for straightening the curvature. Under general anesthesia, bands were placed around the base of the penis and incisions were made degloving the penis circumferentially. The foreskin was divided in Byers flaps and the penile skin was reapproximated at the 12 o’clock position. Two Byers flaps were reapproximated, recreating a mucosal collar which was then criss- crossed and trimmed in the midline in order to accommodate median raphe reconstruction. This was reconstructed with use of a horizontal mattress suture. The shaft skin was then approximated to the mucosal collar with sutures correcting the defect. Which CPT code should be used? A. 54304 B. 54340 C. 54360 D. 54440 17. The patient is a 22-year-old who was found to be 7-1/2 weeks pregnant. She has consented for a D&E .She was brought to the operating room where MAC anesthesia was given. She was then placed in the dorsal lithotomy position and a weighted speculum was placed into her posterior vaginal vault. Cervix was identified and dilated. A 6.5-cm suction catheter hooked up to a suction evacuator was placed and products of conception were evacuated. A medium size curette was then used to curette her endometrium. There was noted to be a small amount of remaining products of conception in her left cornua. Once again the suction evacuator was placed and the remaining products of conception were evacuated. At this point she had a good endometrial curetting with no further products of conception noted. Which CPT code should be used? A. 59840 B. 59841 C. 59812 D. 59851 18. A 37-year-old female has menorrhagia and wants permanent sterilization. The patient was placed in Allen stirrups in the operating room. Under anesthesia the cervix was dilated and the hysteroscope was advanced to the endometrium into the uterine cavity. No polyps or fibroids were seen. The Novasure was used for endometrial ablation. A knife was then used to make an incision in the right lower quadrant and left lower quadrant with 5-mm trocars inserted under direct visualization with no injury to any abdominal contents. Laparoscopic findings revealed the uterus, ovaries and fallopian tubes to be normal. The appendix was normal as were the upper quadrants. Because of the patient's history of breast cancer and desire for no further children, it was decided to take out both the tubes and ovaries. This had been discussed with the patient prior to surgery. What are the codes for these procedures? A. 58660, 58353 B. 58661,58563-51 C. 58661, 58558 D. 58662, 58563-51 19. This gentleman has localized prostate cancer and has chosen to have complete transrectal ultrasonography performed for dosimetry purposes. Following calculation of the planned transrectal ultrasound, guidance was provided for percutaneous placement of 1-125 seeds. Select the appropriate codes for this procedure. A. 55860, 76942-26 B. 55875, 76965-26 C. 55860, 76873-26 D. 55875, 77778-26, 76965-26 Question 115 20. -year-old female in the OR for ectopic pregnancy. Once the trocars were place a pneumoperitoneum was created and the laparoscope introduced. The left fallopian tube was dilated and was bleeding. The left ovary was normal. The uterus was of normal size, shape and contour. The right ovary and tube were normal. Due to the patient’s body habitus the adnexa could not be visualized to start the surgery. At this point the laparoscopic approach was terminated. The pneumoperitoneum was deflated, and trocar sites were sutured closed. The trocars and laparoscopic instruments had been removed. Open surgery was performed incising a previous transverse scar from a cesarean section. The gestation site was bleeding and all products of conception and clots were removed. The left tube was grasped, clamped and removed in its entirety and passed off to pathology. What code(s) should be used for this procedure? A. 59150, 59120 B. 59151 C. 59121 D. 59120 21. 23-year-old who is pregnant at 39 weeks and 3 days is presenting for a low transverse cesarean section. An abdominal incision is made and was extended superiorly and inferiorly with good visualization of the bladder. The bladder blade was then inserted and the lower uterine segment incised in a transverse fashion with the scalpel. The bladder blade was removed and the infant's head delivered atraumatically. The nose and mouth were suctioned with the bulb suction trap and the cord doubly clamped and cut. The placenta was then removed manually. What code should be reported for this procedure? A. 59610, 654.21, V27.0 B. 59510, 669.61, V27.0 C. 59514, 669.71, V27.0 D. 59515, 669.71, V27.0 22 . 