NUR201-ModuleGSlides
advertisement

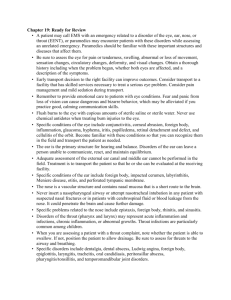
SENSORY/PERCEPTUAL EYE ALTERATIONS REFRACTIVE ERRORS OVERVIEW A. THE ABILITY OF THE EYE TO FOCUS ON THE RETINA DEPENDS ON THE LENGTH OF THE EYE FROM FRONT TO BACK & THE REFRACTIVE POWER OF THE LENS SYSTEM B. REFRACTION IS THE BENDING OF LIGHT RAYS C. PROBLEMS IN EITHER EYE LENGTH OR REFRACTION CAN RESULT IN REFRACTIVE ERRORS REFRACTIVE ERRORS TYPES STRABISMUS (Eye Deviation) May lead to Amblyopia Common test to detect the disorder • Corneal Light Reflex • Cover Test If uncorrected leads to blindness REFRACTIVE ERRORS TYPES MYOPIA A. ALSO REFERRED TO AS – NEARSIGHTNESS B. THE REFRACTIVE ABILITY OF THE EYE IS TOO STRONG FOR THE EYE LENGTH C. IMAGES ARE BENT & FALL IN FRONT OF, NOT ON, THE RETINA REFRACTIVE ERRORS TYPES HYPEROPIA A. ALSO REFERRED TO AS – FARSIGHTEDNESS B. THE REFRACTIVE ABILITY OF THE EYE IS TOO WEAK C. IMAGES ARE FOCUSED BEHIND THE RETINA D. A SHORTER LENGTH OF THE EYE MAY CONTRIBUTE TO THE DEVELOPMENT OF HYPEROPIA REFRACTIVE ERRORS TYPES PRESBYOPIA A. AS PEOPLE AGE THE CRYSTALLINE LENS LOSES ITS ELASTICITY & IS LESS ABLE TO ALTER ITS SHAPE TO FOCUS THE EYE FOR CLOSE WORK B. IMAGES FALL BEHIND THE RETINA C. PRESBYOPIA USUALLY OCCURS IN PEOPLE IN THEIR 30’s & 40’s REFRACTIVE ERRORS TYPES ASTIGMATISM A. OCCURS WHEN THE CURVE OF THE CORNEA IS UNEVEN B. BECAUSE LIGHT RAYS ARE NOT REFRACTED EQUALLY IN ALL DIRECTIONS A FOCUS POINT ON THE RETINA IS NOT ACHIEVED EYE DISORDERS BLINDNESS • LEGALLY DEFINED AS VISION < 20/200 W/ THE USE OF CORRECTIVE LENSES OR A VISUAL FIELD OF NO GREATER THAN 20 DEGREES. • GREATEST INCIDENCE AFTER AGE OF 65 • RISK FACTORS A. GLAUCOMA B. CATARACTS C. DIABETIC RETINOPATHY D. ATHEROSCLEROSIS E. TRAUMA EYE DISORDERS BLINDNESS ANALYSIS / NURSING DIAGNOSIS A. VISUAL SENSORY/PERCEPTUAL ALTERATION R/T BLINDNESS B. IMPAIRED SOCIAL INTERACTION R/T LOSS OF SIGHT C. RISK FOR INJURY R/T VISUAL IMPAIRMENT D. SELF-CARE DEFICIT R/T VISUAL LOSS EYE DISORDERS BLINDNESS NURSING CARE PLAN / IMPLEMENTATION A. GOAL: PROMOTE INDEPENDENCE & PROVIDE EMOTIONAL SUPPORT 1. FAMILIARIZE W/ SURROUNDINGS & ENCOURAGE USE OF TOUCH 2. ESTABLISH COMMUNICATION LINES & ANSWER QUESTIONS 3. DEAL W/ FEELINGS OF LOSS & OVERPROTECTIVENESS BY FAMILY MEMBERS EYE DISORDERS BLINDNESS 4. PROVIDE DIVERSIONAL ACTIVITIES, ie: A. RADIO B. TALKING BOOKS, TAPES, RECORDS 5. ENCOURAGE SELF-CARE ACTIVITIES 6. ALLOW VOICING OF FRUSTRATIONS WHEN ACTIVITY IS NOT DONE TO SATISFACTION – TO DECREASE ANGER & DISCOURAGEMENT EYE DISORDERS BLINDNESS NURSING CARE PLAN / IMPLEMENTATION B. GOAL: FACILITATE ACTIVITIES OF DAILY LIVING 1. EATING: A. ESTABLISH ROUTINE PLACEMENT FOR TABLEWARE, ie: PLATES B. HELP PERSON MENTALLY VISUALIZE THE PLATE AS A CLOCK / COMPASS C. TAKE PERSON’S HAND & GUIDE THE FINGERTIPS TO ESTABLISH SPATIAL RELATIONSHIP EYE DISORDERS BLINDNESS NURSING CARE PLAN / IMPLEMENTATION B. GOAL: FACILITATE ACTIVITIES OF DAILY LIVING 2. WALKING: A. HAVE PERSON HOLD YOUR FOREARM & WALK HALF A STEP IN FRONT B. TELL THE PERSON WHEN APPROACHING STAIRS, CURB, etc. EYE DISORDERS BLINDNESS NURSING CARE PLAN / IMPLEMENTATION B. GOAL: FACILITATE ACTIVITIES OF DAILY LIVING 3. TALKING: A. SPEAK WHEN APPROACHING PERSON & TELL THEM BEFORE YOU TOUCH THEM B. TELL THEM WHO YOU ARE & WHAT YOU WILL BE DOING C. DO NOT AVOID USING WORDS SUCH AS “SEE” / DISCUSSING THE APPEARANCE OF THINGS EYE DISORDERS BLINDNESS NURSING CARE PLAN / IMPLEMENTATION C. GOAL: HEALTH TEACHING 1. ACCIDENT PREVENTION IN THE HOME 2. COMMUNITY RESOURCES A. VOLUNTARY AGENCIES * American Foundation for the Blind * Nat’l. Society for the Prevention of Blindness B. GOVERNMENT AGENCIES * Social & Rehabilitative Service * Veteran’s Administration c. CARE OF ARTIFICIAL EYE CARING FOR AN ARTIFICAL EYE • W/ GLOVED HAND PULL LOWER EYELID DOWN OVER THE INFRAORBITAL BONE & EXERT PRESSURE BELOW THE EYELID • PRESSURE WILL MAKE THE EYE POP OUT • HANDLE EYE PROSTHESIS CAREFULLY • USING ASEPTIC TECHNIQUE, CLEANSE SOCKET W/ SALINE-MOISTENED GAUZE – STROKING FROM THE INNER TO OUTER CANTHUS • WASH THE PROSTHESIS IN WARM NORMAL SALINE • TO REINSERT – GENTLY PULL THE PATIENT’S LOWER LID DOWN, RAISE THE UPPER LID IF NECESSARY, SLIP THE SALINE-MOISTENED EYE PRSOSTHESIS GENTLY INTO THE SOCKET, & RELEASE THE LIDS EYE DISORDERS BLINDNESS EVALUATION / OUTCOME CRITERIA A. ACCEPTANCE OF DISABILITY * PARTICIPATES IN SELF-CARE ACTIVITIES * REMAINS SOCIALLY INVOLVED B. REGAINS INDEPENDENCE W/ REHABILITATION TRAUMA • • • • • Hematoma Chemical burns Corneal abrasions Penetrating/Non-penetrating wounds Foreign bodies EYE DISORDERS INFLAMMATION & INFECTIONS • BLEPHARITIS 1. AN INFLAMMATION OF THE EYELID EDGES 2. MOST COMMON IN THE OLDER ADULT 3. OFTEN ASSOCIATED W/ DRY EYE SYNDROME 4. LACK OF SUFFICIENT TEARS W/ THIS DX. MAY LEAD TO BACTERIAL INVASION OF THE EYE STRUCTURES, BECAUSE TEARS ARE BACTERIOSTATIC 5. SX.& SX. – ITCHY, RED & BURNING EYES W/ SEBORRHEA OF THE EYEBROWS & EYELIDS 6. TREATMENT – EYELID CARE OF WARM, MOIST COMPRESSES FOLLOWED BY GENTLE SCRUBBING W/ BABY SHAMPOO EYE DISORDERS INFLAMMATION & INFECTIONS • CHALAZION 1. 2. 3. 4. 5. 6. A STERILE INFLAMMATION OF A SEBACEOUS GLAND IN THE EYELID SX. & SX. - BEGINS W/ AN INFLAMMATION & TENDERNESS , FOLLOWED BY A GRADUAL PAINLESS SWELLING @ THE GLAND IN ITS FULLY DEVELOPED STATE NO SX. OF INFLAMMATION ARE PRESENT C/O EYE FATIGUE, SENSITIVITY TO LIGHT, POSSIBLEY EXCESSIVE TEARING TREATMENT – USE OF WARM COMPRESSES FOR 15’ QID, FOLLOWED BR INSTILLATION OF AN ANTI-INFECTIVE OPHTHALMIC OINTMENT M.D. MAY EXCISE CHALAZION IF IT INTERFERES W/ VISION EYE DISORDERS INFLAMMATION & INFECTIONS • CONJUNCTIVITIS 1. AN INFLAMMATION / INFECTION OF THE CONJUNCTIVA 2. INFLAMMATORY CONJUNCTIVAITIS RESULTS FROM EXPOSURE TO ALLERGENS / IRRITANTS & IS NOT CONTAGIOUS SX. & SX. – CONJUNCTIVAL EDEMA, BURNING SENSATION, EXCESSIVE TEARING , ITCHING & VASCULAR ENGORGEMENT W/ BLOODSHOT APPEARANCE OF EYE/S TREATMENT – INSTILLATION OF VASOCONSTRICTORS & CORTICOSTEROIDS EYEDROPS AS WELL AS INSTRUCTION FOR THE CLIENT TO AVOID USING EYE MAKE-UP UNTIL CONDITION SUBSIDES 4. 5. EYE DISORDERS INFLAMMATION & INFECTIONS CONJUNCTIVITIS -- CONT’D 1. 2. 3. 3. 4. 