R - HRET.org
advertisement
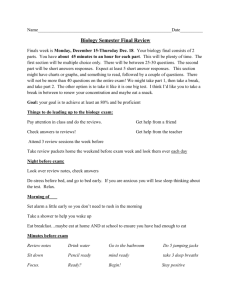
AHRQ Safety Program for Long-term Care: HAIs/CAUTI How to Avoid the Harms of Antibiotic Overuse Training Module 4 for Core Team Staff Current as of July 2015 Learning Objective Upon completion of this session, participants will be able to: • Describe what is a knee-jerk antibiotic response; • List two reasons to avoid antibiotic overuse; • Explain communication strategies that address antibiotic alternatives with providers, residents and family member; and • Train staff members about the importance of avoiding antibiotic overuse. 2 Have You Ever Heard This? Why not just give her an antibiotic? It won’t do any harm. It’s probably the urine. Needs an antibiotic. Turning to antibiotics as a knee-jerk reflex 3 Your Role in Engaging Staff in Antibiotic Stewardship • The presentation and learning activity for • Review the video and the licensed front-line staff focus on harms accompanying materials before associate with antibiotic overuse and how facilitating discussion with your frontto communicate with residents and families line staff and providers about antibiotic stewardship • Share information with all • Key messages from that training resource staff/teammates include: • Recognize and appreciate staff who ― Reasons antibiotics are not good for the resident are already proactive about antibiotic stewardship ― What antibacterial resistance is ― Communication strategies for speaking with staff members, residents and families ―CUS • Your role as leaders and teachers is vital to the prevention of CAUTIs! ―SBAR 4 Why is Knee-Jerk Antibiotic Use Bad? Reason 1 IT’S BAD FOR THE RESIDENT! • Side effects are common • Nausea, diarrhea • Allergic reactions • Antibiotic-related infections • Clostridium difficile • Candida (yeast) • Wrong diagnosis will delay treatment 5 Core Team Tip #1 • Share stories to engage staff • Overuse of antibiotics is something that needs to change • Think about changes that you may have seen in health care – Use of restraints – Universal catheterization policies • Use case studies to introduce and highlight key concepts and ideas 6 Why is Knee-Jerk Antibiotic Use Bad? Reason 2 It Leads to Bacterial Resistance! 27,000 nursing home residents have resistant infections 2 out of 3 nursing home residents receive at least one course of antibiotics annually 250,000 nursing home residents have infections 1.6 million people live in nursing homes The White House Office of the Press Secretary http://www.cdc.gov/getsmart/healthcare/learn-from-others/factsheets/nursing-homes.html FACT SHEET: Obama Administration Releases National Action Plan to Combat Antibiotic-Resistant Bacteria March 27, 2015 1. Centers for Medicare and Medicaid Services, Long Term Care Minimum Data Set, Resident profile table as of 05/02/2005. Baltimore. MD. 2. Loeb, M et.al. Antibiotic use in Ontario facilities that provide chronic care. J Gen Intern Med 2001; 16: 376-383. 3. Centers for Medicare and Medicaid Services, Long Term Care Minimum Data Set, Resident Profile Table as of 05/02/2005. Baltimore, MD. 4. Centers for Disease Control and Prevention, National Center for Health statistics, 1999 National Nursing Home Survey. Nursing Home Residents, number, percent distribution, and rate per 10,000, by age at interview, according to sex, race, and region: United States, 1999. 7 Why is Knee-Jerk Antibiotic Use Bad? Reason 2 Let’s look at the example of Klebsiella pneumonia Antibiotic Sensitive (S) or Resistant (R) Antibiotic Sensitive (S) or Resistant (R) Ampicillin S Ampicillin R Sulfatrimethoprim (Septra, Bactrim) S 30 years ago Sulfatrimethoprim (Septra, Bactrim) R Ciprofloxacin (Cipro) S 20 years ago Antibiotic Sensitive (S) or Resistant (R) Ampicillin R Sulfa-trimethoprim (Septra, Bactrim) R Ciprofloxacin (Cipro) R Cefuroxime R Nitrofurantoin (Macrodantin) R Ceftriaxone (Rocephin) R Gentamycin R Carbapenem R Today 8 Core Team Tip #3 • Reminding your team of the larger mission that is important to achieving success – Better care for individual residents – Fewer resistant infections at your facility – Saving antibiotics for the future generations 9 Communicating with Interdisciplinary Team Members, Residents and Families 10 Engaging Physicians and Clinical Leadership • Share the evidence-based information • When Do You Need An Antibiotic? Brochure • CDC: Get Smart About Antibiotics • CDC: Fact Sheet—Antibiotic Use in Nursing Homes • FDA: Know when Antibiotics Work • Use the CAUTI Criteria—NHSN Definitions Pocket Cards • Highlight why unnecessary antibiotics are bad for the resident and how it can lead to antibiotic resistance • Discuss alternatives to antibiotics • CUS to train staff on internal communication strategy 11 CUS Please use CUS Words but only when appropriate! 12 Communicating with Residents and Families • Situation • Educate residents and families regarding antibiotic use! – Highlight realistic side effects – Promote shared decision-making • Ensure that residents’ needs for pain relief and other supportive care are met • Use SBAR to improve communication – Explain the current situation • Background – Brief history with only the important information • Assessment – Summarize the facts and what you think is going on • Recommendation – Explain what actions you think should take place 13 Summary: Avoid Knee-Jerk Antibiotics • Unnecessary antibiotic use can lead to: – Resident harms – An Increase in antibiotic resistant organisms • Be aware of overuse in these situations: – Positive urine dipstick – Positive urine culture • Communication can reduce antibiotic overuse: – Include the resident and family in discussions – Use proven communication tools like CUS and SBAR 14 Stay Updated with Useful Resources 1. AHRQ Safety Program for Long-term Care: HAIs/CAUTI Project Website Login information Username: ltcsafety Password: ltcsafety 2. TeamSTEPPS® for Long-term Care 3. When Do You Need An Antibiotic? Brochure 4. CDC: Get Smart About Antibiotics 5. CDC: Fact Sheet —Antibiotic Use in Nursing Homes 6. FDA: Know When Antibiotics Work 15