ACUTE CORONARY SYNDROMES
advertisement

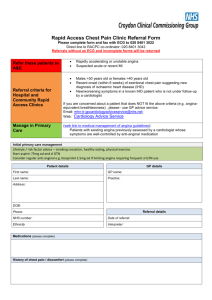
ACUTE CORONARY SYNDROMES R MAHARAJ EMERGENCY MEDICINE LECTURE OUTLINE • INTRODUCTION – EPIDEMIOLOGY/PREVALENCE/DEFINITION • PATHOPHYSIOLOGY OF ACUTE CORONARY SYNDROMES • APPROACH TO SUSPECTED ACUTE CORONARY SYNDROME – GUIDELINE UPDATE • TREATMENT/MANAGEMENT UPDATE INTRODUCTION • Coronary Artery Disease – leading cause of morbidity & mortality in industrialised nations. • Although decrease in cardiovascular mortality still major cause of morbidity & burden of disease. • South African perspective of cardiovascular disease: • “A World in One Country” - Yusuf et al • Epidemiological transitions of cardiovascular disease. • HIGH RISK POPULATION FOR CAD/ACS: INDIAN/WHITE/COLOURED • INCREASING rate in Black population – lifestyle/socioeconomic changes, urbanisation • GF Jooste stats: 23.8% of admissions to resus. unit for chest pain/acs related (stats 1Jan 2009 – 28 Feb 2009) 150/628 entries. • In US – 2004 – 1.56 million admissions for ACS – 669 000 for unstable angina, 896 000 for MI • Higher prevelance for NSTEMI. DEFINITIONS • CAD is a continuum of disease…. • Angina -> unstable angina -> AMI -> sudden cardiac death • Acute coronary syndrome encompasses unstable angina, NSTEMI, STEMI • Stable angina – transient episodic chest pain d/t myocardial ischaemia, reproducible, frequency constant over time.usually relieved with rest/NTG. • Classification of angina – Canadian Cardiovascular Society classification. Canadian Cardiovascular Association Classification of Angina CLASS 1 NO PAIN WITH ORDINARY PHYSICAL ACTIVITY CLASS 2 SLIGHT LIMITATION OF PHYSICAL ACTIVITY – PAIN OCCURS WITH WALKING, CLIMBING STAIRS,STRESS CLASS 3 SEVERE LIMITATION OF DAILY ACTIVITY – PAIN OCCURS ON MINIMAL EXERTION CLASS 4 UNABLE TO CONDUCT ANY ACTIVITY WITHOUT PAIN, PAIN AT REST • UNSTABLE ANGINA – • Pain occurring at rest – duration > 20min, within one week of first visit • New onset angina – ~ Class 2 severity, onset with last 2 months • Worsening of chest pain – increase by at least 1 class, increases in frequency, duration • Angina becoming resistance to drugs that previously gave good control. • NB! ECG – normal, ST depression(>0.5mm), T wave changes • ACUTE MYOCARDIAL INFARCTION – • ECC/ACC DEFN –rise and fall in cardiac enzymes with one or more of the following: • Ischaemic type chest pain/symptoms • ECG changes – ST changes, pathological Q waves • Coronary artery intervention data • Pathological findings of an acute MI • NSTEMI = UNSTABLE ANGINA SYMPTOMS/FINDINGS + POSITIVE CARDIAC ENZYMES • STEMI = ST ELEVATION ON ECG + SYMPTOMS • WHY IS IT IMPORTANT TO RECOGNISE PATIENTS WITH UNSTABLE ANGINA?? • 5 -17% suffer an MI within a week after admission. • 3 -15% die within a year. ACS PATHOPHYSIOLOGY • Distruption of coronary artery plaque -> platelet activation/aggregation /activation of coagulation cascade -> endothelial vasoconstriction ->intraluminal thrombus/embolisation -> obstruction -> ACS • Severity of coronary vessel obstruction & extent of myocardium involved determines characteristics of clinical presentation APPROACH • • • • • • • Identifying those with chest pain suggestive of IHD/ACS. Thorough history required: Character of pain Onset and duration Location and radiation Aggravating and relieving factors Autonomic symptoms • TYPICAL VS ATYPICAL HISTORY • Failure to recognise symptoms other than chest pain -> approx 2 hr delay in seeking medical attention CHARACTERISTICS OF TYPICAL ANGINAL CHEST PAIN (ADAPTED FROM ROSEN’S, EMERGENCY MEDICINE) CHARACTERISTIC SUGGESTIVE OF ANGINA LESS SUGGESTIVE OF ANGINA TYPE OF PAIN DULL PRESSURE/CRUSHING PAIN SHARP/STABBING DURATION 2-5 MIN, <20 MIN SECONDSTO HOURS/CONTINUOUS ONSET GRADUAL RAPID LOCATION/CHEST