Living Well with Psoriatic Arthritis
advertisement
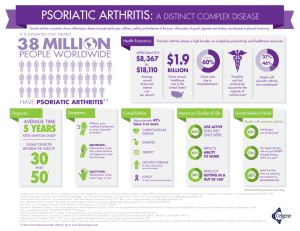
2015 LIVING WELL WITH PSORIATIC ARTHRITIS Presented by: Barry Shibuya, MD Introduction Dr. Barry Shibuya Board certified in Rheumatology, Internal Medicine, and most recently Integrative Medicine Specializes in arthritis, osteoporosis and related autoimmune diseases like lupus and rheumatoid arthritis Washington Hospital (Fremont) Overview of today’s talk • Psoriatic arthritis as a whole-body condition • Holistic medicine approach to psoriatic arthritis • Healthy diet • Safe use of supplements • Exercise: benefits and strategies • Sleep hygiene • Self-care and dealing with stress • Question and answer session Psoriatic arthritis • Psoriatic arthritis is an inflammatory type of arthritis • Causes stiffness, pain and swelling in and around joints; surrounding ligaments and tendons • Can affect any joint in the body, and symptoms vary from person to person • Research has shown that persistent inflammation from psoriatic arthritis can lead to joint damage Psoriatic arthritis and related diseases Individuals with psoriatic arthritis are at an elevated risk to develop other chronic and serious health conditions also known as “comorbidities”, including: • Heart disease • Diabetes • Depression • Metabolic syndrome • Obesity Healthy living with psoriatic arthritis Because psoriatic arthritis is a whole-body condition, a good diseasemanagement plan incorporates: • Treatment • Healthy diet • Regular exercise • Stress reduction • Strong support network Holistic medicine vs. Western medicine • Holistic medicine is a form of healing that considers the whole person -- body, mind, spirit, and emotions -- in the quest for optimal health and wellness • Searching for the underlying causes of disease is preferable to treating symptoms alone • Integrates conventional and alternative therapies to prevent and treat disease • Optimal health is the priority over the absence of sickness Remember • A holistic approach does not replace the need for Western medicine • However, it can aid you in becoming healthier and happier overall, and perhaps lessen the need for pharmaceutical intervention Pharmacologic treatment options for psoriatic arthritis • NSAIDs (Nonsteroidal anti-inflammatory drugs) • Aleve, Celebrex, Motrin, and many others • DMARDs (Disease-modifying antirheumatic drugs) • Methotrexate, sulfasalazine, Arava (leflunomide) • Biologic agents (also DMARDs) • Enbrel, Humira, Remicade, Simponi, Stelara • Other treatment options • Otezla, surgery, physical therapy Benefits of early intervention • • • • Improve skin disease and joint function Minimize disease progression Ease pain and swelling Lower risk of developing comorbid conditions • Better health outcomes overall Tips to improve psoriatic disease Ongoing care means: • See your health care provider • Take medications as prescribed • Regular blood screenings • Make lifestyle changes See your health care provider • Visit your health care provider / team as prescribed • Work with your health care provider to find the best treatment options for you Regular blood screenings Visit your primary care provider regularly to check: • Blood count levels • Blood pressure • Blood sugar • Cholesterol Psoriatic arthritis and diet • No diet is scientifically proven to lessen symptoms of psoriasis or arthritis • NPF Medical Board recommends eating a healthy, balanced diet: • Variety of fruits and vegetables • Whole grains • Lean meats • Low-fat dairy products • Limited alcohol • Healthy fats Whole foods diet • The standard American diet often includes too much sugar, white flour, processed foods • Following a whole food diet involves maximizing your nutrient intake from natural sources and avoiding nutrient-poor processed foods • Include plant-based foods • Vegetables, fruits and nuts • Animal foods • Eggs, meat, fish and poultry • A whole food diet can provide you with all of the nutrients you need for optimal health Weight loss diet • Being overweight further compounds your risk for diabetes and heart disease • To help identify what is a healthy weight for you, calculate your body mass index (BMI) • To lose weight, you need to burn more calories than you consume • One pound equals 3,500 calories • If you cut 500 a day from your diet, you will lose a pound a week • People who lose weight slowly are more successful in keeping it off • Can burn additional calories by increasing physical activity Tips for preparing healthy foods • When you feel like cooking, prepare extra to freeze for leftovers so you always have healthy food around • Make sure any frozen entrees and canned soups are low in sodium • Consider pre-cut vegetables and fruits for healthy snack options • Pay close attention to portion size! • The 9-inch “Plate Method” consisting of: • • • Half vegetables Quarter protein Quarter starch Dietary supplements • Dietary supplements can be extracts or concentrates, and they can occur in many forms, such as tablets, capsules, softgels, gelcaps, liquids or powders • Tell your doctor before taking any OTC supplements • Every substance has a potential to interact with your other