55-year-old female has a symptomatic rectocele. She had been admitted and taken to the main OR. An incision is made in the vagina into the perineal body (central tendon of the perineum). Dissection was carried underneath posterior vaginal epithelium all the way over to the rectocele. Fascial tissue was brought together with sutures creating a bridge and the rectocele had been reduced with good support between the vagina and rectum. What procedure code should be reported? A. 45560 B. 57284 C. 57250 D. 57240 23. A pregnant patient delivers twins at 30 weeks gestation. The first baby is delivered vaginally, but during this delivery, the second baby has turned into the transverse position during labor. The decision is made to perform a cesarean to deliver the second baby. The OB physician who performed the delivery also performed the prenatal care. The standard coding for this is: A. 59400, 59514-51, 651.01, 652.31 B. 59510, 59409-51, 651.01, 652.31 C. 59510-22, 651.01, 660.01, 652.31 D. 59510, 59409-51, 651.01, 660.30 24. A 30-year-old disabled Medicare patient is scheduled for surgery due to the finding of what looks like an ovarian mass on the right ovary. On entering the abdomen, the surgeon finds an enlarged ovarian cyst on the right, but the ovary is otherwise normal. The left ovary is necrotic looking. The decision is made, based on the patient’s age, to remove the cyst from the right ovary, but performs a left salpingooophorectomy. Code this encounter. A. 58720-RT, 58925-LT B. 58925-RT, 58720-51-LT C. 58925, 58720-50 D. 58720, 58925-51 25. 35-year-old male patient presented to an urologist because he was having continuous yeast infections and irritation on his penis. The physician recommended he have a circumcision. The physician performed the circumcision using a clamp with regional block. Code this procedure. A. 54150 B. 54160 C. 54161 D. 54150-52 26. A 55-year-old man with complaints of an elevated PSA of 6.5 presents to the outpatient surgical facility for prostate biopsies. The patient is placed in the lateral position. Some calcifications were found in the right lobe, with no obvious hypoechogenic abnormality. The base of the prostate was infiltrated and under ultrasonic guidance random needle biopsies were performed. A. 55700, 76872-26 B. 55706 C. 55700, 76942-26 D. 55700 27. A colposcope was introduced into the patient’s vagina and under direct visualization through a binocular microscope excessive lesions were revealed in and around the vagina. Electrocautery and laser vaporization were used to destroy the extensive number of vaginal lesions. What are the procedure and diagnosis codes? A. 57061, 623.8 B. 57065, 623.8 C. 57000, 621.9 D. 57120, 621.9 28. A pregnant patient is diagnosed with an incompetent cervix. The physician performs a cervical cerclage to prevent a missed abortion. After inserting a speculum into the vagina to view the cervix, the physician threads heavy suture material around the cervix using purse-string sutures. The sutures are pulled tight to make the opening smaller and prevent spontaneous abortion. What are the procedure and diagnosis codes? A. 57700, 654.50 B. 59320, 654.53 C. 59325, 622.5 D. 59899, 622.5 29. A patient is diagnosed with a bladder tumor. The physician performs a cystourethroscopy with fulguration and resects a 7 cm bladder tumor. Which CPT® code(s) would you use for this service? A. 52000, 52235 B. 52000, 52240 C. 52240 D. 52204, 52240 30. The patient has a positive pregnancy test, but ultrasound does not confirm a gestational sac in the first trimester. The physician diagnoses a blighted ovum and performs a suction D&C. What are the procedure and diagnosis codes? A. 59870, 631 B. 59820, 631 C. 58120, 631 D. 59840, 631 31. The physician performs a cystoscopy, bilateral retrograde pyelograms, removal of stent, and ureteroscopy on the left side at a hospital. DESCRIPTION: After satisfactory general anesthesia, and after routine preparation and draping in the lithotomy position. The urethra seemed to be free of lesions. There was no prostatic tissue. The bladder had two diverticula, one right end one left inferolateral wall, no lesions were noted, and the right was larger. Urine for cytology and FISH was sent. Residual urine was approximately 100 mL. Ureteral stent was seen in the left ureter. Right retrograde ureterogram revealed no lesions. The bladder was free of lesions. The stent was removed easily on the left side, and ureteroscopy was carried out into the renal pelvis with no lesions noted. Right retrograde pyelogram then revealed grade II-III dilatation of the ureter, grade I dilatation of the calices on the left side, and no other lesions. It was decided not to replace