Modulations of green tea, black tea and oolong tea on drug
advertisement

Effect of commercially available green and black tea beverages on
drug-metabolizing enzymes and oxidative stress in Wistar rats
Hsien-Tsung Yaoa,*, Ya-Ru Hsua, Chong-Kuei Liia,b, Ai-shen Lina, Keng-Hao Changa,
Hui-Ting Yanga,*
a
Department of Nutrition, China Medical University, 91, Hsueh-shih Road, Taichung
404, Taiwan.
b
Department of Health and Nutrition Biotechnology, Asia University, 500, Lioufeng Rd.,
Wufeng, Taichung 413, Taiwan, ROC.
*Corresponding author: Prof. Hsien-Tsung Yao. Department of Nutrition, China
Medical University, 91 Hsueh-Shih Road, Taichung 404, Taiwan. Tel: 886-4-22053366
ext. 7526. Fax: 886-4-22062891. E-mail: htyao@mail.cmu.edu.tw.
*Co-Corresponding author: Prof. Hui-Ting Yang. Department of Nutrition, China
Medical University, 91 Hsueh-Shih Road, Taichung 404, Taiwan. Tel: 886-4-22053366
ext. 7525. Fax: 886-4-22062891. E-mail: lulu0319@mail.cmu.edu.tw.
Short title: tea and drug-metabolizing enzymes
Keywords: Green tea, black tea, drug-metabolizing enzymes, oxidative stress, rats
1
Abbreviations:
AhR, Aryl hydrocarbon receptor; ARE, antioxidant response element; BT, black
tea; CYP, cytochrome P450; DME, drug-metabolizing enzymes; DR4, direct repeat
with 4 bp spacer; DRE, dioxin response elements; GT, green tea beverage; EC,
epicatechin;
EGC,
epigallocatechin;
EGCG,
epigallocatechin
gallate;
GCG,
gallocatechin gallate; GA, gallic acid; GT, green tea; GST, glutathione-S-transferase;
NQO1, NADPH:quinone oxidoreductase 1; Nrf2, nuclear factor erythroid 2-related
factor 2; PXR, pregnane X receptor; UGT, UDP-glucuronosyltransferase; GCLc/m,
glutamate cysteine ligase catalytic and modifier subunits; GSH, reduced glutathione;
GSSG, oxidized glutathione; MRP2, multidrug resistance-associated protein 2;
OATP1a1, organic anion transporting protein 1a1;ROS, reactive oxygen species; SDS,
1-chloro-2,4-dinitrobenzene, sodium dodecylsulfate
1. Introduction
Cytochrome
P450
(CYP)
enzymes
are
the
most
important
Phase
I
drug-metabolizing enzymes (DMEs) and are responsible for catalyzing the oxidative
biotransformation of many drugs, xenobiotics, and endogenous compounds. Phase II
enzymes catalyze the conjugation of glucuronate, glutathione, sulfate, or glycine to
foreign molecules (Rendic, 2002) to facilitate the elimination of electrophiles and
reactive oxygen species (ROS) generated by Phase I enzyme reactions, thereby
protecting organisms against chemical insult (Krajka-Kuz’ niak, 2007; Kondraganti et
al., 2008). Induction of Phase II enzymes, such as glutathione S-transferase (GST),
UDP-glucuronosyltransferase (UGT), and NADPH:quinone oxidoreductase 1 (NQO1),
and reduction of ROS is most pronounced in the prevention of chemical-induced tissue
injuries and carcinogenesis (Krajka-Kuz’ niak, 2007). CYP and Phase II enzymes have
been shown to be modulated by complex mixtures of phytochemicals in fruits and
2
vegetables (Rodríguez-Fragoso et al., 2011). Induction or inhibition of DMEs may
change the pharmacological activities and toxicities of drugs and carcinogens and may
also cause drug interactions (Rodríguez-Fragoso et al., 2011).
A number of nuclear receptors, including pregnane X receptor (PXR), constitutive
androstane receptor, peroxisome proliferator-activated receptor, retinoid X receptor, and
aryl hydrocarbon receptor (AhR), and transcription factors, including nuclear
factor-erythroid 2 p45-related factor 2 (Nrf2), have been demonstrated to play
important roles in the transcription of Phase I and II enzymes and Phase III transporter
genes (Xu et al., 2005). For example, AhR transcriptionally induces the expression of
human CYP1A1, CYP1A2, and CYP1B1 (Beischlag et al., 2008). AhR can be induced
by chemicals such as 2’,3’,7’,8’-tetrachlorodibenzo-p-dioxin (TCDD) (Budinsky et al.,
2010). Studies have also indicated that CYP3A as well as CYP2C are regulated by PXR
(Pascussi et al., 2000; Rana et al., 2010). Nrf2 is a transcription factor that is activated
in response to electrophiles and oxidative stress that is involved in the transcription of
some Phase II enzymes, such as GST and UGT (Aleksunes and Manautou, 2007;
Saracino and Lampe, 2007) and glutamate cysteine ligase (GCL), the rate-limiting step
in the formation of the cellular antioxidant glutathione (GSH) (Huang et al., 2013).
Green tea (GT) and black tea (BT) have been reported to act as chemoprevention
agents by modulating both Phase I CYP and Phase II conjugating enzymes (Yang and
Pan, 2012; Murugan et al., 2008). Previous studies have indicated that the polyphenols
in GT and BT induce the activation of Nrf2 (Mann et al., 2007; Patel and Maru, 2008;
Han et al., 2012) and inhibit AhR-regulated genes (e.g., CYP1A1) and the binding of
toxic chemicals to the AhR (Fukuda et al., 2004; Fukuda et al., 2005; Han et al., 2012).
Rats treated with GT or BT extracts have been reported to have increased hepatic CYP
1A2 and UGT activities (Bu-Abbas et al., 1999; Nikaidou et al., 2005). However, GT
was also reported to have no effect on hepatic CYP1A2 and CYP3A activities in rats
3
(Niwattisaiwong et al., 2004). Inhibition of CYP3A and 2E1 in liver by GT catechins
has also been reported in mice (Chen et al., 2009). Furthermore, an increase of GST and
NQO1 activities in both liver and lungs was observed in mice treated with BT
polyphenols (Patel and Maru, 2008). On the other hand, mice that were treated with
decaffeinated GT and BT extracts were found to have lower CYP enzyme activities in
the lungs than control mice (Shi et al., 1994). These results indicate that the effects of
tea or tea extracts on DMEs in tissues differ depending on the experimental conditions.
Although the effects of various tea components on the regulation of DMEs are not
consistent, these results do indicate that GT and BT consumption may play an
important role in modulating DMEs and redox status.
