Patient Engagement and Coaching Models
advertisement
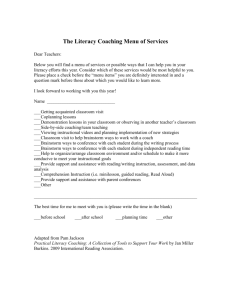
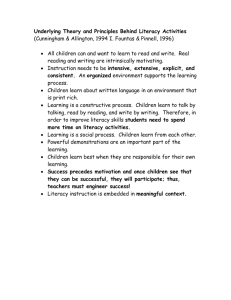
Patient Engagement and Coaching Models Rebecca Durham Project Coordinator, HealthInsight Incorrect Assumptions Incorrect Assumptions • Patients want to change behavior • Advising optimal health is motivator for change • Patients are either motivated to change, or not Change Our Thinking From • Patients are Non-Compliant To • Patients are unsuccessful at managing their own care • Patients are not yet engaged in their own care Consider… • Chronically ill patients make many daily health decisions • Sometimes make unwise decisions • Don’t fully understand implications of particular health decisions • Lack support to make better choice • 9/10 patients lack skills to manage their health/prevent disease1 1. Advocate for Health Literacy in your organization (n. d.). Quick Guide to Health Literacy. Retrieved from http://HHS.com How to Not Engage Patients • Tell patients what to do (give advice) • Misjudge sense of importance regarding behavior change • Use scare tactics, argue, blame them for no willpower and self-concern • Overestimate readiness to change and degree of confidence • Take away control, generating resistance How To Engage Patients • Listen: Don’t jump on first things patients say • Understand behavior change and motivation • Change clinical visits from “to-do” lists to helping patients identify and establish care priorities • Help patients develop a care plan to improve outcomes (Shared Care Plan) Can We Be Engaged? • 23% adopted new health behaviors (but unsure could maintain if stressed) • Remaining 77%: -- Remain passive recipients (12%) -- Lack basic facts to follow treatment recommendations (29%) -- Have facts, no skills/confidence (36%) Hibbard, J. H., Mahoney, E. R., Stock, R., & Tusler, M. (2007). Do increases in patient activation result in improved self-management behaviors? Health Services Research, 42, 1443-1463. Polling Question What is the most important determinant to advance patients’ with diabetes healthy behaviors? 1. Increasing patient education 2. Spending more time with patients 3. Developing a shared relationship between patient and provider Norris, S. L., Engelgau, M. M., & Narayan, K. M. V. (2001). Effectiveness of self-management training in Type 2 diabetes. Diabetes Care, 24, 561-587 Ideal PCC Approach Tennison, J. (2012) Education + Self-Management • Information, technical skills • Problems due to poor disease control • Disease-specific knowledge • Goal is behavior compliance to improve outcomes • Skills to act on problems • Patients ID problems in self-management • Improving patient confidence to change • Goal is increased self-efficacy to improve outcomes Bodenheimer, T., & Abramowitz, S. (2010). Helping patients help themselves: How to implement self-management support. Oakland, CA: California HealthCare Foundation. The Facts • 40-80% medical information given forgotten immediately; half retained is incorrect1 • Physicians thought 89% of patients understood medication side effects, only 57% of patients understood2 1. Kessels, R. P. (2003). Patients' memory for medical information. Journal of Social Medicine, 96(5), 219-222. 2.Training to Advance Physicians‘ Communication Skills. (n. d). Retrieved from AHRQ Website. Medication Adherence? Take 3 tablets by mouth 2 times per day, with food for 14 days, then take 2 tablets 2 times per day with food for 14 days, then take 1 tablet every morning, 30 minutes before meal for 14 days, then take ½ tablet every morning, 30 minutes before meal for 14 days Teach-Back Method • Method to confirm patients understand their medication/treatment: – “Tell me why you need this medication” – “Tell me how you take this medication” • Teach Back not a test of patients’ knowledge • Is a test of how well we explain something Kessels, R. P. (2003). Patients' memory for medical information. Journal of Social Medicine, 96(5), 219-222. Health Literacy • The capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. Healthy People. (2010). Cited in What is Health Literacy? Retrieved from www.chcs.org • Only 12% of adults have proficient health literacy • Lower literacy = more admissions, ER visits, costs, higher risk of poor health Advocate for Health Literacy in your organization (n.. d.) Quick Guide to Health Literacy. Retrieved from http://HHS.com Keep Your Glucose in Normal Range Watch Your Words Problem Word Ailment Adverse Benign Condition Lesion Oral Vertigo Consider Using Sickness, illness Bad Won’t cause harm, isn’t cancer How you feel; health problem Wound, sore By mouth Dizziness Ask Me 3. Retrieved from www.npsf.org. What is Coaching? • Managing: Making sure people do what they know how to do • Training: Teaching people to do what they don’t know how to do • Mentoring: Showing how those who are good at doing things do them • Coaching: Helping identify skills and capabilities, and empowering people to use them as best they can Motivational Interviewing A collaborative, patient-centered form of guiding to elicit and strengthen motivation for change Miller, W. R. & Rollnick, S. (2009). Ten things that Motivational Interviewing is not. Behavioural and Cognitive Psychotherapy, 37, 129- 140. Motivational Interviewing • Non-judgmental, non-confrontational, non-adversarial • Explore and resolve ambivalence • Help patients envision a better future, and become increasingly motivated to achieve it Miller, W. R. & Rollnick, S. (2009). Ten things that Motivational Interviewing is not.. Behavioural and Cognitive Psychotherapy, 37, 129- 140. Four Principles of MI 1. Express empathy (not pity) - Put yourself in patients’ shoes 2. Develop discrepancy (ambivalence) - Explore how they want their life to be and how it is now 3. Roll with resistance (expect it) 4. Support self-efficacy (empower) OARS • • • • Open-ended questions Affirmations Reflections Summaries Care Transitions Coaching Model • Improve transitions of care • Transitions Coaches encourage patients and caregivers to take a more active role in their own selfcare • Not doing for, but empowering patients to do for themselves • Involves pre-discharge and then follow-up, in-home visits Transitions Coaching in Your Practice • A tool everyone can use • Patients engaged in coaching have better outcomes • Effective to avoid downward trends, or keep patients at new “normal” • Program consistently reduced 30-day hospital readmissions and costs, and 180-day hospital readmissions Discussion Question #1 How will I use patient engagement techniques to improve patient outcomes? Discussion Question #2 Name two times during an encounter when you might engage a patient using a patient engagement or coaching model