medications and treatments Omega-3 fatty acids (fish oil) • Oils of cold water fish are rich in omega-3 fatty acids • Fish accumulate omega-3 fatty acids by consuming either microalgae or prey fish • There are three types of omega-3 fatty acids: • Alpha-linolenic acid • Eicosapentaenoic acid (EPA) • Docosahexaenoic acid (DHA) • Fish oil appears to reduce inflammation in the body • Used in many contexts, including: • Conditions related to the heart and blood system • To lower blood pressure or triglyceride levels • Preventing heart disease or stroke Food sources of omega-3 fatty acids • Alpha-linolenic acid can be found in: • Some vegetable oils • Nuts, seeds • Flax seeds, chia seeds • Soy foods • EPA and DHA: • Found in fatty fish and algae • Salmon, herring, mackerel, anchovies, and sardines Vitamin D • “The sunshine vitamin” • Helps maintain healthy bones • Assists with absorption and distribution of calcium in the body • Speculation that vitamin D can help with aspects of health • The prevention of cancer- this needs to be further elucidated however • Maintenance of a normal and effective immune system • Possibly with certain autoimmune diseases like multiple sclerosis • Vitamin D can change the way cells grow Food sources of Vitamin D • • • • • • • • • • Cod liver oil Salmon (sockeye) Mackerel Tuna fish canned in water Milk, non-fat, reduced-fat, and whole, vitamin D-fortified Orange juice fortified with vitamin D Yogurt fortified with 20 percent of the daily value of vitamin D Eggs, vitamin D is found in the yolk Swiss cheese Fortified cereals • Also– sunlight exposure (limited amount) Turmeric (curcumin) • Turmeric, a shrub related to ginger, is grown throughout India, other parts of Asia, and Africa • Turmeric has been used to aid digestion and liver function, relieve arthritis pain, and regulate menstruation • Preliminary findings from animal and other laboratory studies suggest that a chemical found in turmeric—called curcumin—may have anti-inflammatory, anticancer, and antioxidant properties Glucosamine • Glucosamine • Natural chemical compound found in the body • Most often used to try to ease the joint pain caused by arthritis • Helps keep the cartilage in joints healthy • Glucosamine has been shown in some studies to help ease the pain of mild to moderate osteoarthritis of the knee • For other types of arthritis/pain, no evidence that glucosamine helps: • sports injuries, temporomandibular joint problems (TMJ), chronic low back pain, etc. Sleep • Sleep is required for most essential body functions • Poor sleep hygiene can lead to poor memory, concentration, problem solving, emotional control, creativity, learning • Tips from National Sleep Foundation: • • • • • • • Avoid napping during the day Avoid stimulants such as caffeine, nicotine, and alcohol too close to bedtime Exercise can promote good sleep Food can be disruptive right before sleep Ensure adequate exposure to natural light Establish a regular relaxing bedtime routine Associate your bed with sleep Exercise • Exercise can make a big difference in quality of life with psoriatic arthritis • Movement keeps joints and tendons looser and limber • Helps reduce the inflammation and pain of psoriatic arthritis • Building up muscles decreases the workload on joints • Exercise can help lower the risk of developing a comorbid condition Vicious Cycle Pain Fatigue Lack of exercise Psoriatic Arthritis Inactivity Stiffness Exercise and fatigue • Studies demonstrate that even small amounts of exercise, as little as 6 minutes per day, can lessen pain and fatigue • Regular exercise can increase energy levels • Even among people suffering from medical conditions like cancer and heart disease • Researchers believe that putting forth more energy into regular exercise may provide increased energy in the long run Exercise and mood • Exercise can also help reduce anxiety and improve mood • Exercise may help ease depression in a number of ways, including: • Releasing feel-good brain chemicals that may ease depression (neurotransmitters and endorphins) • Reducing immune system chemicals that can worsen depression • Increasing body temperature, which may have calming effects Exercise: getting started • • • • Consult your doctor to determine what is appropriate for you Stretch out. Your workout should include 15 minutes of flexibility exercises Build muscles by using weights or resistance Find a buddy. Consider exercising in a group or with a friend to help you stick with your regimen • Make it fun. Start slow and focus on activities that you find enjoyable Types of exercise • Cardiovascular Exercise • Strength Training • Flexibility Cardiovascular exercise • • • • High vs. low impact activities 30-40 minutes of moderate-intensity aerobic activity Four to five days per week Examples: brisk walking, cycling, swimming Strength training • Increase muscle strength surrounding joints • Stability at joints • Muscle-strengthening activities on 2 or more days a week that work all major muscle groups • Examples: free weights and resistance bands Flexibility • Increases ROM at a joint • Decreases soft tissue tightness • Prevents stiffness • Can be done on a daily