the double-J stent. The patient tolerated the procedure well and was sent to the RR in good condition. How would you code the procedure? A. 52310, 74420-26 B. 52332, 52000-59, 74420-26 C. 52310, 52000, 74425-26 D. 52332, 52310, 74425-26 32. A laparoscopic removal of the patient’s left testicle was performed on a 34-year-old patient who was diagnosed with testicular cancer. Code the encounter. A. 54522, 186.0 B. 58671, 257.8 C. 54640, 257.8 D. 54690, 186.9 33. A patient had three needle biopsies of the prostate completed under imaging and guidance. Which codes capture the professional services for this procedure? a. 55700 x 3, 76942-26 b. 10022, 55700 x 3, 76942-26 c. 55700, 76942-26 d. 55705 x 3, 10022, 76942-26 34. A Newborn baby boy Martinez underwent a procedure to slit the prepuce to relieve constriction that prevented retraction of the foreskin over the head of the penis. The slit tissue was sutured at the divided skin to control bleeding. The patient tolerated the procedure well. How would Dr. David report his services for this procedure? a. 54000-63 b. 54000 c. 54001-52 d. 54001-63 35. A patient underwent destruction of extensive condyloma lesions on the penis. The documentation stated 12 or more lesions were visible and treated during this session. The procedure was completed by laser technique. The patient received follow-up and post-procedure care instructions and was discharged in good condition. How should you report this procedure? a. 54057 x 12, 54065-59 b. 54065 x 12 c. 54057-22 d. 54065 36. A patient underwent an injection procedure for voiding urethrocystography with contrast. During the same investigative session, the physician completed all components of a urethral pressure profile study and a simple UFR including interpretation of the results. How should you report the professional services for this procedure? a. 51600, 74455-26, 51727-51, 51736-51 b. 51605, 74430-26, 51727-26, 51741-51 c. 51600, 74430-26, 51727-26, 51797-51 d. 51605, 74455-TC, 51727-26, 51736-51 37. A physician completed a cystourethroscopy with insertion of two permanent urethral stents. How should you report this? a. 53855 x 2 b. 52282 x 2 c. 52281, 53855-59 d. 52282 x 2, 52305-59 38. What modifier should be reported with the procedure code for transurethral resection of residual, or regrowth of, obstructive prostate tissue when the procedure is performed by the same physician during a postoperative period? a. -22 b. -52 c. -77 d. -78 39. Dr. Laura completed a vaginal delivery in the hospital for Stephanie, a 30-year-old patient. This is Stephanie’s first child and she delivered a healthy baby boy. Dr. Laura has taken care of Stephanie during the entire pregnancy and followed her through the postpartum period. Dr. Laura’s documentation stated that during the delivery admission, Stephanie required prophylactic antibiotics because she has mitral valve prolapse. How should Dr. Laura report the delivery care and diagnosis for this patient? a. 650, 424.0, V30.0, 59400 b. 424.0, 424.0, V30.0, 59510 c. 648.61, 424.0, V27.0, 59400 d. 414.0, 648.61, V27.0, 59614 40. Diane suffered a spontaneous incomplete miscarriage during the second trimester and required surgical completion of this event. How should this procedure be reported? a. 59812 b. 59820 c. 59821 d. 59840 41. An established patient required medical attention for removal of an impacted foreign body from the vaginal canal. Her physician documented a detailed history, detailed examination including enlargement of the vaginal opening with introduction of speculum, and identification of the foreign body as a tampon. The patient was asked to return to the office if she had any complications, fever, or abnormal discharge or heavy bleeding. How should you report the procedure? a. 99214-25, 57415 b. 99214 c. 57415 d. 57415-52 42. One week ago, Marion underwent a surgical laparoscopy with vaginal hysterectomy including removal of a 275-g uterus tube and ovaries due to cancer of the endometrium. Today she was admitted for a planned insertion of a vaginal radiation afterloading apparatus for clinical brachytherapy. During this procedure, the surgeon inserted the device and took x-rays to ensure placement. Once the device was in the proper location, it was fixed into position by tightening the applicator base plate and locking mechanism. Marion tolerated the procedure well and was sent to the recovery suite in satisfactory condition. How should today’s professional services be reported? a. 58554, 57156 -58 b. 57156 -59, 77326-26 c. 58554, 57156 -59, 77326-26 d. 57156 -58 43. What code should be reported for a diagnostic dilation and curettage for a patient experiencing heavy bleeding that is not associated with pregnancy? a. 58120 b. 59160 c. 57800 d. 57700 ANSWERS 1. “c” The code 50380 reports the auto-transplantation and re-implantation of a kidney. The parenthetical note under this code directs the use of the code for nephrectomy with modifier -51. 