5. AN INFLAMMATION / INFECTION OF THE CONJUNCTIVA INFECTIOUS CONJUNCTIVITIS OCCURS AS A RESULT OF BACTERIAL / VIRAL INFECTION & IS CONTAGIOUS ALSO KNOWN AS BACTERIAL CONJUNCTIVITIS / “PINK EYE” SX. & SX. – BLOOD VESSEL DILATION, CONJUNCTIVAL EDEMA, TEARING & DISCHARGE DISCHARGE IS USUALLY WATERY @ FIRST THEN BECOMES THICKER, W/ SHREDS OF MUCUS TREATMENT – AIMED @ CONTOLLING THE INFECTION W/ C&S DONE OF DRAINAGE FOR APPROPRIATE ANTIINFECTIVE – HYGIENE INSTRUCTION GIVEN – ISOLATE LINENS & OTHER CLOTHING TO PREVENT SPREAD EYE DISORDERS INFLAMMATION & INFECTIONS HORDEOLUM 1. 2. 3. ALSO KNOWN AS A “STYE” THIS “STYE” CAN BE INTERNAL / EXTERNAL USUALLY AFFECTS ONLY ONE EYE @ A TIME W/ NO VISION IMPAIRMENT 3. EXTERNAL STYE IS AN INFECTION OF THE SWEAT GLANDS IN THE EYELID, OCCURING NEAR THE EMERGENCE OF THE EYELASHES FROM THE EYELID 5. INTERNAL STYE IS CAUSED BY AN INFECTION OF THE EYELID SEBACEOUS GLAND 4. SX. & SX. – A RED, SWOLLEN, TENDER AREA IS NOTED ON THE SKIN SURFACE SIDE OF THE EYELID & PAIN IS PRESENT R/T PURULENT DSCHG IN STYE 5. TREATMENT - WARM COMPRESSES – QID, & ANTIINFECTIVE OINTMENT EYE DISORDERS GLAUCOMA PATHOPHYSIOLOGY A. ACUTE (CLOSED ANGLE) IMPAIRED PASSAGE OF AQUEOUS HUMOR INTO THE CIRCULAR CANAL OF SCHLEMM DUE TO CLOSURE OF THE ANGLE BETWEEN THE CORNEA AND THE IRIS. ** MEDICAL EMERGENCY -- REQUIRES SURGERY EYE DISORDERS GLAUCOMA -- CONT’D B. PATHOPHYSIOLOGY CHRONIC (OPEN-ANGLE) LOCAL OBSTRUCTION OF AQUEOUS HUMOR BETWEEN THE ANTERIOR CHAMBER AND THE CANAL.. MOST COMMONLY TREATED WITH FOLLOWING MEDICATION : 1. MIOTICS 2. CARBONIC ANHYDRASE INHIBITORS EYE DISORDERS GLAUCOMA -- CONT’D C. PATHOPHYSIOLOGY GLAUCOMA (UNTREATED) IMBALANCE BETWEEN RATE OF SECRETION OF INTRAOCULAR FLUIDS AND RATE OF ABSORPTION OF AQUEOUS HUMOR > INCREASED INTRAOCULAR PRESSURE > DECREASED PERIPHERAL VISION > CORNEAL EDEMA > HALOS AND BLURRING VISION > BLINDNESS EYE DISORDERS GLAUCOMA -- CONT’D RISK FACTORS 5. 6. 7. 8. 9. *UNKNOWN, BUT ASSOCIATED WITH: 1. EMOTIONAL DISTURBANCES 2. HEREDITARY FACTORS 3. ALLERGIES / AGE 4. VASOMOTOR DISTURBANCES NEARSIGHTNESS (MYOPIA) EYE TRAUMA / SYSTEMIC CORTICOSTEROIDS CV DISEASE & DIABETES MIGRAINE SYNDROMES AFRICAN AMERICAN / ASIAN MALES EYE DISORDERS GLAUCOMA -- CONT’D ASSESSMENT A. SUBJECTIVE DATA ACUTE (CLOSED-ANGLE) 1. 2. 3. 4. 5. B. PAIN: SEVERE, IN & AROUND EYE HEADACHE RAINBOW HALOS AROUND LIGHTS BLURRING OF VISION N& V CHRONIC (OPEN-ANGLED) 1. EYES TIRE EASILY 2. LOSS OF PERIPHERAL VISION EYE DISORDERS GLAUCOMA -- CONT’D ASSESSMENT OBJECTIVE DATA 1. 2. 3. 4. 5. 6. CORNEAL EDEMA DECREASED PERIPHERAL VISION INCREASED CUPPING OF OPTIC DISC TONOMETRY - PRESSURES > 22mmHg PUPILS DILATED REDNESS OF EYE EYE DISORDERS GLAUCOMA -- CONT’D NURSING DIAGNOSES A. VISUAL SENSORY/ PERCEPTUAL ALTERATIONS R/T INCREASED INTRAOCULAR PRESSURE B. PAIN R/T SUDDEN INCREASE IN INTRAOCULAR PRESSURE C. RISK FOR INJURY R/T BLINDNESS D. IMPAIRED PHYSICAL MOBILITY R/T IMPAIRED VISION EYE DISORDERS GLAUCOMA -- CONT’D GOALS & IMPLEMENTATIONS 1. REDUCE IOP • ACTIVITY: BEDREST • POSITION: SEMI-FOWLER’S • MEDS AS ORDERED: A. MIOTICS B. CARBONIC ANHYDRASE INHIBITORS C. ANTICHOLINESTERASE D. OPHTHALMIC EYE DISORDERS GLAUCOMA MEDICATIONS 1. MIOTICS (PILOCARPINE & CARBACHOL) * USED TO LOWER THE IOP > INCREASED BLOOD FLOW TO THE RETINA & DECREASED RETINAL DAMAGE AND LOSS OF VISION * MIOTICS CAUSE A CONTRACTION OF THE CILIARY MUSCLE & WIDENING OF TRABECULAR MESHWORK * PILOCARPINE PRODUCES MIOSIS & DECREASES IOP EYE DISORDERS GLAUCOMA MEDICATIONS 2. CARBONIC ANHYDRASE INHIBITORS (acetazolamide) * INTERFERE WITH PRODUCTION OF CARBONIC ACID, WHICH LEADS TO DECREASED AQUEOUS HUMOR FORMATION & DECREASED IOP * USED FOR LONG-TERM TREATMENT OF OPEN-ANGLE GLAUCOMA * RECOMMENDED ONLY AFTER PILOCARPINE, BETA BLOCKERS, EPINEPHRINE, & CHOLINESTERASE INHIBITORS ARE INEFFECTIVE EYE DISORDERS GLAUCOMA MEDICATIONS 3. ANTICHOLINESTERATE * FACILITATES OUTFLOW OF AQUEOUS HUMOR SHORT-ACTING (PHYSOSTIGMINE SALICILATE) LONG-ACTING (DEMECARIUM BROMIDE ) EYE DISORDERS GLAUCOMA MEDICATIONS 4. OPHTHALMIC: BETA-ADRENERGIC BLOCKERS * (BETAXOLOL) BETOPTIC - USED TO DECREASE ELEVATED IOP IN CHRONIC OPENANGLE GLAUCOMA & OCULAR HYPERTENSION * (TIMOLOL MALEATE) TIMOPTIC - REDUCES PRODUCTION OF AQUEOUS HUMOR EYE DISORDERS GLAUCOMA -- CONT’D GOALS & IMPLEMENTATIONS 2. PROVIDE EMOTIONAL • PLACE PERSONAL OBJECTS SUPPORT WITHIN FIELD OF VISION • ASSIST WITH ACTIVITIES • ENCOURAGE VERBALIZATION OF CONCERNS, FEARS OF BLINDNESS, LOSS OF INDEPENDENCE EYE DISORDERS GLAUCOMA -- CONT’D GOALS & IMPLEMENTATIONS 4. HEALTH TEACHING A. PREVENT > IOP BY AVOIDING: 1. ANGER, EXCITEMENT, WORRY 2. CONSTRICTIVE CLOTHING 3. HEAVY LIFTING 4. EXCESSIVE FLUID INTAKE 5. STRAINING @ STOOL 6. EYE STRAIN 7. ATROPINE, OR OTHER MYDRIATICS WHICH CAUSE DILATION EYE DISORDERS GLAUCOMA -- CONT’D GOALS & IMPLEMENTATIONS 4. HEALTH B. TEACHING C. RELAXATION & STRESS MANAGEMENT TECHNIQUES PREPARE FOR SURGERY, IF ORDERED * LASER TRABECULOPLASTY * TRABECULECTOMY (FILTERING) D. ACTIVITY ALLOWED: * MODERATE EXERCISE - WALKING EYE DISORDERS GLAUCOMA -- CONT’D GOALS & IMPLEMENTATIONS 4. HEALTH E. SAFETY MEASURES: TEACHING 1. EYE PROTECTION - SHIELD/GLASSES 2. Medic Alert BAND/TAG 3. AVOID DRIVING 1-2 HR. AFTER INSTILLING MIOTICS F. MEDICATIONS: 1. PURPOSE, DOSAGE & FREQUENCY 3. EYEDROP INSTILLATION G. COMMUNITY RESOURCES, AS NEEDED EYE DISORDERS GLAUCOMA -- CONT’D EVALUATION/OUTCOME CRITERIA A. EYESIGHT PRESERVED, IF POSSIBLE B. IOP LOWERED ( < 22 mm Hg ) C. CONTINUES MEDICAL SUPERVISION FOR LIFE -REPORTS REAPPEARANCE OF SYMPTOMS IMMEDIATELY EYE DISORDERS -- CATARACTS PATHOPHYSIOLOGY/ETIOLOGY * * * * * DEVELOPMENT or DEGENERATIVE OPACIFICATION OF THE CRYSTALLINE LENS * CATARACTS CAN DEVELOP @ ANY AGE THEY MAY BE DUE TO A VARIETY OF CAUSES MOST COMMON IN LATER LIFE & ASSOCIATED WITH AGING CAN DEVELOP IN BOTH EYES -- USUALLY ONE EYE IS MORE COMPROMISED VISUAL IMPAIRMENT USUALLY PROGRESSES @ SAME RATE IN BOTH EYES EYE DISORDERS -- CATARACTS RISK FACTORS * * * * * AGING (MOST COMMON) * TRAUMA * TOXINS * CONGENITAL DEFECTS ASSOCIATED OCULAR CONDITIONS NUTRITIONAL FACTORS PHYSICAL FACTORS SYSTEMIC DISEASES & SYNDROMES EYE DISORDERS -- CATARACTS ASSESSMENT SUBJECTIVE DATA * VISION ( DIMMING ) * * * * * BLURRING ( PAINLESS ) LOSS OF ACUITY (SEE BEST IN LOW LIGHT) DISTORTION DIPLOPIA PHOTOPHOBIA * SENSITIVITY TO GLARE EYE DISORDERS -- CATARACTS ASSESSMENT OBJECTIVE DATA * BLINDNESS A. UNILATERAL B. BILATERAL ( PARTICULARLY, IN CONGENITAL CATARACTS) * LOSS OF RED REFLEX * GRAY OPACITY OF LENS * MYOPIC SHIFT & COLOR SHIFT * ASTIGMATISM * REDUCED LIGHT TRANSMISSION EYE DISORDERS -- CATARACTS ANALYSIS / NURSING DIAGNOSES A. VISUAL SENSORY/PERCEPTUAL ALTERATIONS R/T OPACITY OF LENS B. RISK FOR INJURY R/T ACCIDENTS C. SOCIAL ISOLATION R/T IMPAIRED VISION EYE DISORDERS -- CATARACTS CATARACT REMOVAL * REMOVAL OF OPACIFIED LENS BECAUSE OF LOSS OF VISION A. EXTRACAPSULAR CATARACT EXTRACTION ( ECCE ) FOLLOWED BY INTRAOCULAR LENS ( IOL ) INSERTION B. PHACOEMULSION - USES AN ULTRASONIC DEVICE THAT LIQUEFIES THE NUCLEUS & CORTEX WHICH ARE THEN SUCTIONED OUT THROUGH A TUBE EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS PREOPERATIVE CARE 1. PREPARE 1. ANTIBIOTIC DROPS/OINTMENT, AS FOR ORDERED SURGERY 2. MYDRIATIC EYEDROPS, AS ORDERED (NOTE DILATATION OF PUPILS) 3. AVOID GLARING LIGHTS 4. SURGERY OFTEN DONE UNDER LOCAL ANESTHESIA WITH SEDATION EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS PREOPERATIVE CARE 2. HEALTH TEACHING PRE-OP. 1. DO NOT RUB , TOUCH, or SQUEEZE EYES SHUT AFTER SURGERY 2. EYE PATCH WILL BE ON AFFECTED EYE 3. ASSISTANCE WILL BE GIVEN FOR NEEDS 4. OVERNIGHT HOSPITALIZATION NOT REQUIRED, UNLESS COMPLICATIONS OCCUR 5. MILD IRITITIS USUALLY OCCURS EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE 1. REDUCE STRESS ON THE SUTURES & PREVENT HEMORRHAGE A. 1. 2. B. 1. 2. ACTIVITY: AMBULATE , AS ORDERED, SOON AFTER SURGERY USUALLY DISCHARGED 5-6 HRS AFTER SURGERY POSITION: FLAT or LOW FOWLER’S LIE ON BACK or TURN TO UNOPERATIVE SIDE EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE C. AVOID ACTIVITIES THAT > IOP: 1. REDUCE 1. STRAINING @ STOOL STRESS ON 2. VOMITING, COUGHING, SHAVING THE SUTURES & PREVENT 3. BRUSHING TEETH or HAIR HEMORRHAGE 4. LIFTING OBJECTS > 20lb. 5. BENDING or STOOPING 6. WEAR GLASSES / SHADED LENS DURING DAY 7. WEAR EYESHIELD @ NIGHT EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE 1. REDUCE STRESS ON THE SUTURES & PREVENT HEMORRHAGE D. PROVIDE: 1. MOUTHWASH 2. HAIR CARE 3. PERSONAL ITEMS WITHIN EASY REACH 4. “STEP-IN” SLIPPERS EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE • FREQUENT CONTACTS TO 2. PROMOTE PREVENT SENSORY PSYCHOLOGICAL DEPRIVATION WELL-BEING • ESPECIALLY , THE ELDERLY EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE 3. HEALTH A. IF PRESCRIPTIVE GLASSES ARE USED, TEACHING EXPLAIN ABOUT: 1. MAGNIFICATION POST-OP. 2. 3. 4. 5. PERCEPTUAL DISTORTION BLIND AREAS IN PERIPHERAL VISION GUIDE THRU ACTIVITIES WITH GLASSES NEED TO LOOK THRU CENTRAL PORTION OF LENS 6. TURNING HEAD TO SIDE WHEN LOOKING TO THE SIDE TO PREVENT DISTORTION EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE 3. HEALTH B. EYE CARE: TEACHING 1. EYE SHIELD @ NIGHT x 1 MONTH POST-OP. 2. EYE CARE - NO IOL INSERTION * INSTILLATION OF MYDRIATIC & CARBONIC ANHDRASE INHIBITORS TO PREVENT GLAUCOMA & ADHESIONS 3. EYE CARE - WITH IOL INSERTION * STEROID- ANTIBIOTIC USED EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE 3. HEALTH C. SIGNS & SYMPTOMS of: TEACHING 1. INFECTION POST-OP. 2. IRIS PROLAPSE * BULGING / PEAR SHAPED PUPIL 3. HEMORRHAGE * SHARP PAIN * HALF MOON OF BLOOD EYE DISORDERS -- CATARACTS GOALS & IMPLEMENTATIONS POSTOPERATIVE CARE 3. HEALTH D. AVOID: TEACHING 1. HEAVY LIFTING POST-OP. 2. POTENTIAL EYE TRAUMA EYE DISORDERS -- CATARACTS EVALUATION/OUTCOME CRITERIA 1. 2. 3. 4. 5. VISION RESTORED NO COMPLICATIONS - ( ie. Severe eye pain or Hemorrhage ) PERFORMS SELF-CARE ACTIVITIES - ( ie. Instills own eyedrops ) RETURNS FOR FOLLOW-UP OPHTHALMOLOGY CARE RECOGNIZES SYMPTOMS REQUIRING IMMEDIATE ATTENTION EYE DISORDERS RETINAL DETACHMENT DESCRIPTION • A RETINAL HOLE IS A BREAK IN THE INTEGRITY OF THE PERIPHERAL SENSORY RETINA & CAN BE CAUSED BY TRAUMA / CAN OCCUR W/ AGING • A RETINAL TEAR IS A MORE JAGGED & IRREGULARLY SHAPED BREAK IN THE RETINA – WHICH CAN RESULT FROM TRACTION ON THE RETINA • A RETINAL DETACHMENT IS THE SEPARATION OF THE SENSORY RETINA FROM THE PIGMENTED EPITHELIUM – A SEPARATION OF RETINA FROM CHOROID EYE DISORDERS RETINAL DETACHMENT RISK FACTORS A. TRAUMA B. DEGENERATION ASSESSMENT -- SUBJECTIVE DATA A. FLASHES OF LIGHT BEFORE EYES B. VISION IS: 1. BLURRED 2. SOOTY (SUDDEN ONSET) 3. SENSATION OF FLOATING PARTICLES 4. BLANK AREAS OF VISION EYE DISORDERS RETINAL DETACHMENT ASSESSMENT – OBJECTIVE DATA A. OPHTHALMIC EXAM REVEALS: 1. RETINA IS GRAYISH IN AREA OF TEAR 2.BRIGHT, RED HORSESHOE-TYPE TEAR EYE DISORDERS RETINAL DETACHMENT ANALYSIS / NURSING DIAGNOSIS A. VISUAL SENSORY/PERCEPTUAL ALTERATION R/T BLURRED VISION B. ANXIETY R/T POTENTIAL LOSS OF VISION C. RISK FOR INJURY R/T BLINDNESS EYE DISORDERS RETINAL DETACHMENT A. NURSING CARE PLAN / IMPLEMENTATION PREOPERATIVE CARE 1. GOAL: REDUCE ANXIETY & PREVENT FURTHER DETACHMENT A. ENCOURAGE VERBALIZATION OF FEELINGS, ANSWER ALL QUESTIONS, & REINFORCE PHYSICIAN’S EXPLANATION OF SURGICAL PROCEDURE B. ACTIVITY: 1. BEDREST 2. EYES USUALLY COVERED TO PROMOTE EYE RELAXATION 3. SIDERAILS UP EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION A. PREOPERATIVE CARE 1. GOAL: REDUCE ANXIETY & PREVENT FURTHER DETACHMENT C. POSITION: 1. ACCORDING TO LOCATION OF RETINAL TEAR 2. INVOLVED AREA OF EYE SHOULD BE IN DEPENDENT POSITION EYE DISORDERS RETINAL DETACHMENT A. NURSING CARE PLAN / IMPLEMENTATION PREOPERATIVE CARE 1. GOAL: REDUCE ANXIETY & PREVENT FURTHER DETACHMENT D. MEDICATIONS: 1. ADMINSTER AS ORDERED 2. CYCLOPLEGIC / MYDRIATICS – TO DILATE THE PUPIL WIDELY & DECREASE INTRAOCULAR MOVEMENT E. RELAXING DIVERSION: 1. CONVERSATION 2. MUSIC EYE DISORDERS RETINAL DETACHMENT A. NURSING CARE PLAN / IMPLEMENTATION PREOPERATIVE CARE 2. GOAL: HEALTH TEACHING A. PREPARE FOR SURGICAL INTERVENTION 1. CRYOTHERAPY - SUPER-COOLED PROBE IS APPLIED TO THE SCLERA, CAUSING A SCAR, WHICH PULLS THE CHOROID & RETINA TOGETHER 2. LASER PHOTOCOAGULATION – A BEAM OF INTENSE LIGHT FROM A CARBON ARC IS DIRECTED THROUGH THE DILATED PUPIL ONTO THE RETINA & SEALS HOLE IF RETINA