WALL TENDERNESS SUBSTERNAL, NOT TENDER TO PALP. LATERAL CHEST WALL/TENDER TO PALP. REPRODUCIBALITY WITH EXERTION/ACTIVITY WITH BREATHING/MOVING AUTONOMIC SYMPTOMS PRESENT USUALLY ABSENT ATYPICAL PAIN • • • • • • • • • • • • RISK FACTORS FOR DEVELOPING ATYPICAL PAIN: Diabetes, females, non white patients, elderly, dementia, no prior history of MI ATYPICAL SYMPTOMS: GIT symptoms Syncope SOB Pleuritic/positional pain Chest wall tenderness No chest pain/symptoms NRMI 2 STUDY – MI without chest pain -> increased risk of death (23% vs 9%) More complications – hypotension,heart failure, stroke Delayed ED presentation, delayed intervention RISK STRATIFICATION IN ACS • Reasons : • Provides prognostic information • Determines treatment and level of intervention -> low risk patients – early discharge, high risk -> admission to high care • Helps decongest the ED and make available medical resources to more needy patients • Risk stratification should be ongoing – at admission, 6-8 hrs, 24hrs, discharge TOOLS USED IN RISK STRATIFICATION • HISTORY • ECG • BIOCHEMICAL MARKERS ECG • First point of entry into ACS algorithm • Abnormal or normal • Neither 100% sensitive or 100% specific for AMI • Single ECG for AMI – sensitivity of 60%, specificity 90% • Represents single point in time –needs to be read in context • Normal ECG does not exclude ACS – 1-6% proven to have AMI, 4% unstable angina • GUIDELINES: • Initial 12 lead ECG – goal door to ECG time 10min, read by experienced doctor (Class 1 B) • If ECG not diagnostic/high suspicion of ACS – serial ECGs initially 15 -30 min intervals (Class 1 B) • ECG adjuncts – leads V7 –V9, RV 4 (Class 2a B) • Continuous 12 lead ECG monitoring reasonable alternative to serial ECGs (Class 2a B) BIOCHEMICAL MARKERS • • • • • • IDEAL MARKER: High concentration in myocardium Myocardium specific Released early in injury Proportionate to injury Non expensive testing • • • • Troponins CKMB Myoglobin Other markers TROPONINS T/I • Troponin T vs I – • both equivalent in diagnostic and prognostic abilities ( except in renal failure – Trop T less sensitive) • Elevation ~ 2hrs to 12hrs • ~30 – 40% of ACS patients without ST elevation – had normal CKMB but elevated troponins on presentation • Meta-analysis (Heindereich et al) – odds of death increased 3 to 8 fold with positive troponin • Mortality at 42 days in troponin positive patients MYOGLOBIN • Rapid release within 2 hours • Not cardiac specific • Rule out for NSTEMI rather than rule in. CKMB Used in conjunction with troponins Useful in diagnosing re-infarction MARKER CHANGE SCORES • 2 hour delta CKMB mass • Aim – to exclude MI within 6hrs of symptom onset • Determine changes in serum marker levels over certain time intervals –delta values • Increasing values while still within normal range suggestive of ischaemia – more rapid anti- ischaemic mxn. OTHER MARKERS • INDICATORS OF INFLAMMATION OR ACTIVATION OF COAGULATION CASCADE: • Myeloperoxidase, soluble CD40 ligand, IL6, hsCRP, d dimer, prothrombin fragment 1 & 2 • Elevated before onset of irreversible injury • Lack specificity • Complex lab assays ISCHAEMIA MODIFIED ALBUMIN • Measured with albumin cobalt binding assay • In ischaemia -> decreased binding of albumin to cobalt • Increased with minutes of ischaemia – elevated for 6-12hrs – gone by 24hrs • ~90% negative predictive value • Combined with myoglobin/CKMB/troponin – increases diagnostic sensitivity of ischaemia by 40% • Possible role for rule criteria in low risk patients • Positive IMA – high risk patients – more aggressive mxn • Positive in hypoxic disorders – poor specificity in this setting • B –type Natriuretic Peptide: • released from heart muscle in response to increased ventricular wall stress. • Studies – BNP not a specific marker