ECG_07 (Intraventricular block)
advertisement

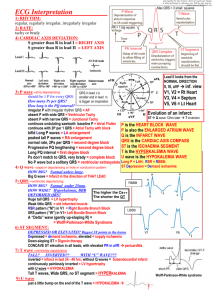
ECG tutorial (Intraventricular block) INTRODUCTION 1. Bundle branch and fascicular blocks are frequently seen in those with and without cardiac disease. These patterns are defined by variations in QRS duration and voltage compared to normal. By convention, deflections on ECG that are > 0.5 mV (> 5 mm with standard calibration) are referred to in capital letters; smaller deflections are noted in lower case. Thus, qRs pattern means that q and s waves are small and R wave is large. LEFT ANTERIOR FASCICULAR BLOCK (LAFB) 1. LAFB is characterized by pathologic left axis in frontal limb leads, defined as axis > -45º or > -60º, depending upon author, up to -90º. This may be result of conduction system disease in anterior fascicle of left bundle, or may occur when there is disease or fibrosis surrounding left 2. 3. anterior fascicle (with MI). QRS measures < 0.12 seconds in duration. QRS complexes in lead I are upright; in inferior leads II, III, and aVF they are negative (small R wave, deep S wave). There is small q wave and tall R wave in lead aVL, and time to peak of R wave in aVL is ≥ 0.045 seconds. There is often tall R wave in aVR and poor R wave progression in leads V1-V3. IMI also has left axis as result of large Q wave in inferior leads. This is due to fibrotic tissue rather than conduction system disease. If there is QR complex due to MI, pattern has been called peri-infarction block. Therefore, LAFB cannot be diagnosed in presence of IMI. LEFT POSTERIOR FASCICULAR BLOCK (LPFB) 1. LPFB occurs when there is conduction system disease involving posterior fascicle of left bundle branch. It is defined as pathologic right axis, > +90º (some authors use even more rightward axis of 120º) up to 180º. QRS complex is < 0.12 seconds. There are small R and deep S waves in leads I and aVL, and small Q and tall R waves in leads III and aVF. 2. However, there are other causes of RAD that need to be considered and excluded before LPFB can be diagnosed, ie, LPFB is diagnosis of exclusion. Other causes for RAD include LMI, where there is QR in leads I and aVL; RVH, in which case there is tall R wave in lead V1; R-L arm lead switch, with negative P wave, QRS complex, and T wave in leads I and aVL; dextrocardia, which resembles R-L arm lead switch and also has PRWP across precordium; and WPW with pseudo LMI pattern. RIGHT BUNDLE BRANCH BLOCK (RBBB) 1. Incomplete RBBB A. An incomplete RBBB is present when there is slowing of or delayed conduction through RBB. It may also be seen with delayed activation of RV within RV myocardium. Although this is often termed incomplete RBBB, it is actually intraventricular conduction delay of B. RV as bundles exhibit all or none conduction rather than incomplete conduction. Activation of septum and LV myocardium is unaffected; thus, initial part of QRS complex is normal (septal Q waves followed by R wave). However, delay in RV myocardial activation causes it to occur after LV activation rather than simultaneously, thereby altering terminal portion of QRS complex. The delayed RV forces are directed from L to R, leading to tall secondary R wave (R') in rightward directed leads, and deep terminal S wave in leftward leads. Thus, there is rsR' in leads aVR and V1-V2, and qRs morphology in leads I, aVL, and V5-6. However, QRS complex width is only slightly prolonged, between 0.10 and 0.12 seconds, since there is only minor delay in RV activation that still occurs via RBB; hence, this is considered intraventricular conduction delay. Incomplete RBBB may be erroneously seen if V1 ECG lead is placed higher than 4th intercostal space or more right than parasternal area. Complete RBBB C. 2. A. A complete RBBB is result of total block of impulse conduction along RBB, leading to delayed and abnormal activation of RV myocardium occurring from LV myocardium. The LBB is not affected; thus, activation of septum and LV myocardium is normal, occurring first from L to R (septal depolarization) and then from R to L (ventricular depolarization). This is then followed by RV activation. B. C. The overall appearance of QRS is RsR’ complex in leads V1-2, commonly called “rabbit-ear” pattern, and deep, broad S wave in leads I, aVL, and V5-6. The width of QRS complex is > 0.12 sec. RBBB also results in abnormality of ventricular repolarization of RV myocardium. Thus, there are often secondary ST segment and T wave changes present in right precordial leads V1-V3, including STD and TWI. ECG in RBBB can be best understood in terms of early anterior vector, mid-temporal and usually posterior vector, and delayed terminal rightward vector. The following are common observations. i. ii. iii. Early anterior and rightward vector — Initial septal activation depends