Recently, commercially available tea beverages have become more popular
worldwide. Sugar is supplemented to various tea beverages to reduce the bitterness of
taste and to provide an energy source. To date, little or no data on the effects of
sugar-containing tea beverages on DMEs and oxidative stress have been reported. In
this study, therefore, the effects of consumption of commercially available GT and BT
on DMEs and oxidative stress in rats were investigated. The possible regulation of PXR,
AhR, and Nrf2 in liver by the GT and BT was also evaluated.
4
2. Materials and methods
2.1. Tea beverages
GT and BT (Manufactured by Uni-President Enterprises Corp, Taiwan) were obtained
commercially. The concentrations of ascorbate, caffeine, gallic acid, and catechins in the tea
beverages were determined by a high-performance liquid chromatography (HPLC) method
reported previously (Wu et al., 2011). The sucrose concentration in the tea beverages was
determined with a commercial assay kit (Megazyme, Bray, Ireland). Two consecutive batches
of beverages were used for this experiment. The concentrations of the major constituents in
the tea beverages are shown in Table 1.
2.2. Chemicals
Epicatechin
(EC),
epigallocatechin
(EGC),
epigallocatechin-gallate
(EGCG),
epicatechin-gallate (ECG), gallocatechin gallate (GCG), gallic acid (GA), caffeine, formic
acid, ammonium acetate, testosterone, ethoxyresorufin, methoxyresorufin, pentoxyresorufin,
resorufin, p-nitrophenol, 4-nitrocatechol, NADPH, glutathione, glutathione reductase,
1-chloro-2,4-dinitrobenzene, sodium dodecylsulfate (SDS), cytochrome c, heparin, Ponceau S,
phenacetin, diclofenac (sodium salt), chlorzoxazone, 1,1,3,3-tetraethoxypropan, thiobarbituric
acid, and pyrogallol were obtained from Sigma (St. Louis, MO, USA). 4-Hydroxydiclofenac,
6-hydroxychlorzoxazone, midazolam, 6--hydroxytestosterone, and 1-hydroxymidazolam
were purchased from Ultrafine Chemicals (Manchester, UK). All other chemicals and reagents
were of analytical grade and were obtained commercially.
2.3. Animals and treatments
Eighteen male Wistar rats, weighing approximately 150 g (4 weeks old) each, were
obtained from BioLASCO, Taiwan (Ilan, Taiwan). During the adaptation period, the rats were
fed a pelleted diet for 1 week. Then the animals were randomly divided into three groups with
six rats in each group. The animals in the control group were given a standard pelleted diet
5
with tap water. The animals in the other two groups were given the same diet with GT or BT.
The tea beverages were the sole source of drinking fluid in the tea groups. All drinking fluid
was given to rats in plastic bottles, which were replaced daily with fresh water or tea.
Rats were housed in individual plastic cages in a room kept at 23 ± 1 °C and 60 ± 5%
relative humidity with a 12-h light and dark cycle. Food and drinking fluid were available ad
libitum for 5 weeks. Body weight and food intake were determined every week. This study
was approved by the Animal Center Management Committee of China Medical University.
The animals were maintained in accordance with the guidelines for the care and use of
laboratory animals as issued by the Animal Center of the National Science Council, Taiwan.
2.4. Collection of blood and tissue samples
At the end of the 5-week feeding period, animals were fasted overnight (12 h) before
being killed by exsanguination via the abdominal aorta while under carbon dioxide (70%/30%,
CO2/O2) anesthesia. Heparin was used as the anticoagulant. Plasma was separated from the
blood by centrifugation (1750 ×g) at 4oC for 20 min and stored at -20 oC. Plasma alanine
aminotransferase was determined by using a commercial kit (Randox Laboratories, Antrum,
UK) within 2 weeks. The liver and lungs from each animal were excised, weighed, and stored
at -80oC.
2.5.
Determination of DME activities
The frozen livers and lungs were thawed and the same portion of each liver or lung
sample was used to prepare microsomes. Each gram of liver or lung was then homogenized
with 4 mL of ice-cold 0.1 M phosphate buffer (pH 7.4) containing 1 mM EDTA. The
homogenates were centrifuged at 10,000 ×g for 15 min at 4oC. The supernatant was then
re-centrifuged at 105,000 ×g for 1 h at 4oC. The resulting microsomal pellet was suspended in
0.25 M sucrose solution containing 1 mM EDTA and was stored at -80oC until use.
The microsomal protein concentration was determined by using a BCA protein assay kit
(Pierce, Rockford, IL). The contents of total CYP and cytochrome b5 in the microsomes were
6
quantified according to the method of Omura and Sato (1964). NADPH-CYP reductase
activity was measured according to the procedure of Phillips and Langdon (1962) by using
cytochrome c as the substrate. A number of substrates were used to determine the activity of
each specific CYP enzyme as reported previously (Yao et al., 2011). Ethoxyresorufin (2 M),
methoxyresorufin (5 M), and pentoxyresorufin (5 M) were respectively used as the probe
substrates for ethoxyresorufin O-deethylation (CYP1A1), methoxyresorufin O-demethylation
(CYP1A2),
and
pentoxyresorufin
O-depentylation
(CYP2B).
Diclofenac
(4
M),
dextromethorphen (5 M), p-nitrophenol (50 M), testosterone (60 M), midazolam (2.5 M),
and lauric acid (100 M) were respectively used as the probe substrates for diclofenac
4-hydroxylation (CYP2C), dextromethorphen O-demethylation (CYP2D), p-nitrophenol
6-hydroxylation
(CYP2E1),
6β-hydroxylation
testosterone
(CYP3A),
midazolam
1-hydroxylation (CYP3A), and lauric acid 12-hydroxylation (CYP4A). Microsomal proteins
(0.2 mg/mL) and the incubation time (15 min) were the same for all metabolic reactions
except for the midazolam 1-hydroxylation (CYP3A) reaction, which was incubated for 5 min.
The metabolites of each CYP enzyme reaction were determined by HPLC/mass spectrometry
(MS) methods as reported previously (Yao et al., 2008). Enzyme activities were expressed as
picomoles of metabolite formed/min/mg protein.
The microsomal UGT activity was determined by using p-nitrophenol as the substrate
where the rate of formation of p-nitrophenol glucuronic acid was measured by HPLC
(Mennier and Verbeeck, 1999).
