The FUNDamentals of DME Equipment:

The FUNDamentals of
DME Equipment:
A Guide for Selection, Acquisition, and Delivery of Complex
Rehab Technology
Beth Beach MS, OTR/L, ATP
Tony Leo MOT/L, ATP
AEL/NRTTS
What is Durable Medical
Equipment (DME)?
Durable Medical Equipment must meet the following criteria (Medicare.gov 2014):
1. Is durable or long-lasting
2. Is used for a medical reason
3. Is not usually useful to someone who isn’t sick, injured or disabled
4. Is used in the home
What is complex rehab technology (CRT)?
“Complex Rehab Technology products and services include medically necessary, individually-configured manual and power wheelchair systems, adaptive seating systems, alternative positioning systems, and other mobility devices that require evaluation, fitting, configuration, adjustment or programming.” (NuMotion/NCART)
Who needs complex rehab technology?
“Primary diagnoses that can require Complex Rehab
Technology include, but are not limited to, spinal cord injury, traumatic brain injury, cerebral palsy, muscular dystrophy, spina bifida, osteogenesis imperfecta, arthrogryposis, amyotrophic lateral sclerosis (ALS), multiple sclerosis, demyelinating diseases, myelopathy, progressive muscular atrophy, anterior horn cell diseases, post polio paralysis, cerebellar degeneration, dystonia,
Huntington’s chorea, spinocerebellar disease, amputation, paralysis or paresis, or any other disability or disease that may require the use of such individually configured products and services.” (NuMotion/NCART)
General Funding Guidelines for CRT
The client requires the equipment long-term
The equipment will improve the client’s function
MRADLs) within the home and, if under 21, the school environment
Other less expensive/extensive equipment has been considered but will not meet the client’s current and anticipated needs (i.e. progressive disease)
Manual Wheelchair criteria
[Needs to meet criteria A, B, C, D, E, + F or G]
A. Cannot participate in 1 or more mobility related activities of daily live (MRADL) such as toileting, feeding, dressing, grooming, and bathing in customary locations in the home
B. Cannot be resolved with a cane or walker
C. Patient’s home has adequate access and maneuverability
D. Use of chair will improve MRADLs and patient will use on a regular basis
E. Patient has not expressed unwillingness to use chair
F. Patient has sufficient capabilities to self-propel the chair during a typical day
G. Patient has caregiver who is willing to assist with chair
Source: OttoBock.com
Manual Wheelchair Criteria
Standard Hemi-Chair (K0002):
Patient requires a lower seat height (17”-18”) because:
Short stature, OR
Need to place feet on ground for propulsion.
Lightweight Chair (K0003):
Patient cannot self-propel in a standard wheelchair using arms and/or legs; AND
Patient can and does self-propel in a lightweight wheelchair (min 2 hr/day).
Source: OttoBock.com
Manual Wheelchair criteria
High Strength Lightweight Chair (K0004):
Patient’s ability to self-propel the wheelchair while engaging in frequent activities
that cannot be performed in a standard or lightweight wheelchair; AND/OR
Requires seat width, depth, height that cannot be accommodated in a standard, lightweight, or hemi-wheelchair and spends at least 2 hours a day in the chair
Ultralight Wheelchair (K0005) payment determined on an individual consideration basis
Description of the K0005 features that are needed compared to the K0004 base.
Source: OttoBock.com
K0005- The Mystery Explained
Per Medicare criteria, a K0005 wheelchair is covered if 1 or 2 is met and 3 and 4 are met:
1. The beneficiary must be a full-time manual wheelchair user OR
2. The beneficiary must require individualized fitting and adjustments for one or more features such as, but not limited to, axle configuration, wheelchair camber, or seat/back angles which cannot be accommodated through a lower level chair AND
K0005
3. The beneficiary must have a specialty evaluation thatwas performed by a licensed/certified medical professional (LCMP), such as a PT or OT or physician who has specific training and experience in rehabilitation wheelchair evaluations and that documents the medical necessity for the wheelchair and its special features. The
LCMP must have no financial relationship with the supplier
AND
K0005
4. The wheelchair is provided by a Rehabilitative
Technology Supplier (RTS) that employs a RESNA certified
Assistive Technology Professional (ATP) who specializes in wheelchairs and who has direct, in-person involvement in the wheelchair selection for the patient.
