1
DEVELOPING PAYER RELATIONS
August 14, 2013
William J (Bill)TenHoor
AHP Healthcare Solutions
2
Objective
Gain a better understanding of
payers and the process of
making them your clients long
term
3
Telling the Payer Relations Story
1. Beginning
2.
Middle
3.
End
4
Why Focus on Payer Relations Now?
• The ACA implements an insurance based payment
system – many payers are now your potential clients
• Reliance on grants is increasingly less feasible
• Paradigm shift is occurring rapidly
From MH & SA to Behavioral Health to a Health Specialty (Behavioral Medicine?)
Care coordination, primary care integration and quality measures are essential
components of care delivery
Population health and wellness are key parts of delivery systems
Payment models are shifting from fee-for-service to pay-for-performance to risk
models like shared savings and related types of capitation
Insurers and providers are integrating within ACOs, creating the opportunity for
more friction free health systems
• Behavioral health has greater legitimacy and visibility
(parity) to leverage – one of the 10 Essential Benefits
• Tempest Fugit!
5
Beginning Steps
1. Prepare
2. Understand the payer
3. Define your value equation
4. Engage in a systematic sales process
5. Formalize your agreements in a contract
6. Sustain your success – learn from (and be
prepared for) setbacks along the way
6
1. Prepare
DEFINITIONS
1. It’s a journey
2. It’s a process
3. It’s a relationship
7
2. Understand Healthcare Payers
• What are the types?
• Commercial/Private
• For-profit (stock and mutual) and non-profits
• Public
• HMOs, PPOs, Indemnity Plans
• Why and when formed and how they have evolved
• Experience of the Blues and the depression
• Discover their values, brand, how regulated, PR,
operations, personnel
8
Health Insurance Is Not a Human Service
Characteristics
1
1. Pooling of losses
2. Payment for
random losses
3. Risk transfer
2
3
4. Indemnification for
illness
Insurer charges individual $250. to cover the risk of
extreme illness and/or potential bankruptcy
(Anticipated care cost ($200) + risk & overhead charge
($50) = premium)
9
The Payer Pie: Market Segments
Public Sector
• Medicaid and SCHIP
• Medicare
• SAMHSA/VA/DOD/HRSA
• State and Local Govt.
Private Sector
• Commercial and non-
profit Insurers
• Large and small group
• Individual
• Self-Insured Employers
• Individual Out-of-Pocket
• Also mention third
(MBHO) parties and
MSO/ASO entities
10
The Payer Pie: Health & BH Spending
Behavioral Health and Total Health
Spending: Public and Private Sector
Segments (in 2005 $)
Private
Public
$955
$760
$83
$52
MH/ SA $
Health $
Private
MH/ SA $
$52
Health $
$955
Public
$83
$760
• What our market
research tells us:
• MH/SA = 5.1% of
Private Health
Spending
• MH/SA is 9.9% of
Public Sector
Health Spending
• Conclusion:
Target Public
Sector Payers
First
• Source: (SAMHSA
2010; Kaiser
Report, 2011)
11
US BH Spending: $135 B
Other Private, 3%
Medicaid, 26%
Private Insurance, 24%
Out-of-Pocket, 1%
Medicare, 7%
Other State and Local,
21%
Other Federal, 7%
12
The Payer Pie: Public BH Spending
MH + SA Public Sector Spending Segments ($ in billions)
$35.0
• What our market
research tells us:
•
$31.1
$30.0
•
$25.0
•
$20.3
$20.0
•
$15.0
$10.0
$8.6
$7.9
$4.6
$5.0
$-
$5.7
•
$3.5
$1.5
Medicare
Medicaid
State& Local Gov
$31.1
SAMHSA/VA/DO
D
$5.7
MH
$8.6
SA
$1.5
$4.6
$3.5
$7.9
$20.3
•
Medicaid is the dominant
payer segment at 43%
State/Local Govt. is
important at 34%
State/Local Govt. is very
impt. for SA at 38%
SAMHSA contributes only
modestly to pie
Conclusion: Funding
from 4 public sector
segments enables
diversification
SA-only providers may
want/need MH services
also
13
ACOs as Payer Prospects
• Important as new ACA models (several hundred in operation)
• Combine payer and provider features
• Are being encouraged and incentivized
• Iowa is encouraging (cannot mandate) Medicaid Expansion members
to join ACOs
• What makes one a good prospect?
• Has status in the community
• Already has enrollment or may be new to the state
• Needs your services
• You have an opportunity for preference and even exclusivity
• References
• www.accountablecarenews.com
• http://www.ncsl.org/issues-research/health/accountable-care-organizations-health-costs.aspx
14
3. Define Your Value Proposition
• The promise of the value to be derived from your services
by a customer (both insurer and individual consumer)
• Is the customer satisfied?
• What is the “proof” of the customer experience?