2.6. Determinations
of
lipid
peroxide,
reactive
oxygen
species
and
glutathione
concentrations, and antioxidant enzyme activities
Liver and lung homogenates were prepared by homogenizing each gram of tissue with 9
mL of ice-cold 1.15% KCl to obtain a 10% (w/v) homogenate. The homogenate was then
centrifuged at 10,000 ×g for 15 min at 4oC. The resulting supernatant was used to determine
7
the lipid peroxide and GSH contents and GST and NQO1 activities. The lipid peroxide level
in tissue homogenates was determined by measuring thiobarbituric acid–reactive substance
(TBARS) values according to the method of Uehiyama and Mihara (1978). The contents of
reduced (GSH) and oxidized (GSSG) glutathione in the liver and lung homogenates were
determined by LC/MS (Guan et al., 2003). GST (Habig and Jakoby, 1981) and NQO1
(Tsvetkov et al., 2005) activities were determined spectrophotometrically. Glutathione
peroxidase activity was determined spectrophotometrically according to the method of
Mohandas et al. (1984). ROS production was measured according to the method of Ali et al.
(1992) by determining fluorescent product of dichlorofluorescein.
2.7. Western blot analysis
Proteins in liver microsomes (CYP1A1 and CYP1A2, 12.5 μg; CYP2C11, 3A1, and 3A2,
4 μg; CYP2E1, 10 μg) or liver homogenates (GCL catalytic and modifier subunits [GCLc and
GCLm]; 10 μg) were separated by 10% SDS-PAGE and transferred to nitrocellulose
membranes. Subsequently, the membranes were blocked with 5% skim milk in PBST buffer
(137 mM NaCl, 2.7 mM KCl, 10 mM Na2HPO4, 2 mM KH2PO4, and 0.1% Tween-20) for 1 h
at room temperature and were then hybridized with primary antibodies against CYP enzymes
and GCLc/m (Abcam, Cambridge) with gentle agitation overnight at 4oC. After two washings
with PBST, the membranes were incubated with a horseradish peroxidase–conjugated
secondary antibody from Abcam for 1 h at room temperature. Immunoreactive bands were
detected by using enhanced chemiluminescence (Western Lightning Chemiluminescence
Reagent; Perkin–Elmer, Boston, MA). Densitometric measurements of the bands were made
by using a luminescent image analyzer (FUJIFILM LAS-4000, Japan) and the bands were
quantitated with an ImageGauge (FUJIFILM). Equal loading across the lanes was confirmed
by staining the blot with Ponceau S solution.
2.8. Determination of caffeine concentrations in plasma and liver
The 10% (w/v) liver homogenates in 1.15% KCl were prepared as described above.
8
An aliquot (100 L) of plasma or liver homogenate was mixed with 200 L of acetonitrile
(1:2, v/v), mixed by vortexing, and then centrifuged at 10,000 ×g for 20 min. The supernatant
was transferred to a clean tube and then a 10-μL aliquot of the supernatant was injected into
the LC/MS system for analysis (Lad, 2010).
2.9. Determination of triglyceride and cholesterol contents in liver
Lipids were extracted from liver by the method of Folch et al. (1957) and solubilized in Triton
X-100 according to the method of Carlson and Goldford (1979). The hepatic total cholesterol
and triglyceride contents were assayed enzymatically by using kits purchased from Audit
Diagnostics (Cork, Ireland).
2.10.Extraction of nuclear proteins and electrophoretic mobility shift assay (EMSA)
Liver nuclear proteins were extracted according to the method of Tian et al. (2004) with
some modifications. Briefly, 50 mg liver was homogenized (1:18, w/v) in an ice-cold
hypotonic buffer containing 10 mM HEPES, 10 mM KCl, 1 mM MgCl2, 0.1 mM EDTA, 0.5
mM dithiothreitol, 0.5 mM PMSF, 4 μg/mL leupeptin, and 20 μg/mL aprotinin, pH 7.9. The
homogenate was placed in an ice bath for 15 min and then centrifuged at 600 ×g for 10 min.
The supernatant was mixed with 100 μL of 10% (v/v) Nonidet P-40 and kept in the ice bath
for another 10 min. The supernatant was then centrifuged at 5000 ×g for 5 min. The crude
nuclei pellet was resuspended in 100 μL of a hypertonic buffer containing 10 mM HEPES,
400 mM KCl, 1 mM MgCl2, 0.1 mM EDTA, 0.5 mM dithiothreitol, 0.5 mM PMSF, 4 μg/mL
leupeptin, 20 μg/mL aprotinin, and 25% glycerol at 4oC for 45 min. Nuclear proteins were
then collected by centrifugation at 12,000 ×g for 15 min. EMSA was performed with the
LightShift Chemiluminescent EMSA kit (Pierce, Rockford, IL) according to the method of
Yang et al. (2001). The synthetic biotin-labeled double-stranded oligonucleotides used were as
follows: antioxidant response element (ARE), 5’-AACCATGACACAGCATAAAA-3'; dioxin
response elements (DRE), 5’-GATCCGGAGTTGCGTGAGAAGAGCCA-3’; direct repeat
with
4 bp spacer
(DR4), 5’-AGCTTCAGGTCACAGGAGGTCAGAGAG-3’.
9
Four
micrograms
of
nuclear
protein,
poly(dI-dC),
and
biotin-labeled
double-stranded
oligonucleotide were mixed with the binding buffer to a final volume of 20 μL and were
incubated at room temperature for 30 min. Unlabeled double-stranded ARE, DR4, and DRE
oligonucleotide and mutant double-stranded oligonucleotide were used to confirm the binding
specificity of nuclear proteins. The nuclear protein-DNA complex was separated by
electrophoresis on a 6% Tris-boric acid-EDTA polyacrylamide gel and was then
electrotransferred to a Hybond-N+ nylon membrane (GE Healthcare, Buckinghamshire). The
membrane was incubated with streptavidin-horseradish peroxidase, and the nuclear
protein-DNA bands were developed with an enhanced chemiluminescence kit (Thermo).2.11.
Statistical evaluation
Statistical differences among groups were calculated by using one-way ANOVA (SAS
Institute, Cary, NC, USA) and were considered to be significant at p<0.05 as determined by
Duncan's new multiple-range test.
10
3. Results
3.1. Constituents of the GT and BT
As shown in Table 1, the GT had higher contents of catechins (EGC, EGCG, EC,
ECG, GCG), ascorbic acid, and total phenols than did the BT. On the other hand, the
gallic acid content was higher in the BT than in the GT. The contents of caffeine and
sucrose were comparable in the two beverages.
3.2. Effect on body weight and tissue weight
After the 5-week feeding period, consumption of the GT and BT resulted in an
increase (p<0.05) in body weight (Control: 340.3±16.1 g; GT: 369.2±13.0 g; BT:
379.5±30.7 g) and relative liver weight (g/100 g body weight; Control: 2.9±0.2; GT:
3.1±0.1; BT: 3.5±0.2) compared with the values in the control group. A significant
increase (p<0.05) in fluid consumption was also noted in rats given the GT or BT
compared with the water control (Control: 22.8±2.5 mL/day/rat; GT: 44.8±7.4
mL/day/rat; BT: 54.0±8.0 mL/day/rat). However, tea consumption did not affect daily
food intake (Control: 25.0±1.0 g; GT: 25.1±1.2 g; BT: 25.5± 1.0 g). Furthermore,
consumption of the GT or BT did not cause any change in the plasma alanine
aminotransaminase level (data not shown).