Tilt in Space Wheelchairs
Tilt in Space coverage criteria
Needs to meet criteria A, B, C, D, E, + F or G]
A. Cannot participate in 1 or more mobility related activities of daily live (MRADL) such as toileting, feeding, dressing, grooming, and bathing in customary locations in the home
B. Cannot be resolved with a cane or walker
C. Patient’s home has adequate access and maneuverability
D. Use of chair will improve MRADLs and patient will use on a regular basis
E. Patient has not expressed unwillingness to use chair
F. Patient has sufficient capabilities to self-propel the chair during a typical day
G. Patient has caregiver who is willing to assist with chair
Source: OttoBock.com
Tilt in Space coverage criteria
Client must have a specialty evaluation that was performed by a licensed/certified medical professional
(LCMP), as previously noted.
The wheelchair is provided by a Rehabilitative
Technology Supplier (RTS) that employs a RESNAcertified Assistive Technology Professional (ATP) who specializes in wheelchairs and who has direct, in-person involvement in the wheelchair selection for the patient.
Note: as of 4/1/14, tilt in space frames are rentals under Medicare
Power Mobility Device criteria
Patient has mobility limitation that significantly impairs mobility related activities of daily living abilities
Prevents ability to accomplish
Can't accomplish safely
Can't accomplish in reasonable time
Limitation not resolved by cane or walker
Limitation not resolved by optimally configured manual wheelchair
* wheelchairjunkie.com
POV vs. Power Wheelchair
In order to request a power wheelchair, a power operated vehicle, or scooter must be ruled out as an option for the client
POV has a tiller for operation
POV has captain’s type seating
POV is usually longer than a power chair
Transfers can be an issue with a POV
Power Chair Groups
Group 1 power chair
Standard integrated or remote proportional control input device- cannot be upgraded for specialty controls
Non-expandable controller- cannot be upgraded
Accommodates non-powered options (i.e. manual recline and manual elevating legrests)
These chairs are not considered complex rehab technology and fall under competitive bidding for Medicare
Group 1 Power Wheelchair
Power Chair Groups
Group 2 power chair
Standard integrated or remote proportional control input device
Accommodates seating and positioning components such as specialty backs, cushions
Can accommodate power functions such as power tilt and/or recline
These cannot be upgraded with specialty controls and power functions are more limited- not CRT under Medicare
Group 2 Power Wheelchair
Power Chair Groups
Group 3 power chairs
Standard integrated or remote proportional control input device
Accommodates seating and positioning components such as specialty backs and cushions
Can be upgraded with specialty controls
Has options for multiple power functions
This is the first category considered CRT under Medicare
Group 3 Power wheelchairs
Mid-wheel Front wheel
Rear wheel
Power Chair Groups
Group 4 power chairs
Not covered under Medicare as they have essentially the same options as group 3, just are more heavy duty and faster.
Group 5 power chairs
These are pediatric power wheelchairs
Power Chair Groups
Group 4 Group 5
Seating
Skin Protection and/or Positioning Seat Cushions
•
Positioning Backs
•
Positioning Accessories
•
Custom Fabricated Seating
Must have a manual wheelchair or power wheelchair with sling/solid seat and back and meet MCR coverage criteria for the skin protection and/or positioning seat or back.
Role of the therapist
Evaluate patient and document need for complex rehab technology in a letter of medical necessity
Communicate with other team members- rehab technology specialist (RTS), physician, treating therapists, case managers, client and family
Role of the therapist
50% of orders in the Medicare Demonstration Project are denied.
A majority of the denied prior authorizations relied on
Physician chart notes and did not include a therapy evaluation.
When the customer sees a therapist for a wheelchair evaluation, the approval rate jumps to around 90%.
When there is a comprehensive therapy evaluation, the process moves faster and the customer is more likely to get their chair approved without needing repeat visits.
Letter of Medical Necessity
Introduces the client- age, sex, diagnosis, past medical history
Discusses what equipment the client has presently and what the problems are with the equipment
Standard therapy evaluation including strength, range of motion, bed/floor mobility, sitting balance, head control, tone, etc.