but a strong predictor of ACS especially in patients with chest pain, no ECG changes, non diagnostic troponins. • Also positive in heart failure, PE, atrial arrythmias, renal failure • Pregnancy Associated Plasma Protein A (PAPP-A): • Released when plaque ruptures • Predictor of ischaemia • HEART FATTY ACID BINDING PROTEIN (HF ABP) • Identifies AMI <4hrs after onset • Protein involved in myocardial lipid synthesis, but also expressed outside heart • Therefore may be sensitive but not specific for injury • Possible role in multi-marker strategy • • • • • IMAGING MODALITIES Cardiac MRI Multidetector CT for coronary calcification Coronary CT angiography Undergoing clinical evaluation • 2007 ACC/AHA guidelines: • Cardiac biomarkers measured in all patients with suspicion of ACS (Class 1 B) • Troponin preferred marker( Class 1 B) • If troponin negative within 6 hours of onset, repeat 8-12hours later(Class 1 B) • Remeasuring of positive biomarkers to determine infarct size/necrosis (Class 2a B) • Patients presenting within 6 hours of symptom onset – myoglobin in conjunction with troponin measured (Class 2b B) • 2hr delta CKMB/Delta troponin considered in <6hr presentation (Class 2b B) • BNP level – for global risk assessment(Class 2b B) • Class 3 – AST/LDH/CK without CKMB RISK STRATIFICATION MODELS TIMI RISK SCORE –increase in mortality with increasing score ~40% all cause mortality at 14 days for patients requiring urgent revascularisation WHICH MODEL IS MOST APPROPRIATE?? • 2007 ACS/AHA GUIDELINES: • Risk stratification models useful in decision making with regard to treatment options ( Class 2a B) • TIMI vs GRACE vs PURSUIT • PURSUIT & GRACE risk scores allow better discrimination of in hospital and 1 year mortality in patients compared to TIMI. (Andrew et al, Risk scores for risk stratification in ACS …) • What’s appropriate in our setting??? MANAGEMENT ALGORITHM MANAGEMENT UPDATE 2007ACS/AHA GUIDELINES: Rapid catergorisation of patient (Class 1 C) Possible ACS, non diagnostic ECG/biomarkers – observed in facility with cardiac monitoring (Class 1 C) Alternative to in patient treatment: for those with 12hr ECG/markers negative – stress ECG in 72hrs (Class 1 C) Giving precautionary treatment for those for OPD stress (Class 1 B) INITIAL INVASIVE VS INITIAL CONSERVATIVE STRATEGY • CLASS 1 RECOMMENDATIONS: • Early invasive strategy for refractory angina, hemodynamic instability (LOE B) • Early invasive strategy for stabilised patients with elevated risk for clinical events. • High risk factors include: • • • • • • • • • Recurrent angina, ischaemia at rest or minimal activity Elevated troponins New ST depression Signs of heart failure/worsening mitral regurg. Ventricular tachycardia Prior CABG PCI in last 6 months High TIMI/GRACE scores LVEF < 40% • CLASS 2b • May opt for initial conservative strategy in stabilised high risk patients – dependent on patient/physician preference (LOE B) • CLASS 3 • Invasive strategy -not recommended in patients with multiple co morbidities, low risk patients, patients not consenting.(LOE C) UA/NSTEMI –PHARMACOTHERAPY UPDATE • GENERAL: • IV B Blockers downgraded from Class 1 to 2a recommendation. (COMMIT Trial) • Oral B Blockers in first 24hrs still Class 1 – but not used in signs of heart failure, cardiogenic shock and reactive airway disease.