(HRA) with a Claim Data Feed from MVP Health
advertisement

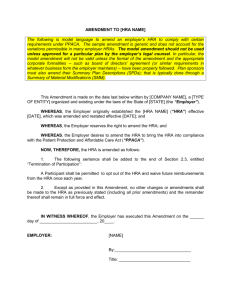
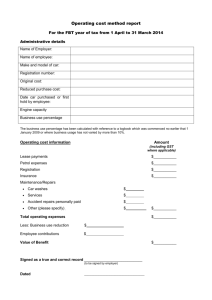
Proposal to Implement for Group Name A Health Reimbursement Arrangement (HRA) with a Claim Data Feed from MVP Health Reimbursement Arrangements - Introduction Health Reimbursement Arrangements (HRAs) are a popular method to help employers control the cost of their health insurance plan while still providing coverage to employees. Typically, an HRA is used in conjunction with a less expensive higher deductible or copay health plan. The higher deductible health care plan provides coverage in the event of a major illness or condition while the HRA provides employees some of the funds necessary to cover routine out of pocket expenses. Features of an HRA HRA utilization is tax deductible to the employer HRA funds are tax-free to the employee Employer can determine fund availability for specific benefits: medical, Rx, dental, vision, etc. Unused funds can roll-over at the employer’s discretion There is no pre-funding requirement – an HRA is a pay as you go plan The Advantages of an HRA Implementation of an HRA with a higher deductible health plan will help reduce costs Creates awareness of the cost of health care Helps to control utilization Provides the employer with a long term health care plan strategy Allows customizable design to meet business needs of employers Overview Choice Strategies is a heath care debit card that can be used for HRA administration. The Choice Strategies is recognized as both a pioneer and leader in debit card administration. We have been implementing and managing HRAs in this unique program since 2001. Choice Strategies debit card and administration service will include: Industry leading service and support The Choice Strategies card for the payment of providers and other vendors Substantiation of card transactions Processing of manually submitted claims Manual claim payments by check or direct deposit Automated reporting functionality Enrollment materials Web site access for employees and employers Plan document production Operation and Functionality of the Choice Strategies Card 1. Submission of Master Application: Installation The first step to implementing Choice Strategies begins with the submission of a Master Application. Once we are in receipt of the Master Application, an installation confirmation is sent to the employer and producing broker. Once installation is complete, employers and brokers receive an email containing contact information, administrative access to the website, plan documents and participant hand outs. 2. The Choice Strategies plan configuration The Choice Strategies plan will be configured based on employer decisions made during the installation process. For example, the employer may choose to allow HRA funds to be used for only medical services or medical and Rx services. MVP Data feed Configurations Choice Strategies has partnered with MVP Healthcare to receive a regularly scheduled data-feed of medical and Rx claim data for all of our members enrolled in an MVP health plan. Essentially, the data-feed provides Choice Strategies with all of the information found on our members’ Explanation of Benefits (EOB) Statements. This direct link with MVP allows us to successfully administer our HRA plans in several unique configurations: Debit-Card Based Plans with Automatic Substantiation For debit card based HRA plans, this condensed claim data allows Choice Strategies to adjudicate many debit card purchases without requiring the member to submit documentation. Standard receipt requests are still sent to members for expenses that are not processed through the health carrier or if the amount paid on the debit card exceeds the member’s responsibility according to the claim data. This configuration works best for clients enrolled in a High Deductible Health Plan (HDHP) and employers who wish to keep their employees involved in the process of managing their health care costs may prefer a debit card based program as well. Member-Pay Plan With Member-Pay HRA plans, Choice Strategies reimburses members automatically from the medical claim data. Employees will not need to submit claims to Choice Strategies. Instead checks and direct deposits will be issued to members directly from the medical claim data-feed. MVP currently sends Rx claim data on a monthly basis offset by 15 days. For example, January Rx expenses will be sent to Choice Strategies around February 15th and processed within 2-3 business days. Medical claim data is sent and processed on a weekly basis. These configurations work well for clients who wish to design an HRA plan that reimburses a portion of each deductible expense. For example, a client may wish the HRA to reimburse medical deductible expenses minus $30, in essence creating co-pays for their employees within the deductible. Similarly, a client may choose to reimburse deductible expenses at 50% or 75%. These “coinsurance” HRA plans work very well on a Member-Pay configuration. Members will not need to submit claims. Instead reimbursements will be made to the members or payments made to the providers automatically every week based on the claim data received from MVP. If Rx is eligible and the HRA covers the full cost of a prescription, we recommend offering the Choice Strategies MasterCard to participants for payment of prescriptions only. Choice Strategies would reimburse medical expenses from the data feed following the parameters elected by the employer while participants could use their Choice Strategies debit cards to pay providers directly with the card. If as an employer you prefer to pay Rx expenses from the MVP claims data feed instead, it is important to note that Choice Strategies receives Rx data from MVP on a monthly basis. 