NOT DETACHED EYE DISORDERS RETINAL DETACHMENT A. NURSING CARE PLAN / IMPLEMENTATION PREOPERATIVE CARE 2. GOAL: HEALTH TEACHING A. PREPARE FOR SURGICAL INTERVENTION 3. SCLERAL BUCKLING – THE SCLERA IS RESECTED / SHORTENED TO ENHANCE THE CONTACT BETWEEN THE CHOROID & RETINA 4. BANDING / ENCIRCLEMENT – SILICANE BAND / STRAP IS PLACED UNDER THE EXTRAOCULAR MUSCLES AROUND THE GLOBE EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 1. GOAL: REDUCE INTRAOCULAR STRESS & PREVENT HEMORRHAGE A. POSITION: 1. FLAT / LOW FOWLER’S 2. SANDBAGS MAY BE USED TO POSITION HEAD 3. TURN TO NON-OPERATIVE SIDE, IF ALLOWED W/ RETINAL TEAR DEPENDENT 4. SPECIAL POSITIONS MAY BE: PRONE SIDE-LYING SITTING W/ FACE DOWN ON TABLE EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 1. GOAL: REDUCE INTRAOCULAR STRESS & PREVENT HEMORRHAGE B. ACTIVITY: 1. BEDREST 2. DECREASE INTRAOCULAR PRESSURE BY NOT: A. STOOPING B. BENDING C. ASSUMING PRONE POSITION EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 1. GOAL: REDUCE INTRAOCULAR STRESS & PREVENT HEMORRHAGE C. MEDICATIONS: 1. MYDRIATICS – REDUCE EYE MOVEMENT 2. ANTI-INFECTIVES – PREVENT INFECTION 3. CORTICOSTEROIDS - INFLAMMATION EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 1. GOAL: REDUCE INTRAOCULAR STRESS & PREVENT HEMORRHAGE D. RANGE OF MOTION EXERCISES: 1. ISOMETRIC 2. PASSIVE 3. ELASTIC STOCKINGS TO PREVENT THROMBUS R/T IMMOBILITY EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 2. GOAL: SUPPORT COPING MECHANISMS A. PLAN ALL CARE W/ PATIENT B. ENCOURAGE VERBALIZATION OF FEELINGS, FEARS C. ENCOURAGE FAMILY INTERACTION D. DIVERSIONAL ACTIVITIES EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 3. GOAL: HEALTH TEACHING A. EYE CARE: 1. EYE PATCH / SHIELD @ NIGHT 2. DARK GLASSES 3. AVOID RUBBING / SQUEEZING EYES B. MEDICATIONS: 1. DRUG TEACHING 2. AVOID OTC MEDICATION EYE DISORDERS RETINAL DETACHMENT NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 3. GOAL: HEALTH TEACHING C. LIMITATIONS: 1. NO READING FOR 3 WEEKS 2. NO PHYSICAL EXERTION FOR 6 WEEKS D. SIGNS OF REDETACHMENT: 1. FLASHES OF LIGHT 2. INCREASE IN “FLOATERS” 3. BLURRED VISION EYE DISORDERS RETINAL DETACHMENT EVALUATION / OUTCOME CRITERIA A. VISION RESTORED B. NO FURTHER “DETACHMENT “ – RECOGNIZES SIGNS & SYMPTOMS C. NO INJURY OCCURS D. ACCEPTS LIMITATIONS EYE DISORDERS RETINITIS PIGMENTOSA • A CHRONIC PROGRESSIVE DISEASE • ONSET IN EARLY CHILDHOOD • PATHOLOGY 1. DEGENERATION OF THE RETINAL EPITHELIUM – ESPECIALLY THE RODS – W/OUT INFLAMMATION 2. ATROPHY OF THE OPTIC NERVE 3. WIDESPREAD PIGMENTARY CHG. IN RETINA EYE DISORDERS RETINITIS PIGMENTOSA • CAUSE OF THE DISEASE IS UNKNOWN • HEREDITARY TENDENCY IS SUSPECTED • SX. & SX. 1. DEFECTIVE NIGHT VISION – EARLY SX. 2. CONSTRICTED FIELD OF VISION – LATER SX. • TREATMENT 1. NO SPECIFIC THERAPY – GENETIC COUNSELING 2. FAMILY VISION CHECKS FOR SAME PROBLEM MACULAR DEGENERATION Two Types • Dry (Atrophic) • Wet (Exudative) • • • • Clinical Manifestations Diagnostic Studies Treatments Nursing Care CANCERS •Retinoblastoma - Definition - Etiology/Incidence - Clinical Manefestations - Diagnostic Tests - Teatments TYPES OF OPHTHALMIC DRUGS F. TOPICAL ANESTHETIC ACTION -- 1. DECREASES SENSATION (PAIN) USES -- 1. SURGERY, TREATMENTS 2. EYE INFLAMMATIONS G. TOPICAL ANTIBIOTIC ACTION -- 1. ANTI- INFECTIVE USES -- 1. EYE INFLAMMATIONS H. STEROID ACTION -- 1. EYE INFLAMMATIONS USES -- 1. EYE INFLAMMATIONS & ALLERGIC REACTIONS TYPES OF OPHTHALMIC DRUGS I. CARBONIC ANHYDRASE INHIBITORS ACTION-- 1. REDUCES PRODUCTION OF AQUEOUS HUMOR USES -- 1. GLAUCOMA J. BETA-ADRENERGIC BLOCKERS ACTION -- 1. REDUCES FORMATION OF AQUEOUS HUMOR W/OUT PRODUCING MIOSIS / HYPEREMIA USES -- 1. CHRONIC GLAUCOMA 2. OCULAR HYPERTENSION TYPES OF OPHTHALMIC DRUGS A. MYDRIATICS ACTION-- 1. DILATES PUPIL USES -- 1. EXAMINATION OF INTERIOR OF EYE 2. PREVENTS ADHESIONS OF IRIS W/ CORNEA IN EYE INFLAMMATIONS TYPES OF OPHTHALMIC DRUGS B. CYCOPLEGIC ACTION-- 1. DILATES PUPIL 2. PARALYZES CILIARY MUSCLE & IRIS USES -- 1. DECREASES PAIN & PHOTOPHOBIA 2. PROVIDES REST IN: A. INFLAMMATIONS OF IRIS & CILIARY BODY B. DISEASES OF CORNEA TYPES OF OPHTHALMIC DRUGS C. MIOTICS ACTION-- 1. CONTRACTS PUPIL 2. PERMITS BETTER DRAINAGE OF INTRAOCULAR FLUID USES -- 1. GLAUCOMA TYPES OF OPHTHALMIC DRUGS D. OSMOTIC ACTION-- 1. DECREASES IOP USES -- 1. ACUTE GLAUCOMA 2. EYE SURGERY E. SECRETORY INHIBITOR ACTION-- 1. DECREASES PRODUCTION OF INTRAOCULAR FLUID USES -- 1. GLAUCOMA EAR ALTERATIONS SX. OF HEARING LOSS • FREQUENTLY ASKING PEOPLE TO REPEAT STATEMENTS • STRAINING TO HEAR • TURNING HEAD/LEANING FORWARD TO FAVOR ONE EAR • SHOUTING IN CONVERSATION • RINGING IN THE EARS • FAILING TO RESPOND WHEN NOT LOOKING IN THE DIRECTION OF THE SOUND SX. OF HEARING LOSS (CONT’D) • IRRITABILITY • ANSWERING QUESTIONS INCORRECTLY • RAISING THE VOLUME OF THE TELEVISION / RADIO • AVOIDING LARGE GROUPS • BETTER UNDERSTANDING OF SPEECH WHEN IN SMALL GROUPS • WITHDRAWING FROM SOCIAL INTERACTIONS PERMISSIVE NOISE EXPOSURES DURATION/DAY (HR) 8 6 4 3 2 1½ 1 ½ ¼ SOUND LEVEL (dbA,slow) 90 92 95 97 100 102 105 110 115 INTENSITY RANGE OF HUMAN HEARING & INTENSITY LEVEL OF VARIOUS ENVIRON. SOUNDS DECIBELS 140 DECIBELS 60 Jet Engine 130 Conversation 50 Average Office 120 40 Thunder 110 30 Avg. Residence 100 Rivet Hammer 90 20 10 Low Whisper 0 Threshold of Hearing Air Hammer 80 Heavy Traffic 70 AUDITORY ASSESSMENT • WHEN EVALUATING HEARING, THREE CHRX. ARE IMPORTANT: A. FREQUENCY B. PITCH C. INTENSITY AUDITORY ASSESSMENT FREQUENCY • FREQUENCY REFERS TO THE NUMBER OF SOUND WAVES EMANATING FROM A SOURCE PER SECOND – CYCLES PER SECOND OR HERTZ (Hz) • THE NORMAL HUMAN EAR PERCEIVES SOUNDS RANGING IN FREQUENCY FROM 20 – 20,000 Hz • THE FREQUENCIES FROM 500 – 2,000 Hz ARE IMPORTANT IN UNDERSTANDING EVERYDAY SPEECH & ARE REFERRED TO AS THE SPEECH RANGE OR SPEECH FREQUENCIES AUDITORY ASSESSMENT PITCH • PITCH IS THE TERM USED TO DESCRIBE FREQUENCY • A TONE WITH 100 Hz IS CONSIDERED OF LOW PITCH • A TONE OF 10,000 Hz IS CONSIDERED OF HIGH PITCH AUDITORY ASSESSMENT LOUDNESS • THE UNIT FOR MEASURING LOUDNESS (INTENSITY OF SOUND) IS THE DECIBEL (dB), THE PRESSURE EXERTED BY SOUND • HEARING LOSS IS MEASURED IN DECIBELS, A LOGARITHMIC FUNCTION OF INTENSITY THAT IS NOT EASILY CONVERTED INTO %. • THE CRITICAL LEVEL OF LOUDNESS IS APPRX. 