(LOE B) • MORPHINE downgraded from Class 1 to 2a – findings from CRUSADE Registry NSTEMI- PHARMACOTHERAPY UPDATE • • • • • ANTIPLATELET THERAPY: CLASS 1 RECOMMENDATION Aspirin to all patients as soon as possible and continued (if no C/I) (LOE A) Initial dose 162 -325mg Maintenance 75 -162mg No added benefit from higher doses except post stenting • Clopidogrel for those allergic to aspirin or major GI bleeding (LOE A) • For initial invasive strategy – aspirin + clopidogrel or IV glycoprotein 2b/3a therapy (LOE A) Abciximab if no delay in angiography/PCI, eptifibatide/tirofiban if delayed angiography(LOE B) • • CLASS 2a • In patients managed conservatively who develop recurrent ischaemia – on clopidogrel/ASA/Anticoagulant – can add glycoprotein inhibitor. (LOE C) • Invasive strategy – can use clopidogrel + glycoprotein inhibitors(LOE C) • CLASS 2b • In patients managed conservatively – can add glycoprotein inhibitor therapy, in addition to aspirin & anticoagulant (LOE B) CLASS 3 • ABCIXIMAB should not be given if PCI not planned (LOE A) • For initial conservative strategy: • Aspirin + Clopidogrel + anticoagulant – administered for 1 month(LOE A), continued ideally up to 1 year(LOE B) • If initial conservative strategy selected but patient has recurrent ischaemic symptoms/heart failure/arrythmias – diagnostic angiography recommended. Clopidogrel or Glycoprotein 2b/3a inhibitors should be added before angiography. ANTICOAGULANT THERAPY CLASS 1 • Anticoagulant therapy should be added as soon as possible • For patients undergoing angiography/PCI – enoxaparin/UFH (LOE A) of Bivalirudin/ fondaparinux (LOE B) • For conservative strategy: enaxaparin, UFH (LOE A), fondaparinux • For patients with increased risk of bleeding with conservative strategy – fondaparinux • CLASS 2a • Enoxaparin /fondaparinux vs UFH • Enoxaparin/fondaparinux preferred except in those undergoing CABG within 24hrs (LOE B) ADDITIONAL MANAGEMENT • STRESS TEST should be performed for those managed conservatively. • If stress test positive/ high risk – needs diagnostic angiography(Class 1 LOE A) • If classed as low risk – • need to continue aspirin indefinitely ( LOE A) • Clopidogrel for at least 1 month(LOE A), ideally up to 1 year(LOE B) UA/NSTEMI ALGORITHM- INVASIVE STRATEGY UA/NSTEMI ALGORITHM –CONSERVATIVE STRATEGY STEMI • PHARMACOLOGICAL UPDATE: • ANALGESIA – changes from 2004 guidelines • MORPHINE: still remains Class 1 C for STEMI, titrated doses • NSAIDS/COX 2 INHIBITORS: those on it should have it discontinued ( increased risk of mortality, re infarction, heart failure, myocardial rupture) Class 1 C • NSAIDS should not be administered in hospital for MI (Class 3) • BETA BLOCKERS • Modified recommendation • Oral Beta Blockers should be initiated in first24rs, if no contraindications (heart failure, risk of cardiogenic shock) Class 1 B • Patients with early contraindications -> re- evaluated later for possible use • Role of IV B blockers – used in hypertensive patients with STEMI Class 2a B • Class 3 LOE A – IV B blockers should not be administrated to patients with heart failure, risk of cardiogenic shock • No major changes to reperfusion strategies. • Emphasis on decreasing ischaemic time. • Increase use of prehospital 12 lead ECG emphasised. • In PCI capable hospital – door to PCI time 90 min (Class 1 A) • In non PCI capable hospital – door to needle time 30 min or timeous transfer to PCI capable hospital. (Class 1 B) REPERFUSION STRATEGY FIBRINOLYTICS • • • • • • • AVAILABLE FIBRINOLYTICS: STREPTOKINASE – 1.5mu infusion over 30min (1hour –ACLS) rtPA – accelerated infusion over 1.5hrs - 15mg IV bolus, 0.75mg/kg over 30 min, 0.5mg/kg over 1hr ANISTREPLASE – 30 U IV over 5 min TENECTEPLASE – 30 TO 50 MG RETEPLASE – 10 U IV bolus, ffd. 10U IV after 30 min • • WHICH FIBRINOLYTIC TO USE??? GISSI 2 trial – tPA vs Streptokinase , no difference in mortality, marginally higher stroke rate with tPA (1.3% vs 1%) GUSTO 1 trial – early vessel patency post infract assoc. with better survival. Accl. tPA/heparin cf comb. Streptokinase/tPA/heprain cf strep with IV vs S/C heparin Outcome – better flow rates with accl. tPA -> lower mortality rates • • • • ASSENT 2 TRIAL – tenecteplase vs