3.3. Effect on DME activities
The total CYP and cytochrome b5 contents and the DME activities in rat liver
microsomes after 5 weeks of GT or BT intake are shown in Table 2. A statistically
significant decrease in cytochrome b5 content was observed in rats treated with the BT
(p<0.05).
Furthermore,
diclofenac
4-hydroxylation
(CYP2C),
testosterone
6β-hydroxylation (CYP3A), midazolam 1-hydroxylation (CYP3A), and nitrophenol
6-hydroxylation (CYP2E1) were significantly decreased (p<0.05) in the liver
microsomes of rats treated with both GT and BT. These results indicate that GT and BT
consumption may reduce the metabolism of xenobiotics catalyzed by CYP3A, CYP2C,
11
and CYP 2E1 in liver. In contrast, an increase of methoxyresorufin O-demethylation
(CYP1A2) was found in rats treated with both GT and BT (p< 0.05). An increase of
ethoxyresorufin O-deethylation (CYP1A1) activity was observed in rats treated with the
GT (p< 0.05) but not with the BT beverage. Neither beverage had a significant effect
(p> 0.05) on the activities of pentoxyresorufin O-depentylation (CYP2B),
dextromethorphen O-deethylation (CYP2D), and lauric acid 12-hydroxylation
(CYP4A).
Rats treated with the GT or BT showed an increase in UGT activity (p<
0.05) but showed no significant difference in GST or NQO1 activities compared with
that in the rats given water. The GT and BT also had no significant effects on
ethoxyresorufin O-deethylation (CYP 1A1), methoxyresorufin O-demethylation (CYP
1A2), or nitrophenol 6-hydroxylation (CYP2E1) activities in lung tissues (Table 3).
However, higher pulmonary UGT activity and lower GST activity were observed (p<
0.05).
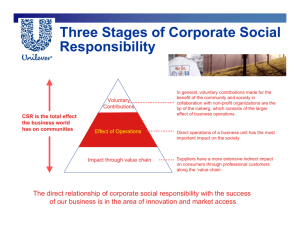
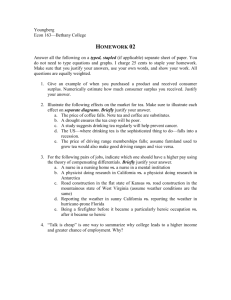
Figure 1 shows the immunoblots of CYP proteins in liver microsomes. Similar to
the changes in CYP enzyme activities, BT and GT consumption decreased CYP 2C11,
2E1, 3A1, and 3A2 protein expression and increased CYP1A2 protein expression in
liver tissues. Only rats fed the GT showed increased CYP1A1 expression in liver.
3.4. Effect on GSH and ROS contents, antioxidant enzyme activities, and lipid
peroxidation
As shown in Table 4, after 5 weeks of treatment, GT and BT increased the GSH
level and GSH/GSSG ratio in liver and lungs (p< 0.05) and decreased the GSSG level
in liver (Table 4). An increase in hepatic GSH peroxidase activity was observed in rats
treated with the GT (p< 0.05) but not the BT. Consumption of both tea beverages
reduced GSH reductase activity in lungs (p< 0.05) but not in liver. Neither tea beverage
caused a significant change in TBARS contents in liver (p< 0.05). However, a lower
TBARS level was found in the lungs of rats treated with the GT (p< 0.05). Both tea
12
beverages resulted in a lower ROS level in liver (p< 0.05). By contrast, in lungs, only
the GT resulted in a lower ROS level (p< 0.05).
3.5. Effect on hepatic lipids content
The GT and BT had no significant effects on hepatic cholesterol or triglyceride
levels in rats (data not shown).
3.6. Plasma and liver caffeine levels
The caffeine levels in plasma of rats treated with the GT and BT were 2.3±2.0 and
3.6±4.1 g/ml, respectively. The corresponding values in liver were 367±241 and
512±464 g/g, respectively.
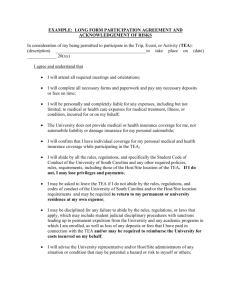
3.7. Effect on GCLc and GCLm protein expression
As shown in Figure 2, rats treated with both tea beverages showed increased GCLc
and GCLm protein expression in liver. In the lungs, both tea beverages increased GCLc
protein expression but did not significantly affect GCLm protein expression.
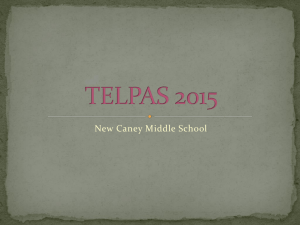
3.8. Effect on DNA binding activity of nuclear Nrf2, PXR, and AhR
We also examined the effect of tea consumption on the binding activity of nuclear
transcription factors to DNA. As shown in Figure 3, rats treated with both tea beverages
showed increased binding activity of nuclear Nrf2 to the ARE consensus sequences (Fig.
3A). Similarly, rats treated with the GT but not the BT showed increased binding
activity of AhR to the DRE consensus sequences (Fig. 3B). Rats treated with both tea
beverages showed decreased binding activity of PXR to the DR4 consensus sequences
(Fig. 3C).
13
4. Discussion
In this study, our results show that consumption of BT and GT by rats changed
the activity of DMEs and increased glutathione levels in liver and lungs. Consumption
of both tea beverages led to decreased hepatic PXR and increased Nrf2 binding to DNA.
In addition, consumption of the GT increased the binding activity of AhR to the DRE.
These results suggest that consumption of GT and BT by rats modulates the metabolism
of drugs and chemical carcinogens and reduces oxidative stress in liver and lungs.
Many phytochemicals have been shown to prevent chemical-induced tissue
damage and carcinogenesis in animals, mainly as a result of the modulation of DMEs
after their administration (Kondraganti et al., 2008; Yang and Pan, 2012). In the present
study, significantly higher CYP1A2 activity in liver was noted in rats treated with GT
and BT. It has been reported that caffeine, but not the polyphenols, in GT or BT extract
may contribute to the induction of CYP1A2 activity (Bu-Abbas et al., 1999; Nikaidou
et al., 2005). In this study, the caffeine concentration in plasma (GT: 2.3±2.0 g/mL;
BT: 3.6±4.1 g/mL) was higher than the level (~0.2 g/mL) that was reported to induce
hepatic CYP1A2 (Chen et al., 1996). Therefore, the induction of CYP1A2 activity and
protein expression after BT and GT consumption might have been due to the caffeine in
the tea beverages. We also observed an increase of UGT activity in the liver and lungs
of rats treated with tea beverages in the present study. This result agrees with the
observation of Srinivasan et al (2008) showing that rats treated with tea catechins had
higher UGT activity in liver. Because UGT has been implicated as an important
detoxifying enzyme that catalyzes the conjugation of the metabolites of major tobacco
carcinogens, such as benzo[a]pyrene, to facilitate their excretion (Zheng et al., 2002),
the consumption of tea beverages may aid in the detoxification of smoking.