30 Db • SOUNDS LOUDER THAN 80 dB IS PERCEIVED BY THE HUMAN EAR TO BE TOO HARSH & CAN BE DAMAGING TO THE INNER EAR. AUDITORY ASSESSMENT LOUDNESS • EXAMPLES OF LOUDNESS IN EVERYDAY LIFE * 15 dB – SHUFFLING OF PAPER IN QUIET SURROUNDINGS * 40 dB -- LOW CONVERSATION * 150 dB -- JET PLANE 100 ft AWAY AUDITORY ASSESSMENT GOAL OF TREATMENT • WITH SURGICAL TREATMENT OF PATIENTS WITH HEARING LOSS, THE AIM IS TO IMPROVE THE HEARING LEVEL TO 30 dB OR BETTER WITHIN THE SPEECH FREQUENCIES AUDITORY ASSESSMENT SEVERITY OF HEARING LOSS LOSS IN DECIBELS • 0 - 15 • • • • • • >15 - 25 >25 – 40 >40 – 55 >55 – 70 > 70 – 90 > 90 INTERPRETATION NORMAL HEARING SLIGHT HEARING LOSS MILD HEARING LOSS MODERATE HEARING LOSS MODERATE TO SEVERE LOSS SEVERE HEARING LOSS PROFOUND HEARING LOSS AUDITORY ASSESSMENT AUDIOMETRY TEST • WITH AUDIOMETRY, THE AUDIOLOGIST PERFORMS THE TESTING WHILE THE PATIENT WEARS EARPHONES & SIGNALS WHEN HEARING A TONE – DONE IN SOUNDPROOF ROOM • WHEN THE TONE IS APPLIED DIRECTLY OVER THE EXTERNAL AUDITORY CANAL, AIR CONDUCTION IS MEASURED • WHEN THE STIMULUS IS APPLIED TO THE MASTOID BONE , BYPASSING THE CONDUCTIVE MECHANISM (OSSICLES) NERVE CONDUCTION IS TESTED • AUDIOMETRY GRAPH PLOTS TYPE OF CONDUCTION AUDITORY ASSESSMENT TYMPANOGRAM TEST • A TYMPANOGRAM , OR IMPEDANCE AUDIOMETRY, MEASURES MIDDLE EAR MUSCLE REFLEX TO SOUND STIMULATION, & COMPLIANCE OF THE TYMPANIC MEMBRANE. • IT DOES THIS BY CHANGING THE AIR PRESSURE IN A SEALED EAR CANAL. • COMPLIANCE IS IMPAIRED W/ MIDDLE EAR DISEASE HEARING LOSS STATISTICS • MORE THAN 28 MILLION PEOPLE IN THE USA HAVE SOME TYPE OF HEARING IMPAIRMENT • MOST CAN BE HELPED W/ MEDICAL OR SURGICAL THERAPIES OR W/ A HEARING AID • BY THE YEAR 2050, ABOUT ONE (1) OUT OF EVERY FIVE (5) PEOPLE IN THE USA, OR ALMOST 58 MILLION PEOPLE, WILL BE AGE 55 OR > • OF THIS POPULATION ALMOST ONE-HALF CAN EXPECT A HEARING IMPAIRMENT CONDUCTIVE HEARING LOSS DESCRIPTION 1. WHEN SOUND WAVES ARE BLOCKED TO THE INNER EAR FIBERS BECAUSE OF EXTERNAL EAR OR MIDDLE EAR DISORDERS 2. DISORDERS CAN OFTEN BE CORRECTED W/ NO DAMAGE TO HEARING, OR MINIMAL PERMANENT HEARING LOSS CONDUCTIVE HEARING LOSS CAUSES 1. ANY INFLAMMATORY PROCESS OR OBSTRUCTION OF THE EXTERNAL OR MIDDLE EAR 2. TUMORS 3. OTOSCLEROSIS 4. A BUILD-UP OF SCAR TISSUE ON THE OSSICLES FROM PREVIOUS MIDDLE EAR SURGERY SENSORINEURAL HEARING LOSS DESCRIPTION 1. A PATHOLOGICAL PROCESS OF THE INNER EAR OR OF THE SENSORY FIBERS THAT LEAD TO THE CEREBRAL CORTEX 2. IS OFTEN PERMANENT & MEASURES MUST BE TAKEN TO REDUCE FURTHER DAMAGE OR TO ATTEMPT TO AMPLIFY SOUND AS A MEANS OF IMPROVING HEARING TO SOME DEGREE SENSORINEURAL HEARING LOSS CAUSES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. DAMAGE TO THE INNER EAR DAMAGE TO CRANIAL NERVE VIII (8) PROLONGED EXPOSURE TO LOUD NOISE MEDICATIONS TRAUMA INHERITED DISORDERS METABOLIC & CIRCULATORY DISORDERS INFECTIONS SURGERY MENIERE’S SYNDROME DIABETES MELLITIS MYXEDEMA MIXED HEARING LOSS • ALSO KNOWN AS CONDUCTIVE-SENSORINEURAL HEARING LOSS • CLIENT HAS BOTH SENSORINEURAL & CONDUCTIVE HEARING LOSS FACILITATING COMMUNICATION • USING WRITTEN WORDS IF THE CLIENT IS ABLE TO SEE, READ, & WRITE • PROVIDING PLENTY OF LIGHT IN THE ROOM • FACING THE CLIENT WHEN SPEAKING • TALKING IN A ROOM WITHOUT DISTRACTING NOISES • MOVING CLOSE TO THE CLIENT & SPEAKING SLOWLY & CLEARLY • GETTING THE ATTENTION OF THE CLIENT BEFORE YOU BEGIN TO SPEAK FACILITATING COMMUNICATION • KEEPING HANDS & OTHER OBJECTS AWAY FROM THE MOUTH WHEN TALKING TO THE CLIENT • TALKING IN LOWER TONES BECAUSE SHOUTING IS NOT HELPFUL • REPHRASING SENTENCES & REPEATING INFORMATION • VALIDATING W/ THE CLIENT THE UNDERSTANDING OF STATEMENTS MADE, BY ASKING THE CLIENT TO REPEAT WHAT WAS SAID • READING LIPS • ENCOURAGING THE CLIENT TO WEAR GLASSES WHEN TALKING TO SOMEONE TO IMPROVE VISION FOR LIP READING FACILITATING COMMUNICATION • USING SIGN LANGUAGE, WHICH COMBINES SPEECH WITH HAND MOVEMENTS THAT SIGNIFY LETTERS, WORDS, OR PHRASES • USING TELEPHONE AMPLIFIERS • INSTALLING FLASHING LIGHTS THAT ARE ACTIVATED BY RINGING OF THE TELEPHONE OR DOORBELL • USING SPECIALLY TRAINED DOGS THAT HELP THE CLIENT TO BE AWARE OF SOUND & TO ALERT THE CLIENT OF POTENTIAL DANGERS COCHLEAR IMPLANTATION • USED FOR SENSORINEURAL HEARING LOSS • A SMALL COMPUTER CONVERTS SOUND WAVES INTO ELECTRICAL IMPULSES • ELECTRODES ARE PLACED BY THE INTERNAL EAR W/ A COMPUTER DEVICE ATTACHED TO THE EXTERNAL EAR • ELECTRONIC IMPULSES DIRECTLY STIMULATE NERVE FIBERS HEARING AIDS • USED FOR THE CLIENT W/ CONDUCTIVE HEARING LOSS • CAN HELP THE CLIENT W/ SENSORINEURAL HEARING LOSS, ALTHOUGH NOT AS EFFECTIVE • A DIFFICULTY THAT EXISTS IS THE AMPLIFICATION OF BACKGROUND NOISE AS WELL AS VOICES • CLIENT EDUCATION EAR PROCEDURES IRRIGATION A. WARM TAP WATER TO BODY TEMPERATURE B. FILL A SYRINGE W/ WARM WATER C. PLACE A BASIN UNDER THE EAR TO BE IRRIGATED AS WELL AS A TOWEL AROUND THE CLIENT’S NECK TO AVOID GETTING THE CLIENT WET D. USE AN OTOSCOPE TO CHECK THE LOCATION OF THE IMPACTED CERUMEN E. PLACE THE TIP OF THE SYRINGE AT AN ANGLE SO THAT THE FLUID PUSHES AT ONE SIDE OF THE IMPACTION & NOT DIRECTLY ON THE IMPACTION – THIS HELPS TO LOOSEN THE CERUMEN & AVOIDS PUSHING IT BACK IN THE CANAL EAR PROCEDURES IRRIGATION cont’d F. WATCH FLUID RETURN FOR SIGNS OF CERUMEN PLUG REMOVAL G. CONTINUE TO IRRIGATE THE EAR W/ APPROXIMATELY 50 –70 ml. OF FLUID H. IF THE CERUMEN DOES NOT DRAIN OUT, WAIT ABOUT 10 MINUTES, THEN REPEAT THE PROCEDURE EAR PROCEDURES IRRIGATION cont’d I. MONITOR FOR SIGNS OF NAUSEA – IF IT DEVELOPS – STOP THE PROCEDURE J. IF CERUMEN CANNOT BE REMOVED BY IRRIGATION, GLYCERIN DROPS AS PRESCRIBED MAY BE USED 3 X A DAY FOR 2 DAYS & THEN IRRIGATION IS REPEATED EAR PROCEDURES A. TILT THE CLIENT’S HEAD IN THE OPPOSITE DIRECTION OF THE AFFECTED EAR & PLACE DROPS IN THE EAR B. INSERT A COTTON BALL INTO THE EAR CANAL TO ACT AS PACKING PRESBYCUSIS DESCRIPTION 1. ASSOCIATED W/ AGING 2. LEADS TO DEGENERATION / ATROPHY OF THE GANGLION CELLS IN THE COCHLEA & A LOSS OF ELASTICITY OF THE BASILAR MEMBRANES 3. LEADS TO COMPROMISE OF THE VASCULAR SUPPLY TO THE