PBL @ CHARLES !
advertisement

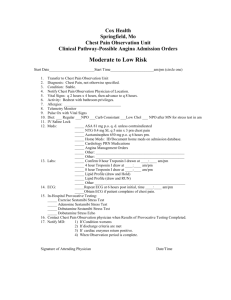
Action: Detail all the aspects of the nursing assessment you will undertake in the recovery room to determine whether Charles is safe to be transferred back to the ward. Ensure each aspect of your assessment is supported with sound rationale. Postoperative patients must be awake, alert, and medically stable before transfer. From an anaesthetic point of view, a patient can be discharged from the recovery room (a) When he is able to maintain adequate alveolar ventilation and can clear his airway; (b) He is awake, alert, well orientated in space and time and can make his wants and needs known, and (c) If he is able to maintain adequate tissue perfusion, without continuous monitoring and support of his cardio-vascular system. Patients with unstable cardio-vascular systems should not be moved, unless they are well stabilized. Action: Find a reliable information source that you believe clearly describes the pathophysiology and management of compartment syndrome. Fully discuss this within your team, and ensure you have the knowledge necessary to respond safely and effectively in a similar situation. Compartment syndrome is the compression of nerves, blood vessels, and muscle inside a closed space (compartment) within the body. This leads to tissue death from lack of oxygenation due to the blood vessels being compressed by the raised pressure within the compartment. Compartment syndrome most often involves the forearm and lower leg. When pressure is elevated, capillary blood flow is compromised. Oedema of the soft tissue within the compartment further raises the intra-compartment pressure, which compromises venous and lymphatic drainage of the injured area. Pressure, if further increased in a reinforcing vicious circle, can compromise arteriole perfusion, leading to further tissue ischemia. Untreated compartment syndrome-mediated ischemia of the muscles and nerves leads to eventual irreversible damage and death of the tissues within the compartment. There are three main mechanisms that are hypothesized to cause compartment syndrome: One idea is the increase in arterial pressure (due to increased blood flow due to trauma or excessive exercise) causes the arteries to spasm and this causes the pressures in the muscle to increase even further. Second, obstruction of the microcirculatory system is hypothesized. Finally, there is the idea of arterial or venous collapse due to transmural pressure. Management: Procedure: Neurovascular Assessment in the Adult Patient. 1. Check patient’s clinical notes for medical instructions on frequency of neurovascular limb assessment (as a minimum, this must be done 4 hourly) 2. Explain the procedure to the patient/family/whanau and ensure an understanding of the process. 3. Discuss any possible discomfort they might experience. If possible establish a hand signal so the patient can indicate if they need a break during the procedure. 4. Gain informed verbal consent (if possible). 5. Ensure patient privacy. 6. Perform hand hygiene. 7. Using the Neurovascular Checklist, perform neurovascular limb assessment. 8. Notify medical team of any of the following changes indicating neurovascular compromise: Progressive pain despite adequate pain relief Pain on passive movement Parasthesia (Numbness) Tingling in affected limb Pulselessness Progressive loss of movement Pallor of limb 9. Document findings on the Neurovascular Checklist: Date and time Sensation Temperature Movement Capillary refill Pulse Colour 10. Document pain score on Pain Assessment Record. 11. Document abnormal findings and action taken in patient clinical notes. 12. In between formal observations, instruct patient to report changes such as: Pain or change in character or intensity of change Numbness and / or tingling Swelling Loss of movement Documentation Document findings on the Neurovascular Checklist: - Date and time - Sensation - Temperature - Movement - Capillary refill - Pulse -Colour Document pain score on Pain Assessment Record and any abnormal findings with action taken in patient clinical notes. Action: Identify the three major nerves of the hand and foot. Hand: -radial nerve -ulnar nerve -median nerve Foot: The Sural Nerve crosses behind the lateral malleolus (the bump on the outside portion of the ankle). Once in the foot, the Sural Nerve's name changes to the Lateral Dorsal Cutaneous Nerve, and it supplies the sensory information back to the brain concerning the outside edge of the foot, including the small