GSH, a vital antioxidant in cells, protects tissues against oxidative stress,
14
inflammation, and injury. GSH acts as a radical-scavenging antioxidant and also is the
preferred substrate for several enzymes in drug metabolism and antioxidant defense (Lu,
2009). GSH biosynthesis is completed in two steps that are catalyzed by GCL and GSH
synthetase. GCL is a heterodimeric holoenzyme composed of the GCLc and GCLm
subunits and is the rate-limiting enzyme in GSH biosynthesis (Franklin et al., 2009). In
the present study, the GT and BT induced both GCLc and GCLm protein expression in
rat liver. Accompanied by the increase in GCLc and GCLm protein expression, a higher
GSH level was observed in rats treated with the GT and BT, thus indicating the
induction of GSH synthesis. Furthermore, higher GSH/GSSG ratios and UGT activity
in liver and lungs were observed after GT and BT treatment. The higher GSH level and
phase II detoxification enzyme activity (e.g., UGT) will, in turn, enhance the protection
of liver and lung tissues against chemical insult. Because lower TBARS and ROS levels
were observed only in the lungs of rats treated with the GT, our results suggest that the
GT was more effective for reducing oxidative stress than the BT in the lungs.
Phytochemicals are known to be potent modulators of the transcription of Phase I
and II DMEs and the Phase III transporter genes (Xu et al., 2005). For instance,
andrographolide induces rat hepatic CYP2C6/11, CYP1A1/2, and CYP3A1/2 protein
expression by increasing PXR and AhR binding activity to DNA (Chen et al., 2013).
Liquiritigenin stimulates Nrf2 translocation into the nucleus (Kim et al., 2010) and
enhances the expression of not only hepatic phase II enzymes (e.g., UGT and GST) but
also the canalicular efflux transporters (e.g., multidrug resistance-associated protein 2,
or MRP2) and basolateral uptake transporters (e.g., organic anion transporting protein
1a1, or OATP1a1) (Kim et al., 2009). Our results revealed up-regulated GCLc/m
protein expression in the liver of rats treated with the GT and BT, and this was related
to the increase of DNA binding activity of Nrf2 (Fig. 3A). Tea polyphenols are known
15
to play a role in the induction of Nrf2 activation, which in turn triggers ARE-driven
transcription of GCL (Huang et al., 2013). Therefore, the increased DNA binding
activity of Nrf2 after the consumption of both tea beverages might be attributed to the
increased GSH level in the liver. In line with previous studies, our results showed
induction of CYP1A2 activity by GT and BT in liver of rats (Niwattisaiwong et al.,
2004; Jang et al., 2005).
Other CYP enzymes such as CYP3A and CYP2E1 were suppressed by the GT
(Park et al., 2009; Chen et al., 1996). Regarding the changes in CYP protein expression,
the consistent decrease in the expression of CYP3A and CYP2C proteins and the DNA
binding activity of PXR by the consumption of BT and GT suggest that both tea
beverages may suppress PXR activation (Fig. 3C). The suppressed PXR activation, then,
results in lower protein expression and activity of CYP3A and CYP2C.
In contrast with the decrease in PXR activation and CYP3A and CYP2C protein
expression and activity, GT administration increased the DNA binding activity of AhR
(Fig. 3B). Activation of AhR explains, at least in part, the induction of hepatic CYP1A1
and CYP1A2 protein expression and activity by the GT. It is interesting to note that
consumption of the BT induced hepatic CYP1A2 protein expression and activity.
However, the BT had little or no effect on the DNA binding activity of AhR. Taken
together, these results suggest that the modulation of DME activity by tea beverages is
likely to work at the transcriptional stage. Moreover, the modulation of DME gene
transcription by tea beverages may be CYP isozyme- and beverage-specific.
The increased fluid intake (approximately 2-2.5 folds) of the rats in the GT and
BT treatment groups, compared with that of the control group in which tap water was
given, might have been due to the sweetness of the drinks. Although the sucrose in the
tea beverages may increase lipid synthesis in liver (Roncal-Jimenez et al., 2011), the
16
results of our study showed no increase of liver triglyceride or cholesterol levels in the
treated rats compared with the controls. The lipid-lowering effects of tea catechins,
particularly EGCG, may have played a role in this result (Koo and Noh, 2007).
In summary, the present study showed that consumption of GT and BT by rats
reduced CYP2C, 2E1, and 3A activities and protein expression and induced CYP1A1
and/or CYP1A2 activity and protein expression in liver. GT and BT treatment also
increased UGT activity and the GSH level in both liver and lungs. Thus, GT and BT
may act as chemopreventive agents. Also, the GT was more effective for reducing
oxidative stress in lungs than was the BT. The modulation of DMEs by GT and BT is
likely to work at the transcriptional stage. Given that tea beverages are becoming more
popular worldwide, their possible interactions with drugs or toxic compounds should be
taken into account.
17
References
Ali, S. F., LeBel, C. P., and Bondy, S. C. (1992). Reactive oxygen species formation as
a biomarker of methylmercury and trimethyltin neurotoxicity. Neurotoxicology 13,
637-648.
Aleksunes, L.M., Manautou, J.E. 2007. Emerging role of Nrf2 in protecting against
hepatic and gastrointestinal disease. Toxicol Pathol. 35, 459–473.
Beischlag, T.V., Luis Morales, J., Hollingshead, B.D., Perdew, G.H. 2008. The aryl
hydrocarbon receptor complex and the control of gene expression. Crit. Rev.
Eukaryot. Gene Expr. 18, 207-250.
Bu-Abbas, A., Copeland, E., Clifford, M.N., Walker, R., Ioannides, Costas. 1997.
Fractionation of green tea extracts: correlation of antimutagenic effect with
flavanol content. J. Sci. Food Agric. 75: 453-462.
Budinsky, R. A., LeCluyse, E.L., Ferguson, S. S., Rowlands, J. C., Simon, T. Human
and rat primary hepatocyte CYP1A1 and 1A2 induction with
2,3,7,8-tetrachlorodibenzo-p-dioxin, 2,3,7,8-tetrachlorodibenzofuran, and
2,3,4,7,8-pentachlorodibenzofuran. Toxicol Sci. 2010. 118, 224-235.
