Current Medical Issues – Power Point Presentation
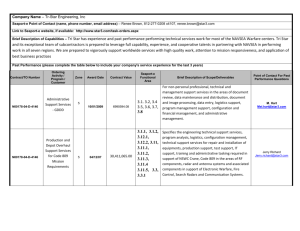
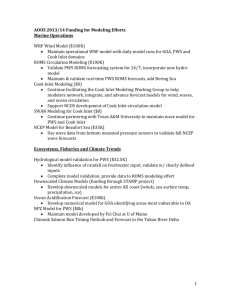
advertisement

Update on Medical Issues in Prader-Willi Syndrome June 17, 2009 NM PWS Gathering Carol Clericuzio, MD Medical Genetics and Pediatrics Medical Advisor New Mexico Prader-Willi Syndrome Project Outline for Today’s Discussion • Brief overview of cause and diagnosis of PWS • Sleep disorders in PWS • Growth hormone therapy in PWS • Adrenal gland problems in PWS • Questions! Prader-Willi Syndrome • 1/15,000 births • Neonatal hypotonia and cryptorchidism • Hypothalamic dysfunction: lack of satiety and subsequent obesity; low sex hormones and growth hormone; some with adrenal insufficiency • Cognitive and behavioral differences • Cause is lack of expression of paternal genes at 15q11-13 Prader-Willi syndrome is due to lack of expression of paternal genes at 15q11-13 Prader-Willi Syndrome at Different Ages Infancy: hypotonia, feeding problems, cryptorchidism, apnea, check adrenals Childhood: obesity, apnea oppositional behaviors, learning problems, short stature Rx GH and thyroid, check adrenals Adulthood: type 2 DM, obstructive sleep apnea, hypogonadism Rx hormone replacement Sleep Disorders in PWS Key Abnormalities of Sleep and Arousal in Prader-Willi Syndrome Main feature Associated features • Excessive daytime sleepiness Increased nocturnal sleep Behavioral problems Issues related to learning and safety • Abnormalities of arousal Reduced arousal to hypoxic and hypercapnic stimuli during sleep • Sleep-disordered breathing Obstructive sleep apnea Sleep-related hypoxemia Hypoventilation Reduced ventilatory response to hypoxia and hypercapnia Sleep and Breathing in Prader-Willi Syndrome Nixon and Brouillette. Pediatric Pulmonology 34:209–217 (2002) What is Sleep Apnea? • Abnormally long pauses in airflow during sleep • Obstructive sleep apnea: pause in breathing due to blockage in the air passages; physical block to airflow despite respiratory effort for 2 or more breaths • Central sleep apnea: pause in breathing due to the brain not telling the body to breathe; lack of respiratory effort for 20 seconds • Complex sleep apnea: a combination of central and obstructive sleep apnea Sleep Apnea in PWS • Sleep apnea is diagnosed with an overnight sleep test called a polysomnogram, or a "Sleep Study". • PWS individuals may have any type, but most often obstructive sleep apnea • Treatment of obstructive sleep apnea may be adenoidectomy, tonsillectomy, oxygen and/or CPAP CPAP Short for "continuous positive airway pressure" • Positive airway pressure therapy is the most effective noninvasive treatment for Obstructive Sleep Apnea (OSA) How does CPAP therapy work? • Air is pushed from the flow generator through the tubing and mask, the air then passes through the nose and into the throat, where the slight pressure keeps the upper airway open. • The low air pressure does not interfere with breathing - though some people need a few nights to get used to the sensation of positive airflow. GeneReviews: Prader-Willi Syndrome • Regardless of age, evaluate respiratory status and perform a sleep study. These studies are specifically recommended prior to initiation of growth hormone therapy, along with assessment of the size of tonsils and adenoids, particularly in the obese individual. • Cassidy and Schwartz Updated March 24, 2008 webpage www.genetests.org Growth Hormone in PWS PWS: Problems with the Hypothalamus • Body thermostat • Regulation of food intake • Controls endocrine system – Growth hormone releasing factor – Corticotropin releasing factor (adrenal gland) – Pubertal hormone releasing factors – Thyrotropin releasing factor (thyroid gland) GeneReviews: Prader-Willi Syndrome • Data from at least 15 studies involving more than 300 affected children (reviewed in Burman et al 2001) document reduced growth hormone secretion in PWS. Growth hormone deficiency is also seen in adults with PWS [Grugni et al 2006, Hoybye 2007] • Cassidy and Schwartz Updated March 24, 2008 webpage www.genetests.org GH therapy in PWS • A rational therapy to improve body composition, growth, strength • Approved by the FDA 2000: Those with PWS only need to show signs of growth failure and have a genetic diagnosis of PWS to qualify for GH treatment under this special Orphan Drug Act approval. (PWSA website 6/10/09) GH improves final adult height in children with PWS • 2007 US retrospective review of 21 children with confirmed GH deficiency compared with 39 non-GH treated adults who had similar early childhood heights • Conclusion: administration of GH to PWS children restores linear growth and adult height without significant effects other than premature adrenarche Angulo et al., AMJG 143A:1456-61 (2007) Concerns with GH therapy in PWS • Sudden death in children with PWS treated with GH has been reported, and a possible contribution of GH to these events has not been definitively excluded. One possible factor is the development or worsening of obstructive sleep apnea. • PWSA recommends a sleep study before the start of growth hormone (GH) on infants, children and adults with Prader-Willi syndrome, and then a follow up study 6-8 weeks later. If there is worsening of obstructive sleep apnea (OSA) on GH temporarily stopping the GH is recommended until the cause is understood. Frequently the OSA can be corrected by removing the adenoids and tonsils or lowering the dose of GH. We also recommend taking precautions during bouts of upper respiratory infections. Does GH Improve Body Composition? • Retrospective study of the potential benefits and adverse events during growth hormone treatment in children with Prader-Willi syndrome Fillion et al., J Pediatr. 2009 Feb;154(2):230-3 • Review of 23 patients with PWS (14 males, 9 females) under age 18 years, 10 of whom (5 males, 5 females) had been treated with GH for periods between 0.1 and 5.5 years • GH therapy in children with PWS in the clinical setting did not lead to any discernible improvement in BMI or body composition • AND it appeared to be associated with OSA • Regardless of GH therapy, parental education was associated with better outcome The Jury is OUT on GH risks/benefits to body composition in PWS • Body mass index in children with Prader-Willi Syndrome during human growth hormone therapy: a real world situation. Dewan and Chanoine J Pediatr. 2009 May;154(5):777-8 • Whether GH affects body mass and composition in patients with PWS in a clinic setting remains unclear and may reflect yet undiscovered individual-specific characteristics. It is, however, important to remind parents that GH is not a cure for obesity and that control of food access and increased physical activity remain the most important factors in obesity control Adrenal Gland Problems in PWS PWS: Problems with the Hypothalamus • Body thermostat • Regulation of food intake • Controls endocrine system – Growth hormone releasing factor – Corticotropin releasing factor (adrenal gland) – Pubertal hormone releasing factors – Thyrotropin releasing factor (thyroid gland) Adrenal Gland Function • Adrenal glands sit on top of the kidneys. They are chiefly responsible for regulating the stress response through the synthesis of cortisol. • Cortisol increases blood pressure and blood sugar, and reduces immune responses • Cortisol deficiency can lead to death if an individual is stressed by surgery, infection, dehydration, etc. Deaths in PWS • Annual death rate is high ~3% • Multiple causes (e.g. choking) but some deaths are unexplained • There are several lines of evidence suggesting that adrenal insufficiency may contribute to unexpected deaths • In 2004 Clericuzio and Stevenson [with the help of NM PWS Project] published a paper on 10 PWS individuals with unexplained death/critical illness and autopsy of 3 infants showed small adrenal glands Two New Adrenal Studies in PWS • 2008: Netherlands physicians studied 25 PWS patients and 60% had adrenal insufficiency – Suggested that hydrocortisone be used during acute illness unless adrenal function studied • 2009: Butler & Garg studied cortisol levels in 63 subjects with PWS and found one of four infants with PWS had a low cortisol level – Recommended PWS infants and children undergo low-dose ACTH stimulation testing before GH treatment or other interventions considered to be stressors Recommendations for PWS patients in stressful situations: e.g. surgery, infections • Our NM pediatric endocrinologists recommend that ALL PWS individuals have a low-dose ACTH stimulation test • Endocrinologist should be consulted prior to elective surgery and in case of acute illness to consider prescribing “stress” doses of replacement cortisol in PWS individuals who have not been tested • Clericuzio and Stevenson recommend that hospitalized PWS patients be monitored closely Most physicians are not aware of risk of adrenal insufficiency in PWS • Studies have not been published in the most widely read pediatric journals • More studies need to be done – including of adults • Physicians can contact me or the Pediatric Endocrinologists • Carol Clericuzio, MD (505) 272-2000 UNM physician access line Questions?