on fibers of left bundle, as depolarization proceeds from L to R. The initial 30 msec of activation is not quite normal in RBBB, since some normally opposing rightward forces are not present. Nevertheless, ECG appearance is essentially normal in that anterior and rightward vector results in q wave in leads I, aVL, and V6; and r wave in leads V1, V2, and aVR (waveform 5). Mid-temporal leftward and usually posterior vector — The initial rightward vector of septal activation is followed by leftward and posterior vector induced by subsequent LV activation. The wave front completes depolarization of LV between 40 and 60 msec, resulting in R waves in I, aVL, and V6 as well as s (or S) in V1 and V2. This appearance is usually similar to that in normal subjects. Delayed terminal rightward vector — The asynchronous depolarization caused by RBBB is primarily manifested in later portion of QRS complex, at 80 msec and beyond. Since abnormal and delayed RV activation occurs from L to R and goes through ventricular myocardium and not His-Purkinje system, forces generated by right septal and right ventricular free wall activation predominate, resulting in terminal rightward and anterior positivity. This also results in S waves in leftward directed leads (I, aVL, and V6), and 2nd positive deflection is usually large (R'), in anterior-posterior leads (V1 and V2). D. As LV activation is normal, abnormalities of LV can be still recognized, such as acute and chronic myocardial ischemia or infarction, LVH, and pericarditis. The RV activation sequence is abnormal, however, and abnormalities of RV myocardium cannot be recognized (RVH). RBBB does not lead to axis deviation. E. Some patients have atypical pattern with loss of S wave in V1 due to anterior displacement of usually posterior mid-temporal forces, resulting in rsR', qR, or M-shaped QRS pattern in V1. There are 3 mechanisms that can account for this pattern: normal variant; gain of mid-temporal anterior forces due to RVH or concurrent LAFB; and loss of posterior forces due to PMI. LEFT BUNDLE BRANCH BLOCK (LBBB) 1. Incomplete LBBB A. 2. An incomplete LBBB occurs when there is slowing or delay of conduction through LBB, or diffusely through Purkinje system and ventricular myocardium. This causes widening of QRS complex to 0.10 to 0.12 seconds and loss of septal q wave in leads I and V5-6. They will usually have pattern resembling LVH and time to peak of R wave in leads V4-6 is > 0.06 seconds. Complete LBBB A. Complete LBBB develops as result of conduction delay or block within LBB, leading to delayed and abnormal activation of LV myocardium occurring from RBB and RV myocardium. LV activation originates from RBB in R to L direction, in contrast to normal situation in which first part of LV myocardium to be activated is septum via small septal B. C. branch of left bundle, with subsequent impulse spread in L to R direction. In common or typical complete LBBB, conduction sequence is to left and asynchronous activation of 2 ventricles with delayed and slowed LV activation increases QRS duration. The following changes are seen on ECG. i. ii. iii. iv. QRS interval is prolonged > 0.12 seconds since LV activation is abnormal, delayed, and slowed due to conduction of impulse through ventricular myocardium rather than His-Purkinje system. There are no septal Q waves in leads I and V5-V6; instead there is tall monophasic broadened and abnormal R wave in these leads. Occasionally, small q wave may be seen in aVL. The time to peak of R wave is > 0.06 seconds in leads V5-6. There is QS complex that is abnormal and widened in leads V1-V2, though small R wave may be seen (rS complex). v. There are no L-to-R forces and hence there cannot be terminal S waves in leads I or V6. vi. QRS axis may be normal, but is frequently leftward. Occasionally, it may be superior or rightward. ST and T wave abnormalities may be present, including STD and TWI, in opposite direction from QRS complex. These changes of myocardial repolarization are secondary to abnormal ventricular activation. Positive concordance, where QRS and T waves are both upright, may be seen as normal. Negative concordance, with both negative QRS and T wave, is abnormal and would be concerning for ischemia/infarction. It is not possible to diagnose other left ventricular abnormalities in presence of vii. viii. LBBB due to abnormal conduction through LV. D. The electrocardiographic pattern in LBBB can be best understood in terms of 3 vectors. i. Early and usually leftward vector — The normal sequence of activation at 10 msec (0.10 sec) is anterior and to right (representing septal activation), resulting in small q waves in I, avL, and V6 with rS in V2. In comparison, initial 10 msec vector in LBBB has two characteristics. First, direction of activation is