3. Plan Document Production The plan documents will be produced according to the parameters established in the Master Application. These documents include an Adoption Agreement (Outline), a Plan Document (for employer reference), and a Summary Plan Description (to hand out to all participants). All documents are posted in the Administrative Guide under the employer section of our website. 4. Enrollment Process Once we receive the initial enrollment forms or templates, employee accounts are established in our system and welcome brochures are emailed or mailed. Accounts are updated when new enrollments, changes in status or employee terminations are sent to Choice Strategies. 5. Choice Strategies production and distribution Cards will be produced and mailed to each participating employee (and spouse if appropriate). Cards will be mailed to the member’s home address provided on the enrollment form. The card is activated automatically at first use. 6. Web Seminars Employers are invited to attend orientation webinars. During the webinar, the website, reporting tools, the Admin Guide, as well as the administrative procedures and details of the program, are all reviewed. Furthermore, Choice Strategies offers plan specific webinars for employees by appointment. Employers can sign up for web seminars at any time by checking the monthly schedule posted to our website. 7. Member Service All member service calls are handled though our toll free service line. Member Service representatives assist employees with their benefits and are available in English and Spanish. They will assist members to reconcile billing with providers and retrieve required information from carriers. The Member Service department is open from 8:00 AM to 7:00 PM Eastern Time, Monday through Thursday and until 5:00 PM Eastern Time on Friday. You can contact Member Services by phone at 1-888278-2555 ext 2, by email at memberservices@choice-strategies.com, or chat live with a representative by going to our website, www.choice-strategies.com, and selecting the “Live Help” icon. Choice Strategies provides members 24/7 access to account balances through our website. Access to data regarding account information is completely secure. 8. Client Service Each employer is assigned a client service team. Each team works with the employer closely to answer questions regarding the administration of the plan, make plan design changes and provide general consultative guidance. Client Service Representatives are available from 8:00 AM to 5:00 PM Eastern Time, Monday through Friday. 9. Substantiation Process The IRS stipulates that the plan sponsor (employer) ensure that HRA, FSA, DCAP, Transit/Parking plans are properly substantiated. In other words, purchases made with the Choice Strategies debit card must be proven to be eligible under the plan. Choice Strategies substantiates purchases made with the Choice Strategies debit card via the following methods. MVP Data-Feed For debit card based HRA plans, the condensed claim data Choice Strategies receives from MVP allows the adjudication of many debit card purchases without requiring the member to submit documentation. Standard receipt requests are still sent to members for expenses that are not processed through the health carrier or if the amount paid on the debit card exceeds the member’s responsibility according to the claim data. Co-Pay Matching The Choice Strategies debit card can be set to match the co-pay(s) of the underlying plan design. Receipt requests are not generated for transactions in which co-pay have been matched as the expense has been deemed substantiated. IIAS (Inventory Information Approval System) Under this inventory control system merchants such as grocery stores, discount stores, pharmacies, department stores, etc. must be able to differentiate between eligible and ineligible items at the point of purchase. Simply put, the Choice Strategies card only works for eligible prescriptions and OTC medication purchases at participating retailers. Ineligible purchases will be denied at the cash register. This system eliminates the need to request receipts for point of sale pharmacy purchases. Receipt Notification Process Receipt requests are generated and sent weekly to employees for those transactions that cannot be substantiated automatically through any of the above. Employees are requested to provide the necessary documentation (generally EOBs or provider statements) for substantiation. Enforcement of Substantiation Requirements Occasionally a member will disregard our letters or forget to send in requested documentation. To protect employer money, member’s Choice Strategies cards are automatically deactivated in cases in which participants do not send in requested documentation. They are once again reactivated upon receipt of requested documentation. Employers may choose to waive this feature on the Master Application, however, employers should note that in the event of an IRS audit the plan may be found to be non-compliant. 