INNER EAR W/ CHANGES IN SEVERAL AREAS OF THE EAR STRUCTURE PRESBYCUSIS ASSESSMENT 1. HEARING LOSS IS GRADUAL & BILATERAL 2. CLIENTS STATE THEY HAVE NO PROBLEM W/ HEARING, BUT THEY CANNOT UNDERSTAND WHAT THE WORDS ARE 3. CLIENTS THINK THAT THE SPEAKER IS MUMBLING DEAFNESS • HARD OF HEARING – SLIGHT OR MODERATE HEARING LOSS THAT IS SERVICEABLE FOR PERFORMING ACTIVITIES OF DAILY LIVING • DEAF – HEARING IS NONFUNCTIONAL FOR CARRYING OUT ACTIVITIES OF DAILY LIVING DEAFNESS RISK FACTORS • CONDUCTIVE HEARING LOSSES -( TRANSMISSION DEAFNESS ) 1. IMPACTED CERUMEN (WAX) 2. FOREIGN BODY IN EXTERNAL AUDITORY CANAL 3. DEFECTS – THICKENING, SCARRING – OF EARDRUM 4. OTOSCLEROSIS OF OSSICLES DEAFNESS RISK FACTORS • SENSORINEURAL HEARING LOSSES – ( PERCEPTIVE OR NERVE DEAFNESS ) 1. ARTERIOSCLEROSIS 2. INFECTIOUS DISEASES MUMPS – MEASLES – MENINGITIS 3. DRUG TOXICITIES QUININE – STREPTOMYCIN – NEOMYCIN 4. TUMORS 5. HEAD TRAUMA 6. HIGH-INTENSITY NOISES DEAFNESS – ASSESSMENT OBJECTIVE DATA • INATTENTIVE OR STRAINED FACIAL EXPRESSIONS • EXCESSIVE LOUDNESS OR SOFTNESS OF SPEECH • FREQUENT NEED TO CLARIFY CONTENT OF CONVERSATION OR INAPPROPRIATE RESPONSES • TILTING OF HEAD WHILE LISTENING • LACK OF RESPONSE WHEN OTHERS SPEAK DEAFNESS - ANALYSIS/ NSG.DX. • AUDITORY SENSORY/PERCEPTUAL ALTERATION R/T LOSS OF HEARING • IMPAIRED SOCIAL INTERACTION R/T DEAFNESS DEAFNESS – NURSING CARE / IMPLEMENTATION • GOAL: MAXIMIZE HEARING ABILITY & PROVIDE EMOTIONAL SUPPORT 1. GAIN PERSON’S ATTENTION BEFORE SPEAKING – AVOID STARTLING 2. PROVIDE ADEQUATE LIGHTING SO PERSON CAN SEE YOU WHEN YOU ARE SPEAKING 3. LOOK AT THE PERSON WHEN SPEAKING 4. USE NONVERBAL CUES TO ENHANCE COMMUNICATION, ie: * WRITING – HAND GESTURES - POINTING DEAFNESS – NURSING CARE / IMPLEMENTATION 4. SPEAK SLOWLY, DISTINCTLY; DO NOT SHOUT ( EXCESSIVE LOUDNESS DISTORTS VOICE ) 5. IF PERSON DOES NOT UNDERSTAND, USE DIFFERENT WORDS: WRITE IT DOWN 6. SUPPORTIVE, NONSTRESSFUL ENVIRONMENT 7. USE ALTERNATIVE COMMUNICATION SYSTEM: A. SPEECH (LIP) READING B. SIGN LANGUAGE C. HEARING AID D. PAPER & PENCIL E. FLASH CARDS DEAFNESS – NURSING CARE / IMPLEMENTATION • GOAL: HEALTH TEACHING 1. PREPARE FOR EVALUATIVE STUDIES ( AUDIOGRAM ) 2. APPROPRIATE COMMUNITY RESOURCES, ie: * NAT. ASSOC. FOR DEAF 3. USE OF HEARING AID, ie: * CARE OF -- TESTING – SPARE BATTERIES 4. SAFETY PRECAUTIONS, ie: * WHEN CROSSING STREETS -- DRIVING DEAFNESS – EVALUATION / OUTCOME CRITERIA • METHOD OF COMMUNICATION ESTABLISHED • ACHIEVES INDEPENDENCE, ie: 1. DOGS FOR DEAF 2. SPECIAL TELEPHONES 3. VISUAL SIGNALS • COPES W/ LIFE-STYLE CHANGES, ie: 1. MINIMAL DEPRESSION 2. ANGER 3. HOSTILITY EAR DISORDERS OTOSCLEROSIS DESCRIPTION A. INSIDIOUS, PROGRESSIVE DEAFNESS B. MOST COMMON CAUSE OF CONDUCTIVE DEAFNESS C. CAUSE UNKNOWN D. DISEASE OF THE LABYRINTHE CAPSULE OF THE MIDDLE EAR THAT RESULTS IN A BONY OVERGROWTH OF TIESSUE SURROUNDING THE OSSICLES EAR DISORDERS OTOSCLEROSIS DESCRIPTION E. CAUSES THE DEVELOPMENT OF IRREGULAR AREAS OF NEW BONE FORMATION & CAUSES THE FIXATION OF THE BONES F. STAPES FIXATION LEADS TO A CONDUCTIVE HEARING LOSS G. IF THE DISEASE INVOLVES THE INNER EAR, SENSORINEURAL HEARING LOSS IS PRESENT H. IT IS NOT UNCOMMON TO HAVE BILATERAL INVOLVEMENT, ALTHOUGH HEARING LOSS MAY BE WORSE IN ONE EAR I. A PARTIAL STAPEDECTOMY W/ PROSTHESIS – FENESTRATION – MAY BE FORMED EAR DISORDERS OTOSCLEROSIS PATHOPHYSIOLOGY • FORMATION OF NEW SPONGY BONE IN LABYRINTH > B. FIXATION OF STAPES > C. PREVENTION OF SOUND TRANSMISSION THRU OSSICLES TO INNER EAR FLUIDS EAR DISORDERS OTOSCLEROSIS RISK FACTORS A. HEREDITY B. FEMALES C. PUBERTY TO 45 yrs OLD EAR DISORDERS OTOSCLEROSIS ASSESSMENT – SUBJECTIVE DATA A. TINNITUS – CONSTANT RINGING / ROARING B. DIFFICULTY HEARING – GRADUAL LOSS IN BOTH EARS C. SLOWLY PROGRESSIVE CONDUCTIVE HEARING LOSS EAR DISORDERS OTOSCLEROSIS ASSESSMENT – OBJECTIVE DATA A. RINNE TEST 1. TUNING FORK PLACED OVER MASTOID BONE 2. REDUCED SOUND CONDUCTION BY AIR & INTENSIFIED BY BY BONE 3. NEGATIVE RINNE TEST W/ OTOSCLEROSIS EAR DISORDERS OTOSCLEROSIS ASSESSMENT – OBJECTIVE DATA B. WEBER TEST 1. TUNING FORK PLACED ON TOP OF HEAD 2. INCREASED SOUND CONDUCTION TO AFFECTED EAR 3. LATERALIZATION OF SOUND TO THE EAR W/ THE MOST CONDUCTIVE HEARING LOSS EAR DISORDERS OTOSCLEROSIS ASSESSMENT – OBJECTIVE DATA C. AUDIOMETRY 1. DIMINISHED HEARING D. PINKISH DISCOLORATION – SCHWARTZE’S SX. – OF THE TYMPANIC MEMBRANE, WHICH INDICATES VASCULAR CHANGES W/IN THE EAR EAR DISORDERS OTOSCLEROSIS ANALYSIS / NURSING DIAGNOSIS A. AUDITORY SENSORY/PERCEPTUAL ALTERATION R/T HEARING LOSS B. BODY IMAGE DISTURBANCE R/T HEARING AID C. INEFFECTIVE INDIVIDUAL COPING R/T GRIEF REACTION TO LOSS D. IMPAIRED SOCIAL INTERACTION R/T HEARING LOSS EAR DISORDERS OTOSCLEROSIS NURSING CARE PLAN / IMPLEMENTATION & EVALUATION / OUTCOME CRITERIA SAME AS STAPEDECTOMY CARE PLAN EAR DISORDERS LABYRINTHITIS DESCRIPTION A. INFECTION OF THE LABYRINTH THAT OCCURS AS A COMPLICATION OF ACUTE / CHRONIC OTITIS MEDIA ASSESSMENT A. HEARING LOSS THAT MAY BE PERMANENT ON THE AFFECTED SIDE B. TINNITUS C. SPONTANEOUS NYSTAGMUS TO THE AFFECTED SIDE D. VERTIGO E. NAUSEA & VOMITING EAR DISORDERS LABYRINTHITIS IMPLEMENTATION A. MONITOR FOR SX. OF MENINGITIS – MOST COMMON COMPLICATION – AEB. 1. HEADACHE 2. STIFF NECK 3. LETHARGY B. ADMINISTER SYSTEMIC ANTIBIOTICS C. ADVICE THE CLIENT TO STAY IN BED IN A DARKENED ROOM EAR DISORDERS LABYRINTHITIS IMPLEMENTATION D. ADMINISTER ANTIEMETICS & ANTIVERTIGO MEDS. E. INSTRUCT THE CLIENT THAT THE VERTIGO SUBSIDES AS THE INFLAMMATION RESOLVES F. INSTRUCT THE CLIENT THAT BALANCE PROBLEMS THAT PERSIST MAY REQUIRE GAIT TRAINING THROUGH PHYSICAL THERAPY EAR DISORDERS MENIERE’S DISEASE • CHRONIC, RECURRENT DISORDER OF INNER EAR, IE: 1. ATACKS OF VERTIGO 2. TINNITUS 3. VESTIBULAR DYSFUNCTION • LASTS 30 MINUTES TO FULL DAY • USUALLY NO PAIN OR LOSS OF CONSCIOUSNESS EAR DISORDERS MENIERE’S DISEASE PATHOPYSIOLOGY • ASSOCIATED W/ EXCESSIVE DILATATION OF COCHLEAR DUCT ( UNILATERAL ) • RESULTING FROM OVERPRODUCTIVE OR DECREASED ABSORPTION OF ENDOLYMPH > • PROGRESSIVE SENSORINEURAL HEARING LOSS EAR DISORDERS MENIERE’S DISEASE • • • • • • • RISK FACTORS EMOTIONAL OR ENDOCRINE DISTURBANCE, ie.: DIABETES MELLITIS