basis Alternatives to regular exercise routine • Aquatic therapy • Tai Chi • Pilates and Yoga Aquatic therapy • Facilitates muscle relaxation and increases circulation • Water provides resistance for strength training • Stimulates body awareness, balance, and trunk stability • Warm water and buoyancy results in decreased pain sensitivity Tai Chi • • • • • Mental and spiritual aspects combined with movement “Meditation in motion” Low impact activity Increases balance and decreases falls risk Helps to improve muscle strength, flexibility, balance, and aerobic conditioning • Has demonstrated benefit for conditions including: • • • • • • • • Arthritis Low bone density Breast cancer Heart disease Heart failure Hypertension Parkinson’s disease Stroke Yoga and Pilates • Combines controlled breathing, stretching and strengthening exercises, and meditation to help control stress and improve blood flow • Can help build core strength, ease joint pain and improve range of motion • Practice yoga poses at least 15 to 20 minutes a day Stay motivated • Set realistic goals • Do activities you enjoy • Try and work exercise into your daily life/routine Modalities for pain • Ice vs. heat • Heat is best for painful joints, helps decrease joint stiffness • Cold is best for warm swollen joints, helps decrease pain with swollen joints • Massage • Massage can lower the body’s production of the stress hormone cortisol • Boost production of serotonin • Lower production of the neurotransmitter substance P, often linked to pain, and improve sleep as a result Relief for pain and swelling in feet • Find the right footwear: shoes with a high toe box and/or heel cups can help • Your insurance plan may cover specialized shoes or orthotic inserts • A podiatrist can fit you with footwear specially made for you and provide other solutions Adaptive tools • Number of tools available to help manipulate small objects and/or perform repetitive motions • Assistive devices help reduce stress on joints. Devices include arthritic grip canes, crutches, walkers, etc. • For more information talk with your doctor, pharmacist, physical or occupational therapist, or the Job Accommodation Network for Assistance Stress • Stress is linked to the 6 leading causes of death: • Heart disease • Cancer • Lung ailments • Accidents • Liver cirrhosis • Suicide • 43% of all adults suffer adverse health effects from stress • 2/3 office visits to family physicians are due to stress-related symptoms Signs of stress • • Poor judgment • Pessimistic attitude • Anxiety and worry • Moodiness and irritability • Agitation, inability to relax • Loneliness and isolation • Feeling overwhelmed, depressed and unhappy • Aches and pains • • Concentration and memory problems • • • • • • • • Diarrhea or constipation Nausea, dizziness Chest pain, rapid heartbeat Loss of libido Frequent colds Eating more or less Sleeping more or less Procrastinating Use of alcohol, cigarettes, or drugs to relax Increase in “nervous habits” like nail biting or pacing Self-perpetuating properties of stress • Stress increases unhealthy behaviors • • • • • Eat comfort foods Smoke and drink alcohol more Become more sedentary Get less sleep Less compliant with using medications • Stress also increases negative thinking The role of expectations • When we don’t meet our expectations, we aren’t just unhappy, we feel a danger or threat • Important to understand what you control and what you don’t control • Avoid “All or nothing” thinking, be realistic and reasonable • I’ll get a job right away • I’ll never get a job The role of expectations • Don’t set expectations too low, that’s a recipe for feeling bad about yourself • Aim for • low expectations for things out of your control • realistic expectations of things we have some control over • high expectations of ourselves • Expect the unexpected Self-appraisals are important • • • • Normal to compare ourselves to others How you compare yourself is important You are not better, they are not better Everyone has their strengths Reducing stress for people with psoriatic arthritis • • • • • • Find a doctor you trust Get better treatments/be proactive Acknowledge your feelings Talk to a friend or counselor Educate yourself See a psychologist • Don’t be afraid to ask for help • Set limits • Learn to say “no” • Spend time in nature Relaxation, meditation, prayer Social support • • • • National Psoriasis Foundation Team NPF events Psoriasis One to One program Volunteer Online presence Comment on blogs Read and post on forums Start your own blog • Don’t assume people will be put off by requests for help. People generally like to help, feel useful, and be needed Take-home points How we think about a situation is important • Avoid catastrophic thinking • Avoid all-or-nothing thinking • Focus on positive aspects What we think How we feel What we do Stress: what you can do • • • • • Identify your stressors Eliminate what you can Reduce exposure Say “No” to new obligations Figure out how your appraisals may be contributing to how much stress you feel • Incorporate stress reduction techniques • Treat your psoriasis and psoriatic arthritis! Question & answer session