10. Claims payment/ reimbursement process/Direct Deposit If a debit card program is elected by the employer, most transactions will be cardbased and paid to the provider at the time of service through the card transaction. However, some health care and dependent care providers may not accept debit cards for their services. In these cases, reimbursement requests can be submitted with a claim form. These claims will be adjudicated, checks will be cut and mailed to the member or, if preferred, the employee may elect direct deposit. For Direct-Pay programs, claim checks and direct deposits will be issued to the member or provider automatically from the data-feed without requiring members to submit claims. 11. Website: Account Information, Functionality, and Reporting The Choice Strategies card allows website access to both the employee and the employer through at www.choice-strategies.com. Our website also contains a multitude of useful forms, presentations and tools for employers and employees. Employee Online Accounts Features: Account Balances YTD Statements Transaction History Online Claims Submission Upload Requested Documentation Forms and News Employer Online Accounts Employers can access specific account information at any time. The employer has password protected access to: General Account Information Employee Account Status Employee Account Balances Plan Documents Invoices Employer Funding Report – This report must be scheduled for email delivery Enrollee Account Balance Report – This report indicates YTD usage on employer plan(s) Reports are generally scheduled for weekly or monthly delivery but can also be sent with more or less frequency. Additionally, the employer can use the online reporting system to generate other reports on an as needed basis. 12. Administrative Standards Choice Strategies has established administrative standards for our processes. These standards reflect an annual average of our processing times. Standards for seven categories are discussed below. a. Claim Processing Claims are processed daily. Our average turnaround time to process a claim submitted online is 1-3 business days. Our average turnaround time to process a paper claim form is 3-5 business days. Checks are mailed and direct deposits are generated to employee accounts (for submitted claims) daily. b. Member Services Most calls and emails are handled on a real time basis. For those that are not, Choice Strategies responds to member service voice messages generally within two business hours and at most 24 hours of having left a message. If a participant prefers, they can email our Member Service department. Inquiries received via email are usually responded to same day and at most 48 hours. c. Client Services Most calls and emails are handled on a real time basis. For those that are not, Choice Strategies usually responds to employer voicemails and emails on the same day and at most up to 24-48 hours. d. New Card Issuance Cards for new employees of existing clients are usually issued within five business days of the receipt of a completed enrollment form. New groups’ cards are usually issued within four days of receipt of completed enrollment forms and bank settlement. Cards are delivered to the employee’s home generally within 710 business days of the issue date e. Renewals Renewal information is emailed to employer groups approximately 45 days in advance of the plan renewal date. HRA renewals are automatic, meaning only changes to plans or participants need to be communicated to Choice Strategies. f. Billing Invoices are created and sent on or about the first week of each month for that month’s administrative fees. Administrative fee funds are drawn on or about the 13th of the month in which the fees are due. Fees Pricing of Choice Strategies consists of three components. Each is outlined below. The fees are inclusive of HRA debit card administration. Groups with 1 – 99 Employees Initial Setup Fee 1 - 24 employees 25 - 49 employees 50 - 99 employees $250 plus $5 per participating employee $500 plus $5 per participating employee $750 plus $5 per participating employee Monthly Administrative Fee HRA $8.50 per participating employee Renewal Fee $100 plus $5.00 per participating employee HSA Pricing Pricing for an HSA is the same as the above with the exception of the per employee start up fee. For HSAs, the per employee component of the startup is $25. This fee is charged at implementation and each time a new HSA employee is added. Groups with 100+ Employees Contact Sales for custom quote: 888-278-2555 x3 Sales@choice-strategies.com