Carlson, E., Goldford, S. 1979. A sensitive enzymatic method for determination of free
and esterified tissue cholesterol. Clin. Chim. Acta.
79, 575–582.
Chen, H.W., Huang, C.S., Liu, P.F., Li, C.C., Chen, C.T., Liu, C.T., Chiang, J.R., Yao,
H.T., Lii, C.K. Andrographis paniculata extract and andrographolide modulate the
hepatic drug metabolism system and plasma tolbutamide concentrations in rats.
Evid Based Complement Alternat Med. 2013;:982689.
Chen, L., Bondoc, F.Y. , Lee, M.J., Hussin, A.H., Thomas, P.E., Yang, C.S. 1996.
Caffeine induces cytochrome P4501A2: induction of CYP1A2 by tea in rats. Drug
Metab Dispos. 24, 529-533.
Chen, X., Sun, C.K., Han, G.Z., Peng, J.Y., Li, Y., Liu, Y.X., Lv, Y.Y., Liu, K.X., Zhou,
Q., Sun, H.J. 2009. Protective effect of tea polyphenols against
paracetamol-induced hepatotoxicity in mice is significantly correlated with
cytochrome P450 suppression. World. J. Gastroenterol. 15, 1829-1835.
18
Franklin, C.C., Backos, D.S., Mohar, I., White, C.C., Forman, H.J., Kavanagh, T.J.
2009. Structure, function, and post-translational regulation of the catalytic and
modifier subunits of glutamate cysteine ligase. Mol Aspects Med. 30, 86–98.
Folch, J., Lees, M., Sloane-Stanley, G.M. 1957. A purification of total lipid from
animal tissue. J. Biol. Chem. 226, 497–509.
Fukuda, I., Sakane, I., Yabushita, Y., Kodoi, R., Nishiumi, S., Kakuda, T., Sawamura, S.
Kanazawa, K. Ashida, H. 2004. Pigments in green tea leaves (Camellia sinensis)
suppress transformation of the aryl hydrocarbon receptor induced by dioxin. J.
Agric. Food Chem. 52, 2499-2506.
Fukuda, I., Sakane, I., Yabushita, Y., Sawamura, S., Kanazawa, K., Ashida, H. 2005.
Black tea theaflavins suppress dioxin-induced transformation of the aryl
hydrocarbon receptor. Biosci. Biotechnol. Biochem. 69, 883-890.
Guan, X., Hoffman, B., Dwivedi, C., Matthees, D.P. 2003. A simultaneous liquid
chromatography/mass spectrometric assay of glutathione, cysteine, homocysteine
and their disulfides in biological samples. J. Pharm. Biomed. Anal. 31, 251–261.
Habig, W.H., Jakoby, W.B. 1981. Assays for differentiation of glutathione
S-transferases. Methods Enzymol. 77, 398–405.
Han, S.G., Han, S.S., Toborek, M., Hennig, B. 2012. EGCG protects endothelial cells
against PCB 126-induced inflammation through inhibition of AhR and induction
of Nrf2-regulated genes. Toxicol. Appl. Pharmacol. 261, 181-188.
Huang, C.S., Lii, C.K., Lin, A.H., Yeh, Y.W., Yao, H.T., Li, C.C., Wang, T.S., Chen, H.
W. 2013. Protection by chrysin, apigenin, and luteolin against oxidative stress is
mediated by the Nrf2-dependent up-regulation of heme oxygenase 1 and glutamate
cysteine ligase in rat primary hepatocytes. Arch Toxicol. 87, 167-178.
Jang, E. H., Choi, J.Y., Park, C. S. et al. 2005. Effects of green tea extract
administration on the pharmacokinetics of clozapine in rats. J. Pharm. Pharmacol.
57, 311-316.
19
Kim, Y.W., Kang, H.E., Lee, M.G., Hwang, S.J., Kim, S.C., Lee, C.H., Kim, S.G. 2009.
Liquiritigenin, a flavonoid aglycone from licorice, has a choleretic effect and the
ability to induce hepatic transporters and phase-II enzymes. Am. J. Physiol.
Gastrointest. Liver Physiol., 296, G372-G381.
Kim, Y.W., Kim, Y.M., Yang, Y.M., Kay, H.Y., Kim, W.D., Lee, J.W., Hwang, S.J.
Kim, S.G. 2010. Inhibition of LXRα-dependent steatosis and oxidative injury by
liquiritigenin, a licorice flavonoid, as mediated with Nrf2 activation. Antioxid.
Redox Signal. 14, 733-745.
Kondraganti, S.R., Jiang, W., Jaiswal, A.K., Moorthy, B. 2008. Persistent induction of
hepatic and pulmonary phase II enzymes by 3-methylcholanthrene in rats. Toxicol.
Sci. 102, 337–342.
Koo, S.I., Noh, S.K. 2007. Green tea as inhibitor of the intestinal absorption of lipids:
potential mechanism for its lipid-lowering effect. J. Nutr Biochem. 18, 179-183.
Krajka-Kuz’ niak, V. 2007. Induction of phase II enzymes as a strategy in the
chemoprevention of cancer and other degenerative diseases. Postepy Hig. Med.
Dosw. 61, 627–638.
Lad, R. 2010. Validation of individual quantitative methods for determination of
cytochrome P450 probe substrates in human dried blood spots with HPLC-MS/MS.
Bioanalysis. 2, 1849-1861.
Lu, S.C. 2009. Regulation of glutathione synthesis. Mol Aspects Med. 30, 42–59.
Mann, G.E., Rowlands, D.J., Li, F.Y., de Winter, P., Siow, R.C. 2007. Activation of
endothelial nitric oxide synthase by dietary isoflavones: role of NO in
Nrf2-mediated antioxidant gene expression. Cardiovasc Res. 75, 261-274.
Mennier, C.J., Verbeeck, R.K. 1999. Glucuronidation of R- and S-ketoprofen,
acetaminophen, and diflunisal by microsomes of adjuvant induced arthritic rats.
Drug Metab. Dispos. 27, 26–31.
Mohandas, J., Marshall, J.J., Duggin, G.G., Horvath, J.S., Tiller, D.J. 1984. Low
activities of glutathione-related enzymes as factors in the genesis of urinary
20
bladder cancer. Cancer Res. 44, 5086–5091.
Murugan RS, Uchida K, Hara Y, Nagini S. 2008. Black tea polyphenols modulate
xenobiotic-metabolizing enzymes, oxidative stress and adduct formation in a rat
hepatocarcinogenesis model. Free Radic Res. 42,873-884.
