Question 3 - Ipswich-Year2-Med-PBL-Gp-2
advertisement
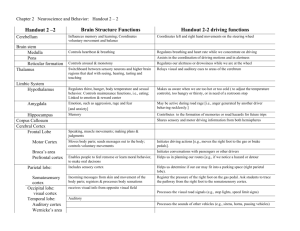
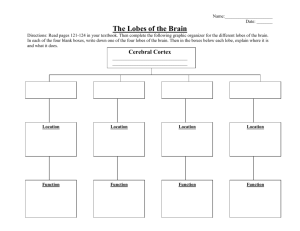
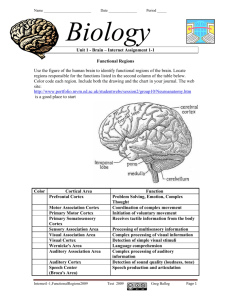
Case 3 Hx & Examination • PC: sudden speech difficulty & right sided weakness • Alert & attentive. • PMH hypertension (BP 172/86), ex smoker and heavy Eth drinker • Comprehends simple commands • speech difficulty (fluency, naming, repetition) • Right lower facial droop • weakness of the right arm and leg What is the likely diagnosis and areas of the brain affected? •Left MCA stroke (embolus, thrombus, haemorrhage) is the probability diagnosis BROCA'S AREA WERNICKE'S AREA MOTOR CORTEX SENSORY CORTEX Expressive speech area. Integration with other language areas. Receptive speech area. Integration with other language areas. Movement of right head and neck, movement of right arm and possibly right leg Sensation from right head and neck, sensation from right arm. Stroke Mimics • A study of more than 400 patients initially diagnosed as stroke, 19% were found to have mimics: • unrecognized seizures with postictal deficits (17% of mimics). Most of these patients had postictal confusion or stupor but transient focal neurological signs were observed in about half of the patients including hemiparesis (Todd’s paralysis), monoparesis, abnormalities of extraocular movements, or hemisensory deficits. • systemic infections (17%), delerium • hemiplegic migraine: unilateral hemiparesis outlasts the headache. • brain tumor (15%) - a review of patients with brain tumors presenting to an ED showed that 6% of patients had symptoms that were of less than one day’s duration; it was thought that these patients with brief symptom duration might reflect a subpopulation who suffer acute deterioration from hemorrhage into the tumor or who develop obstructive hydrocephalus. • toxic-metabolic disturbances (13%) – hypo natremia/glycemia • Conversion Disorder: psychiatric, loss of body functions • Libman RB, Wirkowski E, Alvir J, Rao TH. Conditions that mimic stroke in the emergency department. Implications for acute stroke trials. Arch Neurol. 1995;52:1119-1122 What is the best next diagnostic step? What other investigations are warranted? • Next best diagnostic step – – – – – – Exclude head trauma (inspect, feel) ECG to identify arrhythmias (esp. AF) & CHF CXR CT (CT angiography) MRI (Diffusion Weighted shows infarction within minutes) MRA (magnetic resonance angiogram) to determine if cause is vascular in origin • Other investigations – – – – FBC, platelets, PTT, INR U&E’s Glucose urinalysis Q3 What is the best next step in management? • • • • • • IV TPA if thromboembolic stroke < 3hrs Tight glycaemic control with insulin Control BP Control arrhythmia Maintain hydration and renal function Stockings or pneumatic boots plus heparin to prevent pulmonary embolism • Plan and begin rehab (speech, physio, diet) Define Ischaemic stroke, Transient ischaemic attack & Haemorrhagic stroke (Intracerebral haemorrhage). Can these be distinguished on clinical grounds? • A stroke has 4 elements. They are – – – – Abrupt Focal Rapidly progressing Irreversible neuronal damage • A stroke is caused by – Embolism: deficits appear instantaneously (AF, HF, IE, PFO) – Thrombus: deficits evolve minutes to days – Haemorrhage: Intracerebral & sub-arachnoid: deficits are static or progress over hrs • A TIA is an abrupt, focal transient loss (< 1-2 hrs – Murtagh says < 24 hours but “wtf”) of brain function which doesn’t result in neuronal necrosis. • They cannot be distinguished on clinical grounds Review and present the vascular supply of the brain. How would lesions in the anterior circulation and posterior circulation present? ACA MOTOR CORTEX (Lower Limb) SENSORY CORTEX (Lower Limb) SUPPLEMENTAL MOTOR AREA (Dominant Hemisphere) PREFRONTAL CORTEX Controls movement of the contralateral lower limb. Receives sensory input from the contralateral lower limb Functions with Broca’s area in the initiation of speech. Functions in volition, motivation, and planning and organizing of complex behaviour. •Left ACA: Right leg upper-motor neuron weakness due to damage to motor cortex and right leg cortical sensory loss due to damage to sensory cortex. Grasp reflex, frontal lobe behavioural abnormalities, and transcortical aphasia can also be seen if the prefrontal cortex and supplemental motor areas are involved. •Right ACA: Left leg upper-motor neuron weakness due to damage to motor cortex and left leg cortical type sensory loss due to damage to sensory cortex. Grasp reflex, frontal lobe behavioural abnormalities and left hemineglect can also be seen if the prefrontal cortex and non-dominant association cortex are involved PCA Superficial Branch Occipital Lobe Corpus Callosum Primary and secondary visual areas. Functions in the sensation and interpretation of visual input.. Primary and secondary visual areas. Functions in the sensation and interpretation of visual input. Inferior Branch Thalamus Relay centre for descending and ascending information Internal Capsule Descending fibres of the lateral and ventral corticospinal tracts •Left PCA: Right homonymous hemianopia due to damage to left visual cortex in the occipital lobe. Extension to the splenium of the corpus callosum therefore interfering with communication between the two visual association areas can cause alexia without agraphia. Larger infarcts involving the internal capsule and thalamus may cause right hemisensory loss and right hemiparesis due to disruption of the ascending and descending information passing through these structures. •Right PCA: Left homonymous hemianopia due to damage to right visual cortex in the occipital lobe. Larger infarcts involving the internal capsule and thalamus may cause left hemisensory loss and left hemiparesis due to disruption of the ascending and descending information passing through these structures. Carotid & Vertebrobasilar