toe. The Saphenous Nerve crosses behind the medial malleolus (the bump on the inside portion of the ankle). This nerve retains its name and supplies the sensory information back to the brain concerning the inside edge of the foot including the small toe. The Posterior Tibial Nerve crosses the ankle behind the medial malleolus (the bump on the inside portion of the ankle). It has three branches. Action point: Access the policy / guideline used by the staff in your clinical placement for managing a patient who is experiencing Angina. Fully discuss the key aspects of the policy / guideline within your team, and ensure you have the knowledge necessary to respond safely and effectively in a similar situation. Guideline: Nurse initiated treatment guideline for adult patients presenting to Emergency Care with chest pain associated with Acute Coronary Syndrome. Standards Step Action 1 Triage: Patient presents at triage with chest pain. Allocate triage category of 2 (as per ATS) and transfer the patient to the monitored area of EC. 2 Immediately on arrival or at least within 10 minutes of arrival – take an ECG on all chest pain patients and simultaneously carry out primary survey. 3 Once the RN has completed the ECG and primary survey, they should register the patient on the Chest Pain pathway on the EC White board, being sure to enter either the time of the ECG or the time of the initial assessment as the seen by time, which ever is earliest. TBS time = ECG/Assessment time = start of pathway. 4 The TC can assign the CP pathway seen by on behalf of the RN 5 The initial assessment is designed to include both subjective and objective data on the patient including: Subjective: Onset, location, duration, characteristics, aggravating/relieving factors, timing/treatment, pain score, allergies, PMHx, family history, smoking status identify risk factors for CVD Objective: - ECG - Connect patient to cardiac monitor- enter patient details onto central monitor - Vital signs- T, P, R, BP consider bilateral BP, SaO2, BSL, GCS - Inspect patient general appearance, colour, positioning, diaphoresis - Palpate pulse, feel skin for warmth - Insert cannula & take bloods- ¡§Myo 1¡¨ & coagulation screen (hold at laboratory if not on anticoagulants) - Appropriate alarm limits must be set according to the patients presentation and condition prior to leaving the bed space 6 If the ECG and initial assessment suggest that the patient’s chest pain is non cardiac in origin then this should be documented in the patients medical notes and the patient will not continue on the Chest pain pathway. Do not remove them from the pathway. 7 ECG to be interpreted by doctor ASAP after it has been taken, particularly if there are changes on the ECG. The doctor should sign the ECG and review the patient immediately if there are acute changes. 8. If the doctor looking after the patient is not available to review the patient and there are acute changes you must notify the CN in monitored and the EC SMO *3703. 9 If patient stable and meets criteria, commence the following interventions & medications check for allergies: - Nitrates (GTN) as per standing orders - Morphine as per standing orders - If the patient is experiencing chest pain and /or breathless or has oxygen saturations below 90% give oxygen at 5 litres per hudson mask - Aspirin as per standing orders (only if patient has not had aspirin prior to presentation) 10 outline the care plan to patient and family -Ensure patient has call bell and understands the need to report any discomfort promptly - Continuous cardiac monitoring - 15 minute vital signs - Repeat ECG at 2-3 hours, or change of rhythm or onset of pain - Ongoing pain management - Repeat Troponin I at 8 hrs post on set of initial chest pain 11 Document in patients notes their initial assessment and on going care. 12 Medical assessment as per triage category. Work with the Medical team to ensure that the patient is treated and transferred from the monitored area in a timely manner. Unless clinically indicated all patients should be transferred from the emergency assessment areas within 6 hours. 12 On discharge from Monitored Area ensure patient details are cleared from the assigned monitored bedspace otherwise ECG recordings for the wrong patient will occur. A printout of the patients observations from the monitor should be filed in the patients medical records. 13 If the patient is for the ward on telemetry or is being transferred to CCU / Step down unit they must be accommodated by nurse with defibrillator