SPASMS OF INTERNAL AUDITORY ARTERY HEAD TRAUMA ALLERGIC REACTION HIGH SALT INTAKE SMOKING EAR INFECTIONS EAR DISORDERS MENIERE’S DISEASE • • • • • ASSESSMENT: SUBJECTIVE DATA TINNITUS HEADACHE TRUE VERTIGO, ie: A. SUDDEN ATTACKS B. ROOM APPEARS TO SPIN DEPRESSION – IRRITABILITY – WITHDRAWAL NAUSEA ON SUDDEN HEAD MOVEMENT EAR DISORDERS MENIERE’S DISEASE • • • • • • ASSESSMENT – OBJECTIVE DATA IMPAIRED HEARING, ESPECIALLY LOW TONES CHANGE IN GAIT – LACK OF COORDINATION VOMITING W/ SUDDEN HEAD MOTIONS NYSTAGMUS – DURING ATTACKS DX. TEST – CALORIC A. COLD WATER IN EAR CANAL B. MAY PRECIPITATE ATTACK DX. TEST – AUDIOMETRY A. LOSS OF HEARING EAR DISORDERS MENIERE’S DISEASE ANALYSIS / NURSING DIAGNOSIS • RISK FOR INJURY R/T VERTIGO, LACK OF COORDINATION • AUDITORY SENSORY/PERCEPTUAL ALTERATION R/T • • • • PROGRESSIVE HEARING LOSS ANXIETY R/T UNCERTAINTY ABOUT TREATMENT RISK FOR ACTIVITY INTOLERANCE R/T SUDDEN ONSET OF VERTIGO SLEEP PATTERN DISTURBANCE R/T TINNITUS INEFFECTIVE INDIVIDUAL COPING R/T CHRONIC DISORDER EAR DISORDERS MENIERE’S DISEASE NURSING CARE PLAN / IMPLEMENTATION A. GOAL : PROVIDE SAFETY & COMFORT DURING ATTACKS 1. ACTIVITY: A. BEDREST DURING ATTACKS B. SIDERAILS UP C. LOWER TO CHAIR / FLOOR IF ATTACK OCCURS WHILE STANDING D. ASSIST W/ AMBULATION – SUDDEN DIZZINESS COMMON EAR DISORDERS MENIERE’S DISEASE NURSING CARE PLAN / IMPLEMENTATION A. GOAL : PROVIDE SAFETY & COMFORT DURING ATTACKS 2. POSITION: A. RECUMBENT B. AFFECTED EAR UPPERMOST, USUALLY 3. IDENTIFY PRODROMAL SX. A. AURA B. EAR PRESSURE C. INCREASED TINNITUS 4. CALL BELL WITHIN REACH EAR DISORDERS MENIERE’S DISEASE NURSING CARE PLAN / IMPLEMENTATION B. GOAL: MINIMIZE OCCURRENCE OF ATTACKS 1. GIVE MEDICATIONS AS ORDERED 1. DIURETICS – TO DECREASE ENDOLYMPHATIC FLUIDS ( DIAMOX ) 2. ANTIHISTAMINES – TO INHIBIT TISSUE EDEMA ( BENADRYL ) 3. VASODILATORS – TO CONTROL SPASMS ( NICOTINIC ACID ) 4. ANTIEMETICS & ANTIVERTIGO AGENTS TO CONTROL NAUSEA & VOMITING ( ANTIVERT ) EAR DISORDERS MENIERE’S DISEASE NURSING CARE PLAN / IMPLEMENTATION B. GOAL: MINIMIZE OCCURRENCE OF ATTACKS 2. DIET: 1. LOW SODIUM 2. LIMITED FLUIDS TO REDUCE ENDOLYMPHATIC PRESSURE 3. AVOID PRECIPITATING STIMULI: 1. BRIGHT, GLARING LIGHTS 2. NOISE 3. SUDDEN JARRING 4. TURNING HEAD OR EYES - STAND IN FRONT OF CLIENT WHILE TALKING EAR DISORDERS MENIERE’S DISEASE NURSING CARE PLAN / IMPLEMENTATION C. GOAL: HEALTH TEACHING 1. NO SMOKING – CAUSES VASOSPASMS 2. NO ALCOHOLIC BEVERAGES 1. CAUSES FLUID RETENTION 2. CONTRAINDICATED W/ MEDS 3. MANAGEMENT OF SYMPTOMS 1. PLAY RADIO TO MASK TINNITUS, PARTICULARLY @ NIGHT EAR DISORDERS MENIERE’S DISEASE NURSING CARE PLAN / IMPLEMENTATION C. GOAL: HEALTH TEACHING 3. KEEP MEDICATION AVAILABLE @ ALL TIMES 4. PREPARE FOR SURGERY IF INDICATED: 1. LABYRINTHECTOMY – IF HEARING IS GONE 2. ENDOLYMPHATIC SAC DECOMPRESSION – TO PRESERVE HEARING EAR DISORDERS MENIERE’S DISEASE EVALUATION / OUTCOME CRITERIA A. DECREASED FREQUENCY OF ATTACKS B. COMPLIES W/ TREATMENT REGIMEN & RESTRICTIONS 1. LOW – SODIUM DIET 2. NO SMOKING C. HEARING PRESERVED EAR DISORDERS MENIERE’S DISEASE DRUG REVIEW • • • • • ANTIEMETICS – TIGAN / PHENERGAN ANTIHISTAMINES – BENADRYL / DRAMAMINE ANTIVERTIGO – VALIUM / ANTIVERT DIURETICS – DIAMOX / DIURIL VASODILATORS – NICOTINIC ACID EAR DISORDERS MASTOIDITIS • DESCRIPTION A. MAY BE ACUTE / CHRONIC B. RESULTS FROM UNTREATED / INADEQUATELY TREATED CHRONIC / ACUTE OTITIS MEDIA C. PAIN IS NOT RELIEVED BY MYRINGOTOMY • ASSESSMENT A. SWELLING BEHIND THE EAR & PAIN W/ MINIMAL MOVEMENT B. CELLULITIS ON THE SKIN / EXTERNAL SCALP OVER THE MASTOID PROCESS EAR DISORDERS MASTOIDITIS ASSESSMENT C. A REDDENED , DULL, THICK, IMMOBILE TYMPANIC MEMBRANE W/ OR W/OUT PERFORATION D. TENDER & ENLARGED POSTAURICULAR LYMPH NODES E. LOW-GRADE FEVER F. MALAISE G. ANOREXIA EAR DISORDERS MASTOIDITIS IMPLEMENTATION A. PREPARE THE CLIENT FOR SURGICAL REMOVAL OF INFECTED MATERIAL B. MONITOR FOR COMPLICATIONS C. SIMPLE / MODIFIED RADICAL MASTOIDECTOMY W/ TYMPANOPLASTY IS THE MOST COMMON TREATMENT D. ONCE TISSUE THAT IS INFECTED IS REMOVED, TYMPANOPLASTY IS PERFORMED TO RECONSTRUCT THE OSSICLES & THE TYMPANIC MEMBRANE IN AN ATTEMPT TO RESTORE NORMAL HEARING EAR DISORDERS MASTOIDITIS COMPLICATIONS A. DAMAGE TO THE ABDUCENS & FACIAL CRANIAL NERVES B. DAMAGE EXHIBITED BY INABILITY TO LOOK LATERALLY - CRANIAL NERVE VI C. DAMAGE EXHIBITED BY A DROOPING OF THE MOUTH ON THE AFFECTED SIDE - CRANIAL NERVE VII D. MENINGITIS EAR DISORDERS MASTOIDITIS COMPLICATIONS E. F. G. H. BRAIN ABCESS CHRONIC PURULENT OTITIS MEDIA WOUND INFECTIONS VERTIGO, IF THE INFECTION SPREADS INTO THE LABYRINTH EAR DISORDERS MASTOIDITIS POSTOPERATIVE IMPLEMENTATION A. MONITOR FOR DIZZINESS B. MONITOR FOR SIGNS OF MENINGITIS AS EVIDENCED BY A STIFF NECK & VOMITING C. PREPARE FOR A WOUND DRESSING CHANGE 24hrs POSTOPERATIVELY D. MONITOR THE SURGICAL INCISION FOR EDEMA DRAINAGE & REDNESS E. POSITION THE CLIENT FLAT W/ THE OPERATIVE SIDE UP EAR DISORDERS MASTOIDITIS POSTOPERATIVE IMPLEMENTATION F. RESTRICT THE CLIENT TO BED W/ BEDSIDE COMMODE PRIVILEGES FOR 24hrs AS PRESCRIBED G. ASSIST THE CLIENT W/ GETTING OUT OF BED TO PREVENT FALLING / INJURIES FROM DIZZINESS H. W/ RECONSTRUCTION OF OSSICLES VIA GRAFT, PRECAUTIONS ARE TAKEN TO PREVENT DISLODGING THE GRAFT EAR DISORDERS STAPEDECTOMY DESCRIPTION A. REMOVAL OF THE STAPES & REPLACEMENT W/ A PROSTHESIS CONSISTING OF EITHER A: 1. STEEL WIRE / 2. TEFLON PISTON / 3. POLYETHYLENE B. TREATMENT FOR DEAFNESS DUE TO OTOSCLEROSIS C. FIXES THE STAPES, PREVENTING IT FROM OSCILLATING & TRANSMITTING VIBRATIONS TO THE FLUIDS IN THE INNER EAR EAR DISORDERS STAPEDECTOMY ANALYSIS / NURSING DIAGNOSIS A. SENSORY/PERCEPTUAL ALTERATION R/T EDEMA & EAR PACKING NURSING CARE PLAN / IMPLEMENTATION A. PREOPERATIVE CARE: HEALTH TEACHING 1. IMPORTANT POSTOPERATIVELY TO KEEP HEAD IN POSITION ORDERED BY M.D. 2. AVOID SNEEZING, BLOWING NOSE, VOMITING, COUGHING – INCREASES PRESSURE IN EUSTACHIAN TUBES 3. BREATHING EXERCISES EAR DISORDERS STAPEDECTOMY NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 1. GOAL: PROMOTE PHYSICAL & PSYCHOLOGICAL EQUILIBRIUM A. POSITION: 1. AS ORDERED BY M.D.