reversed, traveling from R to L (as there is absence of septal activation that results from septal or median branch of LBB). Second, activation also travels from apex to base and to right ventricular apex and free ventricular wall. However, septum is larger structure than RV free wall; thus, septal activation predominates. The resultant vector is to left and usually ii. iii. anterior, resulting in loss of normal q wave and initiation of wide, slurred R wave in I, aVL, and V6. In addition, rS or QS pattern is seen in V1. "Pseudonormalization" of septal depolarization in LBBB (reappearance of q wave in I and V6) may reflect septal infarction. Mid-temporal leftward and posterior vector — Depolarization continues in ordinary myocardial cells of septum from apex to base. From 20 to 60 msec, spatial vectors are oriented to left and posteriorly since LV is leftward and posterior structure. The spatial vector that appears at 80 msec represents mass of LV myocardial depolarization, resulting in signal of large amplitude. The amplitude of signal is further increased by 2 factors: terminal vectors are not countered by RV forces since RV has already been depolarized; and thick posterobasal portion of LV is activated before thinner anterolateral wall. Terminal leftward vector — The terminal 10 msec vector and beyond result from depolarization of anterolateral wall of LV which is thinner than posterobasal region, producing small vector that is also directed to left and posteriorly. Infarction of anterolateral wall will decrease or actually reverse the direction of terminal vector. INTRAVENTRICULAR CONDUCTION DISTURBANCE 1. IVCD is result of diffuse slowing of impulse conduction involving entire His-Purkinje system, resulting in generalized delay in activation of ventricular myocardium. It is diagnosed in presence of QRS duration > 0.10 sec, and QRS morphology does not resemble either typical LBBB or RBBB. This can include appearance of RBBB in limb leads and LBBB in precordial leads, or reverse. BILATERAL BUNDLE BRANCH BLOCK (BBBB) 1. BBBB is caused by diffuse disease involving both bundles. If conduction within both bundles is completely blocked, no impulse is able to reach ventricles and there is complete or 3rd degree AVB. This leads to ventricular asystole or ventricular escape rhythm. 2. BBBB also may be diagnosed when there are QRS complexes that occasionally have LBBB morphology and occasionally have RBBB morphology. Often every other complex is right or left bundle. This is also termed alternating bundle branch block, and is worrisome sign for development of complete heart block. INTERMITTENT BUNDLE BRANCH BLOCK 1. Intermittent bundle branch block, either right or left, is diagnosed on ECG when there are occasional QRS complexes with RBBB or LBBB morphology (but not both RBBB or LBBB), interspersed with QRS complexes that have normal morphology. Most often intermittent bundle branch block is rate-related; thus, RR intervals of QRS complexes manifesting bundle branch block are shorter when compared to intervals of normal QRS complexes. In other cases there is no rate related change in QRS intervals, but occurrence of the bundle branch block is random or sporadic event. RATE RELATED BUNDLE BRANCH BLOCK 1. Rate-related BBB conduction is present when QRS complex during tachycardia is wider (usually > 0.12 seconds) when compared to QRS duration during slower sinus rhythm. The aberrated QRS complexes may have appearance of RBBB, LBBB, IVCD, or from bypass pathway; important diagnostic feature is that expression is usually influenced by HR. 2. 3. 4. Rate-related aberration is result of slowed and delayed conduction within bundle of His or right or left bundle branches. This may be due to intrinsic disease of conducting system or depressant effects on conduction from AAD or hyperkalemia. If rate of impulse stimulation is faster than ability of that part of conduction system to have repolarized from prior impulse, impulse may fail to conduct through part of His Purkinje system (only right or left bundle). There is a critical heart rate above which the impulse is conducted by only one of bundles, or is conducted with diffuse slowing throughout the His Purkinje system resulting in nonspecific intraventricular delay. Thus, there is rate-related widening of QRS complex occurring when HR increases. The block is most often in right bundle, which generally has longer refractory period than left bundle at similar HR; thus, RBBB configuration is the most common morphology for aberrated QRS complex. However, in patients with underlying heart disease, particularly coronary heart disease and fibrosis of left septum, LBBB morphology is not uncommon. Aberrancy may also be seen when single atrial or junctional premature beat arrives at RR interval (or rate) that is faster than the conduction system can conduct. The single premature beat is conducted aberrantly, usually when there is a critical coupling interval between the preceding sinus QRS complex and the premature beat; premature beats that occur later in diastole may be conducted normally. 