aTPA • - tenecteplase was equally or minimally more effective, especially in those presenting > 4hrs after symptom onset. • Fibrinolysis combined with glycoprotein 2b/3a inhibitors – no overall advantage (ASSENT 3, GUSTO 5 trials) • RESCUE PCI: • CLASS 1 LOE B – angiography with +/- PCI in patients (<75 yrs)with cardiogenic shock, severe heart failure, ventricular dysrythmias • Class 2a – persistent ischaemic symptoms post fibrinolysis, haemodynamic instability, electrical instability (LOE C) • New recommendation – PCI for failed fibrinolytic therapy (less than 50% decrease in ST elevation in worst lead, 90min post fibrinolytic therapy, or large area of myocardium injured) LOE B • Class 3 – angiography performed if invasive strategy contraindicated, or patient refusal (LOE C) ANTICOAGULANT ADJUNCTS • NEW RECOMMENDATIONS: CLASS 1 • Patients undergoing fibrinolysis should be kept on anticoagulants for atleast 48 hrs and preferably the duration of hospital stay. LOE A • Anti coagulants with proven efficacy: • Unfractionated Heparin - keeping aPTT 1.5 – 2 sec above control (LOE C) • Enoxaparin (Clexane) – initial dosage of 30mg IV bolus – ffd by 1mg/kg 12hrly, caution in renal impairment (LOE A) • Fondaparinux – 2.5mg IV, ffd by 2.5mg dly S/C maintenance for duration of hospitalisation (LOE B) ANTICOAGULANTS • CLASS 2a recommendation to use anticoagulants in STEMI without reperfusion. • UFH (LOE B) • LMWH (LOE C) • Fondaparinux (LOE B) THIENOPYRIDINES CLASS I • CLOPIDOGREL – now recommended in all STEMI patients in addition to aspirin, whether undergoing reperfusion or not. Dosage 75mg daily(LOE A) • Duration -14 days (LOE B) CLASS 2 A In patients < 75yrs – Clopidogrel 300mg loading dose recommended(LOE C) Long term maintenance therapy should be considered, 75mg dly for 1 year (LOE C) SECONDARY PREVENTION • INCREASED FOCUS ON SECONDARY PREVENTION: • SMOKING CESSATION • DIET MODIFICATION/WT CONTROL • BP CONTROL • LIPID MANAGEMENT • EXERCISE • DIABETES MANAGEMENT • Despite good reperfusion strategies approx. 1/3 of patients worldwide miss out. • Attributed to – delayed presentation, atypical presentation, complicated disease presentation, older age • SYMPTOMS OF INFARCT BUT NO ESTABILISHED ECG CHANGES - keep in mind aortic dissection, GIT disease, other chest pathology CONCLUSION • With increase burden of CVD, and lack of health resources risk stratification becomes important. • Emphasis should also be placed on primary &secondary prevention of ACS. • Early intervention helps prevent complications, decreases morbidity & mortality • The way forward – fully equipped CHEST PAIN OBSERVATION UNIT REFERENCES • EDITORS MARX ET AL, ROSEN’S EMERGENCY MEDICINE: CONCEPTS AND CLINICAL PRACTICE, 6TH EDITION • PAUL PD ET AL, KEY ARTICLES IN MANAGEMENT OF ACS & PCI -2007 UPDATE, PHARMACOTHERAPY 2007:27(12), 1722 -1750 • WHITE HD, DEFINING THE LIMITS OF ACS, CARDIOLOGY AT THE LIMITS IV, EDITORS: OPIE LH, YELLON DM • YUSUF S, THE GLOBAL EPIDEMIC OF ATHEROSCLEROTIC CARDIOVASCULAR DISEASE, CARDIOLOGY AT THE LIMITS IV, EDITORS: OPIE LH, YELLON DM • FOX KA, MANAGEMENT OF ACS: AN UPDATE, HEART.2004 JUNE, 90(6):698 -706 • ANDERSON ET AL, ACC/AHA 2007 GUIDELINES FOR MXN OF U/A,NSTEMI – EXECUTIVE SUMMARY – DOWNLOADED content.onlinejacc.org • SIX AJ ET AL, CHEST PAIN IN THE ER: VALUE OF THE HEART SCORE, NETH. HEART J. 2008 JUNE,16(6):191 -196 • ANTMAN EM ET AL, 2007 FOCUSSED UPDATE OF ACC/AHA 2004 GUIDELINES FOR MAXN OF PATIENTS WITH STEMI, DOWNLOADED http://circ.ahajournals.org • McCANN CJ ET AL, NOVEL BIOMARKERS IN EARLY DIAGNOSIS OF AMI COMPARED WITH CARDIAC TROPONIN T, EUROPEAN HEART JOURNAL 2008,29(23): 2843 -2850 • KING III SB ET AL, 2007 FOCUSSED UPDATE OF ACC…..FOR PCI, JOURNAL OF AMERICAN COLLEGE OF CARDIOLOGY, VOL 51, NO 2, 2008