2. “b” The code 55875 represents the procedure and the code 77778 is the clinical brachytherapy. Code 77778 includes admission to the hospital and daily visits. You can find this rule in the subcategory guidelines for Clinical Brachytherapy in the CPT Professional Edition. 3. “a” This is a lithotripsy, extracorporeal shock wave treatment. You can find this procedure in the index of the CPT Professional Edition under Lithotripsy. 4. “d” You can find this answer in the CPT Professional Edition index under Excision, Lesion, Epididymis. Be careful with the index in this section and follow it to lesion or you may use the incorrect code. 5. “a” You can find this procedure in the index of the CPT Professional Edition under Repair, Penis, Injury. You would report modifier -79 for the unrelated procedure during a post-operative period by the same physician. 6. “b” The code 58671 reports this procedure via a laparoscopic approach. Modifier -50 is not necessary to report a bilateral procedure due to the code description of oviducts (which is bilateral). 7. “c” The code 50385 includes the conscious sedation, radiological supervision, and interpretation. The code defines a removal and replacement so there is one code to describe the entire procedure. 8. “d” The code 51785 describes this procedure. The guidelines under urodynamics indicate…“When the physician only interprets the results and/or operates the equipment, a professional component, modifier -26, should be used to identify physicians’ services.” 9. “b” You can find this code in the index of the CPT Professional Edition under Prostate, Enucleation. The vasectomy procedure is bundled with code 52649. 10. “d” You can find this information in the CPT Professional Edition under the Delivery After Previous Cesarean Delivery subsection. 11. “d” The code 50300 describes a donor nephrectomy (including cold preservation); from a cadaver donor, unilateral or bilateral. Because the procedure is described as a unilateral or bilateral procedure, you would not report modifier -50. 12. B This is a surgical laparoscopic procedure for removing the kidney (nephrectomy), eliminating multiple choice answers C and D. The whole kidney was taken out from a donor and put on ice (cold preservation), eliminating multiple choice answer A. 13. A Removal or revision of the sling is not being performed, eliminating multiple choice answer B. The procedure was an open surgery, eliminating multiple choice answer D. Cystoscopy procedure code is a separate procedure. According to CPT Surgery guidelines, “The codes designated as “separated procedure” should not be reported in addition to the code for the total procedure or service of which it is considered an integral component.” Meaning that the cystoscopy is included with the sling operation procedure since it was performed at the same time. 14. C The physician is not incising the membrane that attaches the foreskin to the glans and shaft of the penis (frenulum), eliminating multiple choice D. The patient is not having the circumcision for the first time, but needed a repair from a previous circumcision, eliminating multiple choice answers A and B. 15. D The key term to narrow your choices down is the removal of “labial adhesions”. This is found in the code descriptive for multiple choice answer D, 56441. 16. A Patient does not have a penile injury, eliminating multiple choice D. Code 54360, Plastic operation on penis to correct angulation is not correct because this patient has hypospadias and 54304 is the correct answer, thus eliminating multiple choice C. The surgery is not correcting a hypospadias complication, but straightening the curvature (chordee), eliminating multiple choice answer B. The correct answer is A, 54304. The penis was degloved and the foreskin divided into flaps to accommodate a plastic repair of the chordee. The hypospadias was not repaired at this time; however, the repair of the angulation is the first step before the hypospadias can be repaired. 