Nikaidou, S., Ishizuka, M., Maeda, Y., Hara, Y., Kazusaka, A., Fujita, S. 2005. Effect of
components of green tea extracts, caffeine and catechins on hepatic drug
metabolizing enzyme activities and mutagenic transformation of carcinogens. Jpn.
J. Vet Res. 52, 185-192.
Niwattisaiwong, N., Luo, X. X.,Coville, P. F., Wanwimolruk, S. 2004. Effects of
Chinese, Japanese and Western tea on hepatic P450 enzyme activities in rats. Drug
Metabol Drug Interact. 20, 43-56.
Omura, T., Sato, R. 1964. The carbon monoxide-binding pigment of liver microsomes.
l. Evidence for its hemeprotein nature. J. Biol. Chem. 239, 2370– 2379.
Park, D., Jeon, J. H., Shin, S., Joo, S. S., Kang, D. H., Moon, S. H., Jang, M. J., Cho,
Y. M., Kim, J. W., Ji, H. J., Ahn, B., Oh, K.W., Kim, Y. B. 2009. Green tea extract
increases cyclophosphamide-induced teratogenesis by modulating the expression of
cytochrome P-450 mRNA. Reprod Toxicol. 27, 79-84.
Pascussi, J.M., Drocourt, L., Fabre, J.M., Maurel, P., Vilarem, M.J. 2000.
Dexamethasone induces pregnane X receptor and retinoid X receptor-alpha
expression in human hepatocytes: synergistic increase of CYP3A4 induction by
pregnane X receptor activators. Mol Pharmacol. 58, 361-372.
Patel, R., Maru, G. 2008. Polymeric black tea polyphenols induce phase II enzymes via
Nrf2 in mouse liver and lungs. Free Radic Biol Med. 44, 1897-1911.
Phillips, A.H., Langdon, R.G. 1962. Hepatic triphosphopyridine nucleotide cytochrome
c reductase: isolation, characterization, and kinetic studies. J. Biol. Chem. 237,
2652-2660.
Rana, R., Chen, Y., Ferguson, S.S., Kissling, G..E., Surapureddi, S., Goldstein, J.A.
2010. Hepatocyte nuclear factor 4{alpha} regulates rifampicin-mediated induction
of CYP2C genes in primary cultures of human hepatocytes. Drug Metab Dispos.
21
38, 591-599.
Rendic, S. 2002. Summary of information on human CYP enzymes: human P450
metabolism data. Drug Metab. Rev. 34, 83–448.
Rodríguez-Fragoso, L., Martínez-Arismendi, J.L., Orozco-Bustos, D., Reyes-Esparza,
J., Torres, E., Burchiel, S.W. 2011. Potential risks resulting from
fruit/vegetable-drug interactions: effects on drug-metabolizing enzymes and drug
transporters. J. Food Sci. 76,112-124.
Roncal-Jimenez, C.A., Lanaspa, M.A., Rivard, C.J., Nakagawa, T., Sanchez-Lozada, L.
G., Jalal, D., Andres-Hernando, A., Tanabe, K., Madero, M., Li, N., Cicerchi, C.,
Mc Fann, K., Sautin, Y.Y., Johnson, R.J. 2011. Sucrose induces fatty liver and
pancreatic inflammation in male breeder rats independent of excess energy intake.
Metabolism. 60, 1259-1270.
Saracino, M.R., Lampe, J.W. 2007. Phytochemical regulation of
UDP-glucuronosyltransferases: implications for cancer prevention. Nutr Cancer.
59, 121-141.
Shi, S.T., Wang, Z.Y., Smith, T.J., Hong, J.Y., Chen, W.F., Ho, C.T. , Yang, C.S. 1994.
Effects of green tea and black tea on
4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone bioactivation, DNA methylation,
and lung tumorigenesis in A/J mice. Cancer Res. 54, 4641-4647.
Srinivasan, P., Suchalatha, S., Babu, P. V., Devi, R.S., Narayan, S., Sabitha, K.E.,
Shyamala Devi, C.S. 2008. Chemopreventive and therapeutic modulation of green
tea polyphenols on drug metabolizing enzymes in 4-Nitroquinoline 1-oxide
induced oral cancer. Chem Biol Interact. 172, 224-234.
Tian, J., Lin, X., Guan, R., Xu, J. G. 2004. The effects of hydroxyethyl starch on lung
capillary permeability in endotoxic rats and possible mechanisms. Anesth Analg
98, 768-774.
Tsvetkov, P., Asher, G., Reiss, V., Shaul, Y., Sachs, L., Lotem, J. 2005. Inhibition of
22
NAD(P)H:quinone oxidoreductase 1 activity and induction of p53 degradation by
the natural phenolic compound curcumin. Proc. Natl. Acad. Sci. 15, 5535–5540.
Uehiyama, M., Mihara, M. 1978. Determination of malonaldehyde precursor in tissue
by thiobarbituric acid test. Anal. Biochem. 86, 271–278.
Wu, J.J., Chiang, M.T., Chang, Y.W., Chen, J.Y., Yang, H.T., Lii, C.K., Lin, J.H., Yao, H.
T. 2011. Correlation of Major Components and Radical Scavenging Activity of
Commercial Tea Drinks in Taiwan. J. Food. Drug. Anal. 19, 289-300.
Xu, C., Li, C.Y., Kong, A.N. 2005. Induction of phase I, II and III drug
metabolism/transport by xenobiotics. Arch Pharm Res. 28, 249-268.
Yang, C.S., Chhabra, S.K., Hong, J.Y., Smith, T.J. 2001. Mechanisms of inhibition of
chemical toxicity and carcinogenesis by diallyl sulfide (DAS) and related
compounds from garlic. J. Nutr. 131, 1041S-1045S.
Yang, C.S., Pan, E. 2012. The effects of green tea polyphenols on drug metabolism.
Expert Opin Drug Metab Toxicol. 8, 677-689.
Yao, H.T., Chang, Y.W., Lan, S.J., Yeh, T.K. 2008. The inhibitory effect of tannic acid
on cytochrome P450 enzymes and NADPH-CYP reductase in rat and human liver
microsomes. Food Chem. Toxicol. 46, 645–653.
Yao, H.T., Lin, J.H., Chiang, M.T., Chiang, W., Luo, M.N., Lii, C.K. 2011.
Suppressive effect of the ethanolic extract of adlay bran on cytochrome p-450
enzymes in rat liver and lungs. J. Agric. Food Chem. 8, 4306–4314.
Zheng, Z., Fang, J.L., Lazarus, P. 2002.Glucuronidation: an important mechanism for
detoxification of benzo[a]pyrene metabolites in aerodigestive tract tissues. Drug
Metab. Dispos. 30, 397-403.
23
Acknowledgments
This study was financially supported by grant aid from China Medical University
(CMU99-N1-10), Taiwan.
