Click Here
advertisement

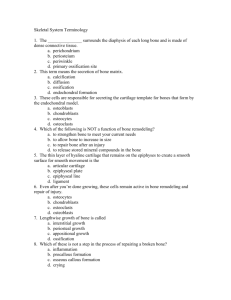
Bone Development and Growth Human Structure and Development ANHB 2212 2008 – Week 12 Avinash Bharadwaj Bone as a Connective Tissue All connective tissue is mesodermal. Undifferentiated (not specialised) cells Specialise to produce different kinds of matrix. “Osteoprogenitor” cells osteoblasts. Fibres and ground substance Osteoid Mineralisation immature (“woven”) bone. Replaced by mature, lamellar bone. Some Significant Features Unlike cartilage… Bone grows only by “apposition” : on the surface In most places… Subjected to forces as it develops and grows Needs a firm base structure to grow into In some areas, can develop in soft tissues In either case – bone formation, growth and maintenance needs blood supply! “Intramembranous” Ossification Around the developing brain – Thin “membrane” in the foetus Mesenchymal cells differentiate Osteoblasts … “Ossification centres” “Spicules” of bone Support for more osteoblasts Ossification spreads radially from the centre. Unossified tissue – sutures Foetal skull is deformable! Sutural growth and obliteration Endochondral Ossification Ossification in cartilage Cartilage withstands forces better than ‘membrane’ Muscular forces during intrauterine life Muscular and other forces during growth period Cartilage provides a mechanism for growth Cartilage can grow interstitially as well. Most bones in the body develop in this manner. Best studied with a long bone as an example. In this process cartilage is temporary. It dies and is replaced by bone. Cartilage is not coverted into bone! A Cartilage Model Mesenchymal cells differentiate chondroblasts Miniature cartilage model of bone Blood vessels invade the middle portion “Collar” of bone – subperiosteal collar Chondrocytes die in the centre Matrix calcified – acts as scaffolding Osteoblasts deposit bone matrix “Primary” centre of ossification Spread from Primary Centre Ossification spreads towards the ends Calcification of cartilage matrix death of cells New bone deposited Simultaneously, cartilage at the ends continues to grow increase in length Removal of calcified cartilage matrix Osteoclasts (“bone breaker” cells) More about their function later At birth – Shafts (diaphyses) of all long bones are bony. Postnatal Growth Bones now subject to more stresses The ends need to be ossified “Secondary” centres appear at ends form epiphyses (First such centres around the knee) However, growth must continue A plate of cartilage remains between shaft and epiphysis epiphyseal plate Cartilage grows… Replaced by bone on the surface facing the shaft “Zones” of epiphyseal plate Resting, growth, maturation, hypertrophy, calcification and death, ossification. Completion of Growth Cartilage stops growing Remaining cartilage replaced by bone Epiphysis unites with shaft Programmed appearance and fusion of epiphyses – concept of “bone age” Hormonal Control Growth hormone Before and after epiphyseal fusion Parathyroid hormone – calcium removal Other hormones Remodelling Destruction an integral part of life history of bone Osteoclasts Multinucleated large (giant) cells. Remodelling during growth Metaphysis – junction of epi- and diaphysis Shaft – increase in diameter, resorption of inner surface Flat bones Replacement of old osteons, trabeculation Altered muscular and other forces Bone Repair Fracture bleeding Blood clot – fibrous tissue Islands of cartilage Callus – fibrous + cartilage Calcification strength + death of cartilage New bone formation Woven bone – bony callus Rough surface – remodelling