17. B Patient is terminating her pregnancy by dilation and evacuation (D&E), eliminating multiple choice answer A. There is no documentation of this being an incomplete abortion, eliminating multiple choice answer C. The abortion was not induced by intra-amniotic injection(s), eliminating multiple choice answer D. 18. B One way to narrow down the choices is to code for the endometrial ablation using the hysteroscope. Since the endometrial ablation was done with hysteroscopic guidance, multiple choice answer A is eliminated. No biopsies were taken or polyps removed eliminating multiple choice answer C. The removal of her ovaries and fallopian tubes (oophorectomy and salpingectomy) were performed by a laparoscope, eliminating multiple choice answer D. 19. D Radioactive seeds were inserted directly into the prostate transperineally using needles (percutaneous), eliminating multiple choice answers A and C. There is a parenthetical note under code 55875 that states “For interstitial radioelement application, see 77776-77787“. A urologist may insert the hollow needles into the prostate (55875) and the physicist may insert the seeds into the needles. Some insurance companies permit one physician to report both the insertion of the needles and the seeds. 20. D Patient had started with a laparoscopic treatment for a tubal ectopic pregnancy. Due to the patient’s body size the laparoscopic approach was terminated, eliminating multiple choice answers A and B. The patient had the left fallopian tube removed (salpingectomy) removed, eliminating multiple choice answer C. When an laparoscopic surgical procedure fails, only the successful open procedure is reported (NCC Manual, version 6.1, April-June, 2000). Modifier -22 for unusual procedure would only be appended if the situation was truly unusual; therefore, it is not appropriate for this case 21. C There is no documentation that supports the patient had a previous cesarean, eliminating multiple choice answer A. There is no documentation that supports patient having antepartum care or will be having postpartum care with the obstetrician delivering the baby, eliminating multiple choice answers B and D. 22. C Patient is having a repair for a rectocele, not a cystocele, eliminating multiple choice answers B and D. The repair of rectocele was performed by a “posterior” colporrhaphy approach, eliminating multiple choice answer A. 23. B. According to CPT® guidelines, when twins are delivered, the global code (prenatal, delivery and post partum) is only reported once. When one twin is delivered via c-section select 59510 for the global procedure and the vaginal delivery only (54909) for the second twin. Modifier 51 is appended to indicate multiple procedures are performed. To code for the twin delivery in the ICD-9-CM manual, look up Delivery/twins, you are referred to 651.0X, the fifth digit being 1 indicating a delivery. The second diagnosis is coded due to the second twin being in a transverse lie, the reason for the cesarean. This is indexed under Delivery/ complicated / transverse/presentation or lie, referring to 652.3X, the fifth digit being a 1. 24.B. The removal of cyst from the ovary is coded 58925. The RT modifier is appended to indicate to the payer the ovarian cystectomy was performed on the right side. The removal of the salpingooophorectomy is coded 58720. Modifiers 51 and LT are appended to this procedure code since the removal of the ovary and fallopian tube was done on the left side and it was an additional procedure performed during the surgery. 25. A. Since this a 35-year-old patient getting a circumcision, that eliminates code 54160, which is for a neonate (28 days of age or less). The patient is having the circumcision performed using a clamp with regional block. Modifier 52 is not appended to 54150 since there is no indication in the encounter of the physician reducing the services provided. The procedure is performed as it is described by the CPT® code. 26. C. 55700 is the correct code since only needle biopsies were performed, without mapping the prostate under a template guide through a transperineal route. There are parenthetical notes under code 55700, which one states: (If imaging guidance is performed, use 76942). Since ultrasonic guidance (imaging guidance) was used, you would need to code 76942. Appending modifier 26 indicates the professional component; the procedure was done in an outpatient surgical center where the physician does not own equipment. 27. B. One way to get to the correct answer is to code for the diagnosis first. The procedure is being performed due to the patient having vaginal lesions. In the ICD-9-CM index, look up Lesion(s)/vagina. You eliminate multiple choice answers C and D. 57065 is the correct code since the scenario states that the laser surgery was used to destroy “extensive” number of vaginal lesions. 