5. Ashman's phenomenon A. Aberrancy is due in some cases to physiologic changes of conduction system refractory B. periods that are associated with RR interval cycle length. A relationship exists in normal circumstances between refractory period of His Purkinje system and HR: there is a decrease in refractory period as HR increases (even if abruptly); the refractory period lengthens as HR slows. If there is long RR interval (due to slow HR), followed by short interval (premature atrial complex), the signal from short interval may encounter refractory period of one of bundles and demonstrate RBBB or LBBB pattern. This is known as Ashman’s phenomenon. Ashman’s phenomenon is most commonly observed during Af when there are frequent episodes of long-short RR cycle lengths. However, it may occur whenever there is abrupt change in rate (slow or long RR interval to fast or shorter RR interval). Hence, it may be seen with abrupt onset of any supraventricular tachyarrhythmia. The aberrancy may be present for one beat and have morphology that resembles VPC, or may involve several sequential complexes, which may give the appearance of ventricular tachycardia. C. It is often difficult to distinguish VPC from aberrantly conducted or Ashman's beat in presence of Af and in most cases is not clinically relevant. i. VPC is usually followed by longer RR cycle, indicating occurrence of compensatory pause, the result of retrograde conduction into AV node and antegrade block of impulse originating in atrium. If there is persistence of aberration at same HR after the first beat, this suggests ventricular origin. ii. The absence of long RR-short RR cycle associated with wide or aberrated QRS complex suggests that it is of ventricular origin. iii. Aberrancy is not present if, with inspection of long ECG rhythm strip, there are RR cycle length combinations that are longer and shorter than those associated with the wide QRS complex. D. A ventricular origin is likely if there is fixed coupling cycle between the normal and aberrated QRS complex when seen repeatedly. 6. Bradycardia dependent aberrancy A. In patients with bradycardia-dependent aberrancy, BBB occurs after longer pause or RR interval, which is the opposite of Ashman’s phenomenon. This has been termed phase 4 block. It is generally unexpected since there should be sufficient time for bundles to recover and conduction to be normal after long cycle. Three explanations have been postulated. One explanation is that bundles are serving as pacemaker tissue and manifest spontaneous automaticity. This pacemaker tissue is no longer suppressed by stimuli from upper pacemakers when the cycle length is very prolonged, leading to generation of impulse from one of bundles and manifesting block pattern in other bundle. Another explanation is that HR is slowed as a result of enhanced vagal tone, which also leads to impaired or slowed conduction through a bundle. Lastly, similar to paroxysmal atrioventricular block, there is disease in the bundle which leads to a spontaneous increase in phase 4 depolarization and sodium channel inactivation, preventing conduction down the bundle until it can be reset. 7. Pre-excitation syndrome A. The presence of accessory pathway that conducts antegrade, such as occurs in WPW or other pre-excitation syndrome, may give general appearance of RBBB or LBBB pattern, though subtle differences are seen that demonstrate atypical features of RBBB or LBBB. In combination with short PR interval, this is reflection of pre-excitation, and RBBB and LBBB cannot be accurately diagnosed. SUMMARY 1. 2. 3. 4. LAFB is characterized by pathologic LAD in frontal limb leads, defined as axis > -45º to > -60º, with QRS < 0.12 seconds, qR in lead aVL and peak time to R wave in aVL ≥ 0.045 seconds. LPFB is defined as pathologic right axis, > +90º (some authors use an even more rightward axis of 120º), when there is no other etiology. QRS complex is negative (small R and deep S) in leads I and aVL, and positive (tall R wave) in leads III and aVF and QRS < 0.12 seconds. RBBB is characterized by. A. A RsR' complex in leads V1-2, often called a “rabbit-ear” pattern. B. A deep and broad S wave in leads I, aVL, and V5-6. C. The width of QRS complex is > 0.12 seconds. LBBB is characterized by. A. B. C. D. E. Absent q waves in I and V5-6. A QS complex which is abnormal and widened in leads V1-V2. Time to peak R wave > 0.06 seconds in leads V5-6. ST and T wave abnormalities. The width of QRS complex is > 0.12 seconds.