Pituitary and Adrenal Gland Dysfunction
advertisement
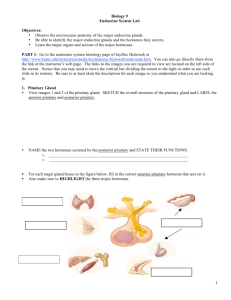
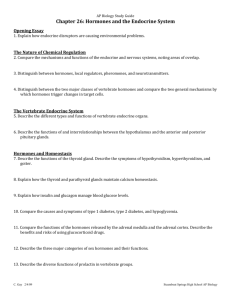
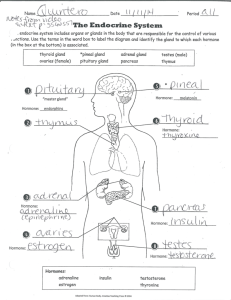
Chapter 19 Care of Patients with Pituitary and Adrenal Gland Problems Disorders of the Anterior Pituitary Gland Target tissue Thyroid, adrenal cortex, ovary, testes, uterus, mammary glands and kidney Either excess or deficiency Pathologic condition within the gland or hypothalmic dysfunction Two to focus on: Hyperpituitarism Hypopituitarism Anterior Pituitary Gland Hyper-secretion and or secretion Pituitary Tumor Pituitary hyperplasia Benign adenoma (most common) Pressure on the optic nerve Excess GH, ACTH, prolactin (PRL) or TSH Hypopituitarism Deficiency of one or more anterior pituitary hormones results in metabolic problems and sexual dysfunction. Panhypopituitarism—decreased production of all of the anterior pituitary hormones. Most life-threatening deficiencies—ACTH and TSH. Deficiency of gonadotropins. Growth hormone Proportionate dwarfism Cause of Hypopituitarism Benign or malignant tumors Anorexia nervosa Shock or severe hypotension Head trauma Brain tumors or infection Congenital Patient-Centered Collaborative Care Assessment Interventions include: Replacement of deficient hormones Androgen therapy for virilization; gynecomastia can occur Estrogens and progesterone Growth hormone Hyperpituitarism Hormone oversecretion occurs with pituitary tumors or hyperplasia Genetic considerations Pituitary adenoma Gigantism Gigantism is the onset of growth hormone hypersecretion before puberty. Acromegaly Growth hormone hypersecretion after puberty Surgical Intervention Transsphenoidal or transfrontal removal of the pituitary gland http://www.youtube.com/watch?v=Ebhf1qKVA9A Patient-Centered Collaborative Care Assessment Nonsurgical management: Drug therapy- to reduce GH secretion or the effects on tissues Somatostatin analogues Dopamine agonists Growth hormone antagonist Radiation Gamma knife procedure Usually one time treatment Surgical Management Postoperative Care Monitor neurologic response Assess for postnasal drip HOB elevated Assess nasal drainage Avoid coughing early after surgery Assess for meningitis Hormone replacement Avoid bending Avoid strain at stool Postoperative Care Avoid toothbrushing Numbness in the area of the incision Decreased sense of smell Vasopressin Diabetes Insipidus Water metabolism problem caused by an antidiuretic hormone deficiency (either a decrease in ADH synthesis or an inability of the kidneys to respond to ADH) Diabetes insipidus is classified as: Nephrogenic Neurogenic Patient-Centered Collaborative Care Assessment Most manifestations of DI are related to dehydration Increase in frequency of urination and excessive thirst Dehydration and hypertonic saline tests used for diagnosis of the disorder Urine diluted with a low specific gravity (<1.005) DI: Interventions Oral chlorpropamide Desmopressin acetate Early detection of dehydration and maintenance of adequate hydration Lifelong vasopressin therapy for patients with permanent condition of diabetes insipidus Teach patients to weigh themselves daily to identify weight gain Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) Vasopressin is secreted even when plasma osmolarity is low or normal. Feedback mechanisms do not function properly. Water is retained, resulting in hyponatremia (decreased serum sodium level). SIADH: Patient-Centered Collaborative Care Assessment: Recent head trauma Cerebrovascular disease Tuberculosis or other pulmonary disease Cancer All past and current drug use SIADH: Interventions Fluid restriction Drug therapy—diuretics, hypertonic saline, demeclocycline Monitor for fluid overload Safe environment Neurologic assessment Adrenal Gland Hypofunction Adrenocortical steroids may decrease as a result of inadequate secretion of ACTH Dysfunction of the hypothalamic-pituitary control mechanism Direct dysfunction of adrenal tissue Effect of Insufficiency of Adrenocortical Steroids Loss of aldosterone and cortical action Decreased gluconeogenesis Depletion of liver and muscle glycogen Hypoglycemia Reduced urea nitrogen excretion Anorexia and weight loss Potassium, sodium, and water imbalances Addison’s Disease Primary Secondary: Sudden cessation of long-term high-dose glucocorticoid therapy Acute Adrenal Insufficiency/Addisonian Crisis Life-threatening event in which the need for cortisol and aldosterone is greater than the available supply Usually occurs in a response to a stressful event Patient-Centered Collaborative Care Assessment Clinical manifestations Assessment Psychosocial assessment Laboratory tests Imaging assessment Adrenal Gland Hyperfunction Hypersecretion by the adrenal cortex results in Cushing’s syndrome/disease, hypercortisolism, or excessive androgen production Pheochromocytoma Hyperstimulation of the adrenal medulla caused by a tumor Excessive secretion of catecholamines Hypercortisolism (Cushing’s Disease) Etiology Incidence/prevalence Patient-centered collaborative care Assessment: Clinical manifestations—skin changes, cardiac changes, musculoskeletal changes, glucose metabolism, immune changes Hypercortisolism Cushing’s Disease Psychosocial assessment Laboratory tests—blood, salivary and urine cortisol levels Imaging assessment Hypercortisolism: Nonsurgical Management Patient safety Drug therapy Nutrition therapy Monitoring Hypercortisolism: Surgical Management Hypophysectomy Adrenalectomy Community-Based Care Home care management Health teaching Health care resources Hyperaldosteronism Increased secretion of aldosterone results in mineralocorticoid excess. Primary hyperaldosteronism (Conn's syndrome) is a result of excessive secretion of aldosterone from one or both adrenal glands. Patient-Centered Collaborative Care Assessment Most common issues—hypokalemia and elevated blood pressure Interventions Adrenalectomy Drug therapy Glucocorticoid replacement When surgery cannot be performed—spironolactone therapy Pheochromocytoma Catecholamine-producing tumors that arise in the adrenal medulla Tumors produce, store, and release epinephrine and norepinephrine Patient-Centered Collaborative Care Assessment Interventions: Surgery is main treatment. After surgery, assess blood pressure.