28. B. The physician performs a cervical cerclage. We know the patient is pregnant so 57700 is an incorrect code. We know the approach for this procedure is vaginally because the scenario states that a speculum is used to access the vagina to view the cervix. From the index look up cerclage/vaginal. You are referred to 59320. The patient is diagnosed with an incompetent cervix. In the ICD-9-CM index, look up incompetent/cervix/in pregnancy. The patient is pregnant so the fifth digit is “3”. 29. C. 52000 is a separate procedure, which indicates that only a cystourethroscopy is performed for diagnostic (examination) purposes only with no other procedure being performed at this time. For this scenario a surgical procedure was performed with the cystourethroscopy, eliminating multiple choice answers A and B. 52204 is not coded because biopsies were not taken from the bladder, leaving multiple choice answer C as the correct choice since a 7 cm bladder tumor was removed with fulguration. 30. D. The hint to narrow down your choices is a D&C (dilation and curettage) for a blighted ovum. This eliminates multiple choice answers A (there is no indication this was a hydatidiform molar pregnancy) and B (there is no indication that this is a missed abortion). 58120 is not the correct D&C, since this is an obstetrical (pregnancy) reason for the procedure. Blight ovum is indexed in the ICD-9-CM under Mole/pregnancy. 31. A. This patient is having a stent removed, eliminating multiple choice answers B and D, which should be used for insertion of a stent. You would not code 52000 since this is a separate procedure, which means that this code is only billed for diagnostic or examination purposes only, with no other procedures being performed at that time. A surgical procedure (removal of the stent) was done at the same time of the cystoscopy. Code 74420 is coded for the use of a retrograde ureterogram (urography). Modifier 26 is appended to report the professional component was performed. 32. D. You can narrow down your choices by first coding the diagnosis. The patient had testicular cancer; in the ICD-9-CM index go to the Neoplasm Table testis,testes/malignant/primary column where you are referred to code 186.9. This eliminates codes A, B, and C. 54690 is the correct procedure code since a laparoscopy was performed to remove the left testicle (orchiectomy). 33. c. One way to find this answer in the index of the CPT® Professional Edition is under the main term “Prostate,” then “Biopsy.” Notice that code 55700 indicates single or multiple, which means the code should be reported only one time per session. 34. b. Code 54000 describes a newborn; therefore, modifier -63 would not be reported with this code. The CPT® Professional Edition provides this information in the parenthetical note following this code. 35. d. Code 54065 includes extensive destruction of lesion(s) of the penis. This code is reported one time regardless of the number of lesions destroyed during a session. 36. a. Review of the subcategory notes in the CPT® Professional Edition with urodynamics indicates that modifier -51 should be used when more than one of these codes is listed in the same investiture session. 37. b. Code 52282 indicates stent (singular); therefore, when more than one stent is placed, the units should be reported. 38. d. The parenthetical notes provided in the CPT® Professional Edition with procedure code for resection of residual prostate tissue indicate modifier -78 would be appended if the procedure is performed by the same physician during a postoperative period. 39. c. The routine obstetric care, including the ante- and postpartum care with vaginal delivery, is reported with code 59400. The diagnosis codes for this case are assigned for the pregnancy complicated by cardiovascular disease. The mitral valve prolapse is then reported as the specific condition. According to the ICD-9 Guidelines for Chapter 11, these codes have sequencing priority. 40. a. One way to find this answer in the index of the CPT® Professional Edition is under the main heading “Miscarriage,” then “Incomplete Abortion.” 41. b. The CPT® Professional Edition provides a parenthetical note below code 57415 that references use of evaluation and management codes for impacted vaginal foreign body removal without anesthesia. This is an example of reading carefully to select the correct answer. The question does not ask for the evaluation and management code, only the procedure; therefore, answer A is not correct. 42. d. According to CPT® Changes: An Insider’s View 2011, this new code includes x-ray confirmation forlocation of the apparatus. 43. a. Code 58120 is described as non-obstetrical, whereas 59160 is used for postpartum hemorrhage.