States the equipment recommended and WHY each component is necessary
Letter of Medical Necessity
Clinician or the Clinic’s own form (meeting all coverage criteria) VOTA
2014\Medicare LMN Requirements.pdf
Orion FME VOTA 2014\Group 3 Power Multiple Seat functions - Copy.pdf
Illinois Seating/Mobility Evaluation (12 Page Eval) VOTA 2014\Seating Eval Form from Illinois Public Aid_019.pdf
State Medicaid and other Payer Specific Wheelchair or Equipment Forms; as required but must be approved for Medicare Funding VOTA 2014\handout- sample
CHKD LMN.doc
Role of the ATP/RTS
The ATP can never complete any portion of the PT/OT
Evaluation prior to, or after the evaluation.
The only exception is the demographics portion of the form, which may be completed before the evaluation.
The ATP must complete a separate Client Assessment for all
Medicare orders requiring ATP involvement per Medicare policy.
The Client Assessment must be completed, signed and dated by the ATP, including credentials to prove involvement in the mobility evaluation
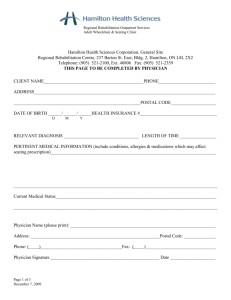
Medicare Forms
F2F
Chart notes
7 element prescription
Face to Face
• History of the present condition(s) and past medical history that is relevant to mobility needs.
• Symptoms that limit ambulation
• Diagnoses that are responsible for these symptoms
• Other diagnoses that may relate to ambulatory problems
• Medications or other treatments for these symptoms
• Progression of ambulation difficulty over time
• How far the patient can walk without stopping
• Pace of ambulation
• History of falls, including frequency, circumstances leading to falls, and why lesser equipment would not be sufficient
• What ambulatory assistance (cane, walker, MWC, caregiver, etc.) is currently being used and why isn’t it sufficient?
Face to Face
• What has changed to now require the use of a power mobility device?
• Description of the home setting
• The ability to perform MRADLs in the HOME
• Physical Examination that is relevant to mobility needs.
• Weight & Height - Medicare will deny even a standard PWC if the client exceeds 95% of the weight capacity per Medicare guidelines.
• Cardiopulmonary examination
• Musculoskeletal examination including upper and lower extremity strength and range of motion measurements
• Neurological examination including gait, balance and coordination
Chart Notes
• The F2F must occur BEFORE the physician completes the 7 element written order.
• Medicare requires the doctor’s findings to be documented in a detailed narrative note in the same format as all other entries in the client’s file.
• The note needs to clearly indicate that the major reason for the visit was a mobility examination.
• The history should paint a picture of the patient’s functional abilities and limitations on a typical day. It should contain as much objective data as possible.
7 Element Prescription
Must contain each of the following elements and must be COMPLETED BY THE PHYSICIAN after conducting the F2F examination (can be on the same day, but never before):
Beneficiary’s Name
Description of the Item
(may be general – e.g. “power wheelchair”), or may be more specific
Date of the completion of the F2F examination
Pertinent diagnosis or conditions that relate to the power mobility device
Length of need
The treating physician’s signature
The date the treating physician signed the order
7 ELEMENT PRESCRIPTION
***graphic abbreviated for content only
— The Numotion 7 Element Written
Order has been revised for easier use.
— Contains a more accurate statement under element #2 to assist the physician with understanding the face to face completion date.
— The 7 Element Written Order is to be completed entirely by the physician.
— No fields can be completed by the supplier or medical office staff.
40
Appeals
Important to be sure that you review the insurance’s coverage criteria for the equipment prior to filing an appeal
First appeal is usually written. Can be filed by the patient, family or representative of the family. Must have an authorized representative statement signed by the patient/family to file the appeal
If appeal is denied, the next step is usually a telephone hearing
Some insurances allow peer to peer reviews
Insurance Trends
Denial of standers as “experimental and investigational”
Denial of adaptive strollers for distances as
“convenience to the caregiver” or “restraint of the individual”
Denial of adaptive beds for safety purposes
Denial of back up wheelchairs or strollers
Denial of bath equipment for very small children and teenagers/young adults “convenience items”
Alternate Funding Sources
Virginia Birth Injury Fund
Charities- both local and national
EPSDT
VOTA 2014\Handout- RESOURCES FOR FUNDING
ADAPTIVE EQUIPMENT (VA).doc