24
Legends to Figures
Figure 1. Effects of tea beverages on CYP protein expression in rat liver microsomes.
Protein contents were measured by immunoblotting assay. Values are the mean±SD of
n = 6. The protein band was quantified by densitometry, and the level of the control
was set at 1. -Actin was used as an internal control for Western blot.
Figure 2. Effects of tea beverages on GCLc and GCLm protein expression in the liver
and lungs of rats. Protein contents in liver (A) and lung (B) homogenates were
measured by immunoblotting assay. Values are the mean±SD of n = 6. The protein
band was quantified by densitometry, and the level of the control was set at 1. -Actin
was used as an internal control for Western blot.
Figure 3. Effects of tea beverages on PXR, AhR, and Nrf2 DNA-binding activity.
Nuclear extracts of liver homogenate were used to determine Nrf2 (A), AhR (B), and
PXR (C) nuclear protein-DNA binding activity.
25
Table 1. Constituents of green tea (GT) and black tea (BT) beveragesa.
Amount (μg/ml)
GT
BT
Gallic acid (GA)
3.2
24.6
Epigallocatechin (EGC)
201.9
25.0
Epigallocatechin gallate
271.5
59.1
(EGCG)
Epicatechin (EC)
29.2
2.6
Epicatechin gallate (ECG)
32.6
3.7
Gallocatechin gallate (GCG)
49
1.8
Total catechinsb
587.4
116.8
Caffeine
179.7
208.3
Ascorbic acid
21.1
6.0
Total phenolicsc
(gallic acid Eq/mL)
Sucrose (g/L)
576.6
323.2
65.5
70.2
a
Two bottles of tea from the same batch were pooled and the constituents were then
determined in triplicate. Values are expressed as the mean of two batches of tea
beverages.
b
c
Total catechins=EGC+EGC+ECG+EGCG+GCG.
The total phenol content of the tea beverages is expressed as μg of gallic acid
equiv/mL of tea.
26
Table 2. The activities of drug-metabolizing enzymes in the liver microsomes a
Groups
Control
GT
BT
Cytochrome P450 (pmol/mg protein)
665.557.8
608.2 114.2
735.2 142.5
Cytochrome b5 (pmol/mg protein)
227.073.2 a
180.367.4 ab
137.152.3b
NADPH-cytochrome P450 reductase (mol/min/mg protein)
281.239.7
298.615.0
318.560.5
1272.8508.0a
483.5 141.7b
427.0101.6b
Midazolam 1-hydroxylation (CYP3A) (pmol/min/mg protein)
102.325.0 a
58.66.9 b
72.620.3 b
Diclofenac 4-hydroxylation (CYP2C) (pmol/min/mg protein)
119.4 31.0a
95.2 11.8b
74.7 14.0b
p-Nitrophenol 6-hydroxylation (CYP 2E1) (pmol/min/mg protein)
347.8 67.4a
223.1 36.4b
162.825.3c
Lauric acid 12-hydroxylation (CYP4A) (pmol/min/mg protein)
492.0 116.1
376.5 123.1
464.7 167.2
Detromethorphen O-deethylation (CYP2D) (pmol/min/mg protein)
142.523.8
136.956.1
133.6 33.9
Ethoxyresorufin O-deethylation (CYP 1A1) (pmol/min/mg protein)
69.4 12.4b
92.0 11.6a
74.1 11.7b
Methoxyresorufin O-demethylation (CYP 1A2) (pmol/min/mg protein)
32.6 11.8b
88.526.5a
72.5 24.3a
14.16.0
15.75.3
16.27.3
1202.073.1
1272.0220.3
1398.2240.0
Testosterone 6β-hydroxylation (CYP3A) (pmol/min/mg protein)
Pentoxyresorufin O-depentylase (CYP 2B) (pmol/min/mg protein)
Phase II enzyme activities
Glutathione S-transferase (nmol/min/mg protein)
27
UDP-glucuronosyltransferase (nmol/min/mg protein)
NADPH:quinone oxidoreductase 1 (nmol/min/mg protein)
a
22.22.8b
27.2 2.1a
31.24.5 a
117.666.8
122.047.3
183.963.5
Values are the mean SD of n = 6. Values in the same row with different letters differ significantly (p < 0.05).
28
Table 3. The activities of drug-metabolizing enzymes in the lung microsomes a
Groups
Control
GT
BT
Ethoxyresorufin O-deethylation (CYP 1A1) (pmol/min/mg protein)
3.71.4
6.02.7
6.22.2
Methoxyresorufin O-demethylation (CYP 1A2) (pmol/min/mg protein)
2.40.5
2.30.4
2.40.3
p-Nitrophenol 6-hydroxylation (CYP 2E1) (pmol/min/mg protein)
166.725.8
179.952.6
172.818.8
Glutathione S-transferase (nmol/min/mg protein)
112.47.8a
58.44.0b
57.93.8b
2.70.5c
3.80.6b
4.90.7a
102.715.8
110.917.1
11321
UDP-glucuronosyltransferase (nmol/min/mg protein)
NADPH:quinone oxidoreductase 1 (nmol/min/mg protein)
a
Values are the meanSD of n=6. Values in the same row with different letters differ significantly (p < 0.05).
29
Table 4. The GSH and GSSG contents and the enzyme activities of antioxidant defense system in rat liver and lungsa
Liver
Lungs
Control
GT
BT
Control
GT
BT
GSH (nmol/mg protein)
20.7 2.5b
43.4 10.6a
38.3 6.5a
2.8 1.8b
11.6 1.0a
11.51.9a
GSSG (nmol/mg protein)
0.560.14a
0.070.02b
0.060.02b
0.30.2
0.20.1
0.20.1
GSH/GSSG
36.914.0b
620.0155.7a
638.3213.6a
9.33.6b
58.010.1a
57.52.8a
Glutathione peroxidase (nmol/min/mg
198.125.7b
280.774.0a
216.4 30.4ab
57.36.7
59.5 3.1
56.44.4
67.9 4.5
62.3 5.8
35.13.7a
16.7 2.7c
25.5 3.7b
61.35.7
protein)
Glutathione reductase (nmol/min/mg
protein)
TBARS (nmol/g protein)
47.9±3.4
47.5±7.5
46.8±6.9
232±22.3a
193.8±25.0b
219.6±27.2ab
ROS (nmol/mg protein)
1.51±0.38 a
1.03±0.27 b
1.00±0.28 b
0.67±0.11a
0.52±0.06 b
0.58±0.18 ab
a
Values are the mean SD of n = 6. Values in the same row with different letters differ significantly (p < 0.05).
30
Figure 1.
31
(A)
(B)
Figure 2.
(A)
(B)
32
(C)
Figure 3.
33