• Requires ability to communicate the offering and the
associated features and benefits
• Differentiates the organization - positions it against
competition
• Who uses the value proposition
• The organization, internally, to ensure communication consistency
• Customers, partners, employees, other stakeholders
Proposition: Comorbidity & Chronic Conditions
Source: Wyatt Matas, 2013
16
4. Engage in a Systematic Sales Process
Don’t simply accept the perfunctory provider contract
route - Alternative Sales Process – Must be customized
Identify opportunities in the markets
Define best prospective clients (payer, ACO, hospital, FQHC, etc.)
Pre qualify and focus on the most qualified client first
1)
2)
3)
1)
4)
5)
6)
7)
8)
Internet, phone, face to face meeting (but this is not selling – see next slide)
Contact prospective payers to ensure interest and need
Make a sales presentation
Prepare and submit the proposal
Proposal follow-up
Close/Negotiate
• Adapted from Pete Frye’s “The Complete Selling System”
17
Example: Qualification and Pre-Qualification
• Following pleasantries, make a value statement –
• “We have care coordination services that ensure people with
substance use disorders regularly act on their problematic physical
health conditions as well as their substance issues”
• Reconfirm the value issues
• Does this prospect need our solution, want to do something about it,
and can we determine what we have to do to make the sale?
• Establish buying criteria, using and reconfirming informational
and knock-off questions
• Providers must be accredited, licensed, etc.
• Gain appropriate commitments
• Establish a written agenda (what has to happen to make the
sale)
• Identify a coach (an internal source for land mines, risks, etc.)
• Identify the next step and its objective
18
5. Formalizing the Agreement
• Agreements (contracts) consummate the deal
• Aspire to more than a traditional provider contract
• They are in many parts
• Key aspects of a contract
• Memorializes intention to create a legal obligation
• Mutual assent
• Involves offer and acceptance
• Remember, contracts represent large portion of asset
value of a service business, deserving appropriate
attention
19
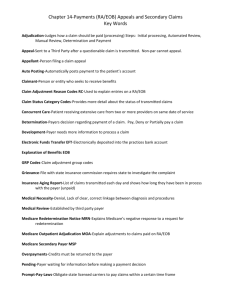
Many Important Parts
• Definitions – ensuring clarity
• Scope of covered (and non-covered) services
• Full capabilities of the provider, such as prevention/wellness
• Scope of license of providers
• Covered products (both Medicaid and commercial?)
• Compensation and payment processing
• Term, termination, post-termination, severability
• New AQCs are 3-5 year contracts
• UR/UM, QA, clinical coordination practices, guidelines and standards
(medical necessity)
• Privacy, reporting and recordkeeping
• Member eligibility, enrollment & disenrollment
• Procedures – negotiate greater MCO responsibility
• Verification (and risk of error) and effective date
20
Negotiation is a Key Part of Contracting
• The process of reaching
agreement that meets your
interests better than your
best “no deal” option
• “The art of letting the other
party have your way”
Daniele Vare
Good Deal
No Deal
Bad Deal
Many FACTORS affect your interest in and the shape of a deal,
such as price, timing, scope, operational considerations, value
perceptions, exclusivity, competitor impacts, territory/place, etc.
21
6. Structure and Manage for Success
• Build a Team - One person cannot handle all functions
• Business Development
• Developing and executing the strategy for the organization
• Leading growth and change
• Sales (and account services)
• Ensuring the growth plans of the organization are achieved by winning new
business, serving existing clients well and growing their business
• Marketing and Product Development
• Creating, communicating & delivering goods and services of value
• Producing the intelligence and research to support organizational strategy
• Shaping and conveying the brand of the organization to all stakeholders
• Public/Governmental Relations
• Maintaining good faith and reputation with communities & regulators
• Enables reactive capability, a “must have” when highly public
22
The Middle - Now I’m In. What Next?
Provide Account Management/Client
Services
• Ensure successful use of your services,
particularly start-up (model office & cut-over)
• Recommend new services or upgrades
• Maintain ongoing relationships with all key
decision makers
• Gain leads, references, service development
intelligence
• Develop and maintain account records
23
Other Account Management Practices
• Assign the right person for managing the client
and the business relationship
• Require project management skills/experience
• Require interpersonal skills necessary for
relationship building/management
• Document and operate by pre-defining expected
practices
• Make course corrections as necessary
• Raising and resolving problems
• Act on client problems
24
The End
• One view: there is no end, only the opportunity for
improvement
• How will you know when exit is the right next step?
• ACO headlines 7/16
• Seven Medicare Pioneer ACOs that didn't produce savings in the
first year … have told the CMS they will leave the Pioneer program
and enter the Medicare Shared Savings Program model, while
another two participants have indicated they will leave Medicare
ACO entirely
25
Questions & Discussion
Bill TenHoor
bill@tenhoor.com
© 2012 by Advocates for Human Potential –
Healthcare Solutions. All rights reserved. No part of
this document may be reproduced or transmitted in
any form or by any means, electronic, mechanical,
photocopying, recording, or otherwise, without prior
written permission of AHP.