- VARIES 2. SIDE RAILS UP R/T COMMON VERTIGO B. ACTIVITY: 1. ASSIST W/ AMBULATION 2. AVOID RAPID TURNING - > VERTIGO EAR DISORDERS STAPEDECTOMY NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 1. GOAL: PROMOTE PHYSICAL & PSYCHOLOGICAL EQUILIBRIUM C. DRESSINGS: 1. CHECK FREQUENTLY 2. MAY CHANGE COTTON PLEDGET IN OUTER EAR EAR DISORDERS STAPEDECTOMY NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE D. MEDICATIONS: 1. ANTIEMETICS 2. ANALGESICS 3. ANTIBIOTICS E. REASSURANCE 1. REDUCTION IN HEARING IS NORMAL 2. HEARING MAY NOT IMMEDIATELY IMPROVE AFTER SURGERY EAR DISORDERS STAPEDECTOMY NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 2. GOAL: HEALTH TEACHING A. EAR CARE: 1. KEEP COVERED OUTDOORS 2. KEEP OUTER EAR PLUG CLEAN, DRY & CHANGED EAR DISORDERS STAPEDECTOMY NURSING CARE PLAN / IMPLEMENTATION B. POSTOPERATIVE CARE 2. GOAL: HEALTH TEACHING B. AVOID: 1. WASHING HAIR FOR 2 WEEKS 2. SWIMMING FOR 6 WEEKS 3. AIR TRAVEL FOR 6 MONTHS 4. PEOPLE W/ URI’s 5. HEAVY LIFTING / STRAINING EAR DISORDERS STAPEDECTOMY EVALUATION / OUTCOME CRITERIA A. HEARING IMPROVES 1. EVALUATE 1 MONTH POSTOPERATIVELY 2. MAY REQUIRE HEARING AID B. RETURNS TO WORK 1. USUALLY 2 WEEKS AFTER SURGERY C. CONTINUES MEDICAL SUPERVISION EAR DISORDERS FENESTRATION DESCRIPTION A. REMOVAL OF THE STAPES W/ A SMALL HOLE DRILLED IN THE FOOTPLATE B. A PROSTHESIS IS CONNECTED BETWEEN THE INCUS & FOOTPLATE C. SOUNDS CAUSE THE PROSTHESIS TO VIBRATE IN THE SAME MANNER AS DID THE STAPES D. COMPLICATIONS INCLUDE: 1. HEARING LOSS 2. PROLONGED VERTIGO 3. INFECTION 4. FACIAL NERVE DAMAGE EAR DISORDERS FENESTRATION PREOPERATIVE IMPLEMENTATION A. INSTRUCT THE CLIENT IN MEASURES TO PREVENT MIDDLE EAR / EXTERNAL EAR INFECTIONS B. INSTRUCT THE CLIENT TO AVOID EXCESSIVE NOSE BLOWING C. INSTRUCT THE CLIENT NOT TO CLEAN THE EAR CANAL W/ ANY FOREIGN OBJECT D. INSTRUCT THE CLIENT TO REMOVE HEARING AID 2 WEEKS BEFORE SURGERY TO ENSURE THE INTEGRATION OF LOCAL TISSUE EAR DISORDERS FENESTRATION POSTOPERATIVE IMPLEMENTATION A. INFORM THE CLIENT THAT HEARING IS INITIALLY WORSE AFTER THE SURGICAL PROCEDURE BECAUSE OF SWELLING & THAT NO NOTICEABLE IMPROVEMENT IN HEARING MAY OCCUR FOR AS LONG AS 6 WEEKS B. INFORM THE CLIENT THAT THE GELFOAM EAR PACKING INTERFERES W/ HEARING BUT IS USED TO DECREASE BLEEDING C. ASSIST W/ AMBULATING DURING THE FIRST 1 TO 2 DAYS AFTER SURGERY EAR DISORDERS FENESTRATION POSTOPERATIVE IMPLEMENTATION D. PROVIDE SIDE RAILS WHEN THE CLIENT IS IN BED E. ADMINISTER ANTIBIOTICS, ANTIVERTIGO & PAIN MEDS F. ASSESS FOR: 1. FACIAL NERVE DAMAGE 2. WEAKNESS 3. CHANGES IN TACTILE SENSATION 4. VERTIGO 5. NAUSEA & VOMITING EAR DISORDERS FENESTRATION POSTOPERATIVE IMPLEMENTATION G. INSTRUCT THE CLIENT TO MOVE THE HEAD SLOWLY WHEN CHANGING POSITIONS – TO PREVENT VERTIGO H. INSTRUCT THE CLIENT TO AVOID PERSONS W/ URI’s I. INSTRUCT THE CLIENT TO AVOID SHOWERING & GETTING THE HEAD AND WOUND WET EAR DISORDERS FENESTRATION POSTOPERATIVE IMPLEMENTATION J. INSTRUCT THE CLIENT TO REFRAIN FROM USING SMALL OBJECTS TO CLEAN THE EXTERNAL EAR CANAL K. INSTRUCT THE CLIENT TO AVOID RAPID, EXTREME CHANGES IN PRESSURE CAUSED BY: 1. QUICK HEAD MOVEMENTS 2. SNEEZING & NOSE BLOWING L.. INSTRUCT THE CLIENT TO AVOID CHANGES IN MIDDLE EAR PRESSURE BECAUSE THEY COULD DISLODGE THE GRAFT / PROSTHESIS EAR DISORDERS TRAUMA DESCRIPTION A. THE TYMPANIC MEMBRANE HAS A LIMITED STRETCHING ABILITY & GIVES WAY UNDER HIGH PRESSURE B. FOREIGN OBJECTS PLACED IN THE EXTERNAL CANAL MAY EXERT PRESSURE ON THE TYMPANIC MEMBRANE & CAUSE PERFORATION C. IF THE OBJECT CONTINUES THROUGH THE CANAL, THE BONY STRUCTURE OF THE STAPES, INCUS, & MALLEUS MAY BE DAMAGED EAR DISORDERS TRAUMA DESCRIPTION D. A BLUNT INJURY TO THE BASAL SKULL & EAR CAN DAMAGE THE MIDDLE EAR STRUCTURES THROUGH FRACTURES EXTENDING TO THE MIDDLE EAR E. EXCESSIVE NOSE BLOWING & RAPID CHANGES OF PRESSURE THAT OCCUR W/ NONPRESSURED AIR FLIGHTS CAN INCREASE PRESSURE IN THE MIDDLE EAR F. DEPENDING ON THE DAMAGE TO THE OSSICLES, HEARING LOSS MAY / MAY NOT RETURN EAR DISORDERS TRAUMA IMPLEMENTATION A. TYMPANIC MEMBRANE PERFORATIONS USUALLY HEAL W/IN 24 HOURS B. SURGICAL RECONSTRUCTION OF THE OSSICLES & TYMPANIC MEMBRANE THROUGH TYMPANOPLASTY / MYRINGOPLASTY MAY BE PERFORMED TO IMPROVE HEARING EAR DISORDERS CERUMEN & FOREIGN BODIES DESCRIPTION A. CERUMEN / WAX IS THE MOST COMMON CAUSE OF IMPACTED CANALS B. FOREIGN BODIES CAN INCLUDE: 1. VEGETABLES 2. BEADS 3. PENCIL ERASERS 4. INSECTS EAR DISORDERS CERUMEN & FOREIGN BODIES ASSESSMENT A. SENSATION OF FULLNESS IN THE EAR W/ W/OUT HEARING LOSS B. PAIN, ITCHING OR BLEEDING CERUMEN A. REMOVAL OF WAX BY IRRIGATION IS A SLOW PROCESS B. IRRIGATION IS CONTRAINDICATED IN CLIENTS W/ A HISTORY OF TYMPANIC MEMBRANE PERFORATION EAR DISORDERS CERUMEN & FOREIGN BODIES CERUMEN (cont’d) C. TO SOFTEN CERUMEN, ADD 3 DROPS OF GLYCERIN TO THE EAR @ BEDTIME & 3 DROPS OF HYDROGEN PEROXIDE 2 X A DAY D. AFTER SEVERAL DAYS THE EAR IS IRRIGATED E. 50 TO 70 ml. OF SOLUTION IS THE MAXIMAL AMOUNT A CLIENT CAN TOLERATE DURING AN IRRIGATION SITTING EAR DISORDERS CERUMEN & FOREIGN BODIES FOREIGN BODIES A. W/ A FOREIGN OBJECT OF VEGETABLE MATTER, IRRIGATION IS USED W/ CARE BECAUSE THIS MATERIAL EXPANDS W/ HYDRATION B. INSECTS ARE KILLED BEFORE REMOVAL UNLESS THEY CAN BE COAXED OUT BY FLASHLIGHT / A HUMMING NOISE EAR DISORDERS CERUMEN & FOREIGN BODIES FOREIGN BODIES (cont’d) C. MINERAL OIL / ALCOHOL IS INSTILLED TO SUFFOCATE THE INSECT, WHICH IS THEN REMOVED USING EAR FORCEPS D. USE A SMALL EAR FORCEPS TO REMOVE THE OBJECT & AVOID PUSHING THE OBJECT FARTHER INTO THE CANAL AND DAMAGING THE TYMPANIC MEMBRANE EAR DISORDERS ACOUSTIC NEUROMA DESCRIPTION A. A BENIGN TUMOR OF THE VESTIBULAR / ACOUSTIC NERVE B. THE TUMOR MAY CAUSE DAMAGE TO HEARING & TO FACIAL MOVEMENTS AND SENSATIONS C. TREATAMENT INCLUDES SURGICAL REMOVAL OF THE TUMOR VIA CRANIOTOMY EAR DISORDERS ACOUSTIC NEUROMA DESCRIPTION D. CARE IS TAKEN TO PRESERVE THE FUNCTION OF THE FACIAL NERVE E. THE TUMOR RARELY RECURS AFTER SURGICAL REMOVAL F. POSTOPERATIVE NURSING CARE IS SIMILAR TO POSTOPERATIVE CRANIOTOMY CARE EAR DISORDERS ACOUSTIC NEUROMA ASSESSMENT A. SYMPTOMS USUALLY BEGIN W/ TINNITUS & PROGRESS TO GRADUAL SENSORINEURAL HEARING LOSS B. AS THE TUMOR ENLARGES, DAMAGE IN ADJACENY CRANIAL NERVES OCCURS